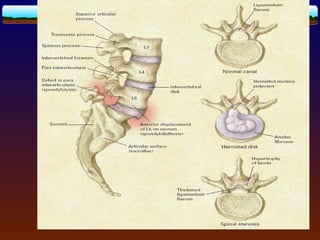
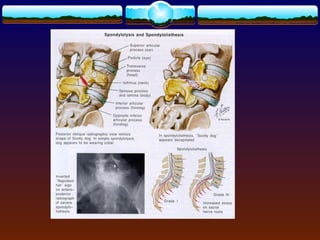
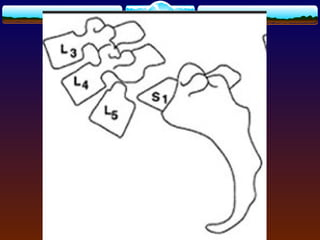
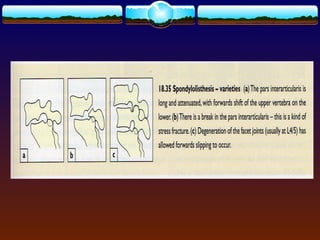
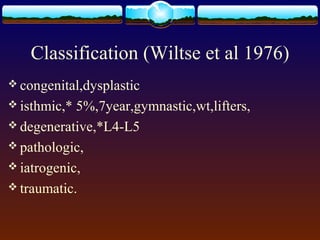
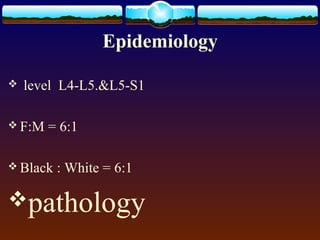
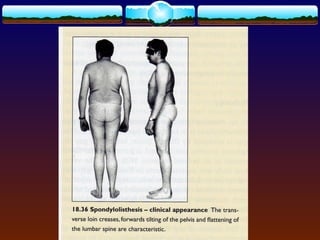
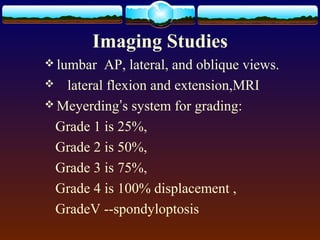
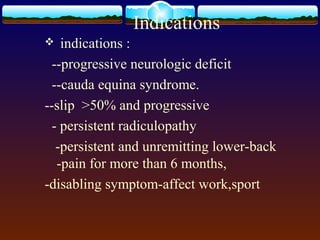
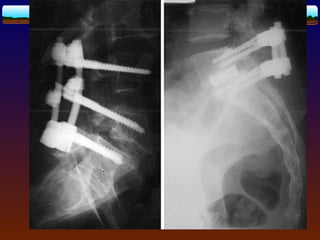
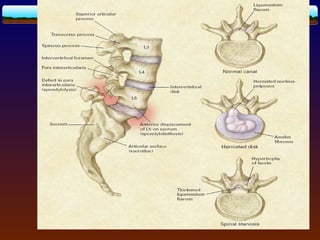
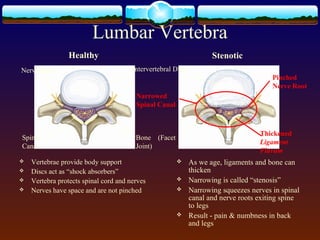
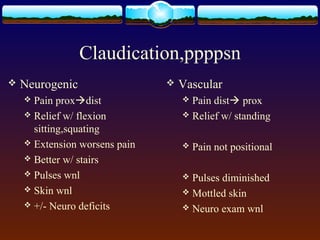
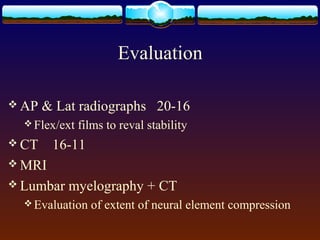
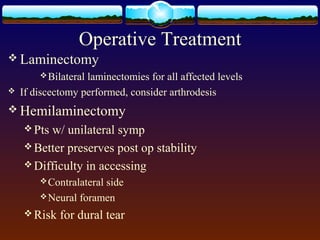
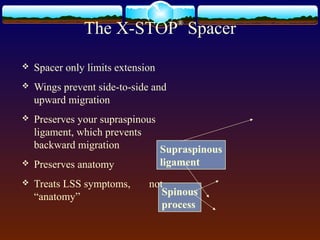
Spondylolisthesis is the slipping of one vertebra over another. It is commonly caused by dysplastic, isthmic, degenerative or traumatic conditions. It most often occurs at the L4-L5 or L5-S1 levels and presents with lower back pain, neurogenic claudication or radiculopathy. Imaging studies can classify and grade the spondylolisthesis. Conservative treatment includes rest, medications and physical therapy while surgical treatment is considered for progressive neurological deficits or severe, persistent pain.