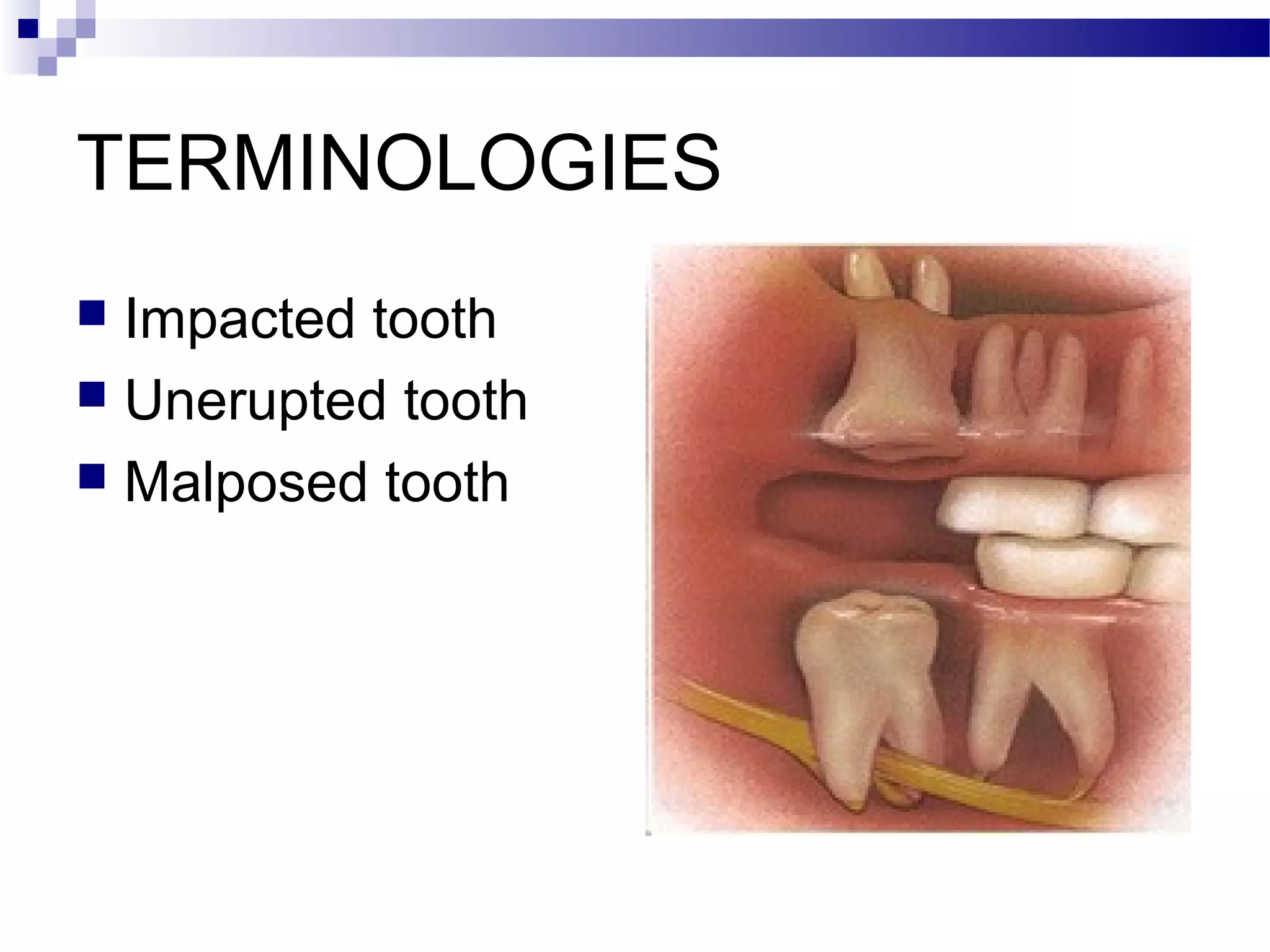
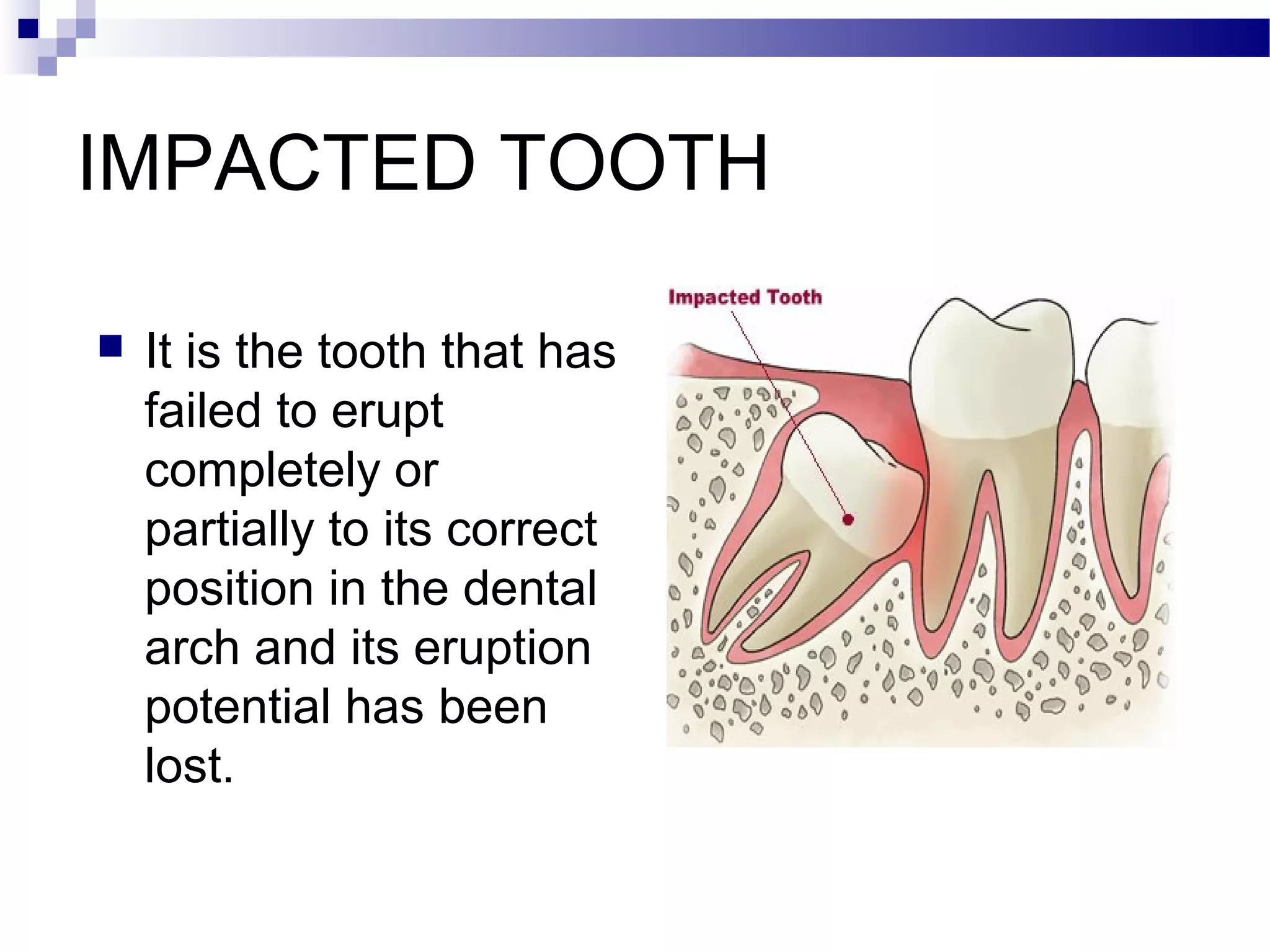
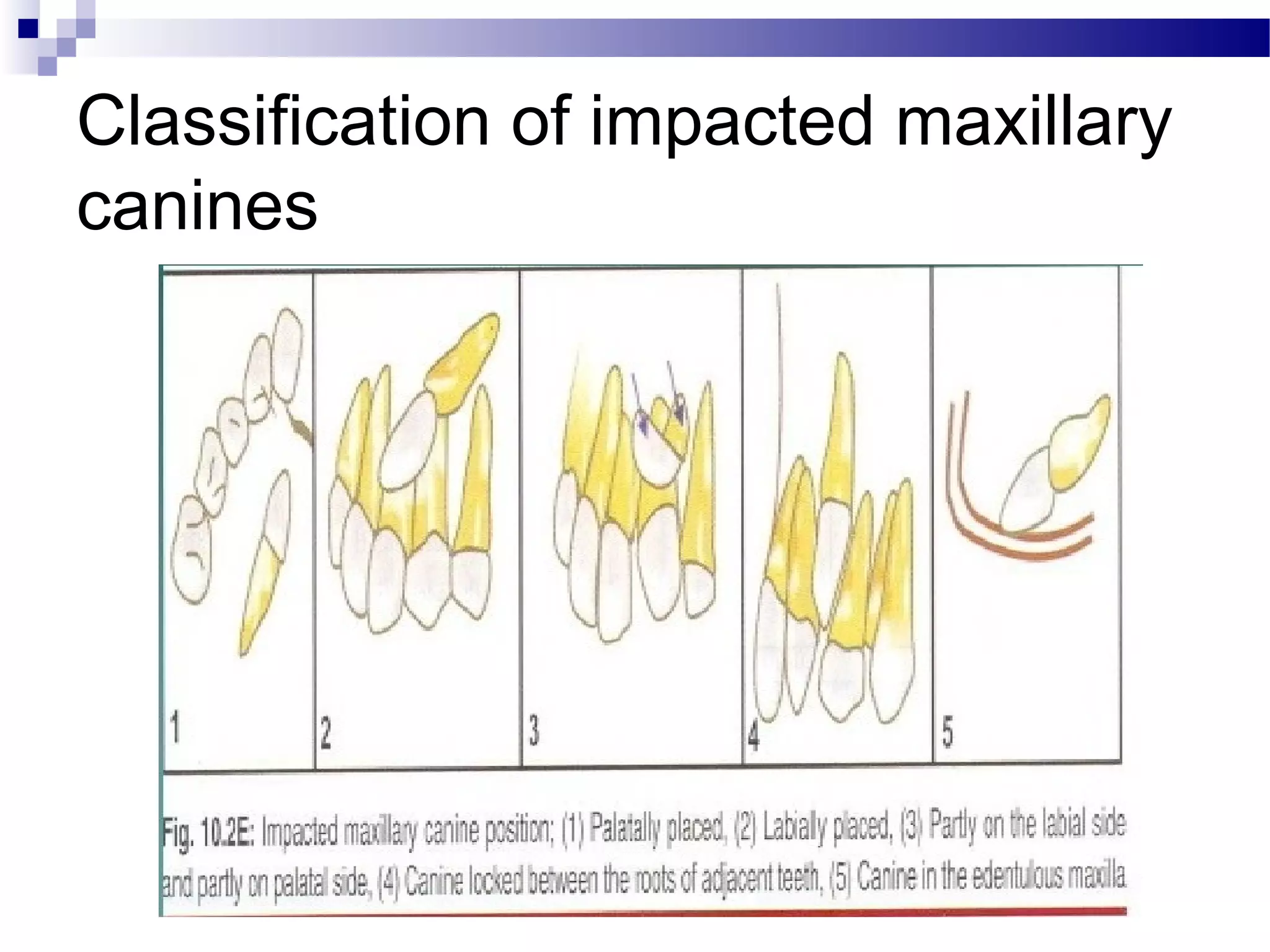
1) The document discusses impacted teeth, which are teeth that fail to fully erupt. It describes common causes and locations of impactions as well as classification systems.
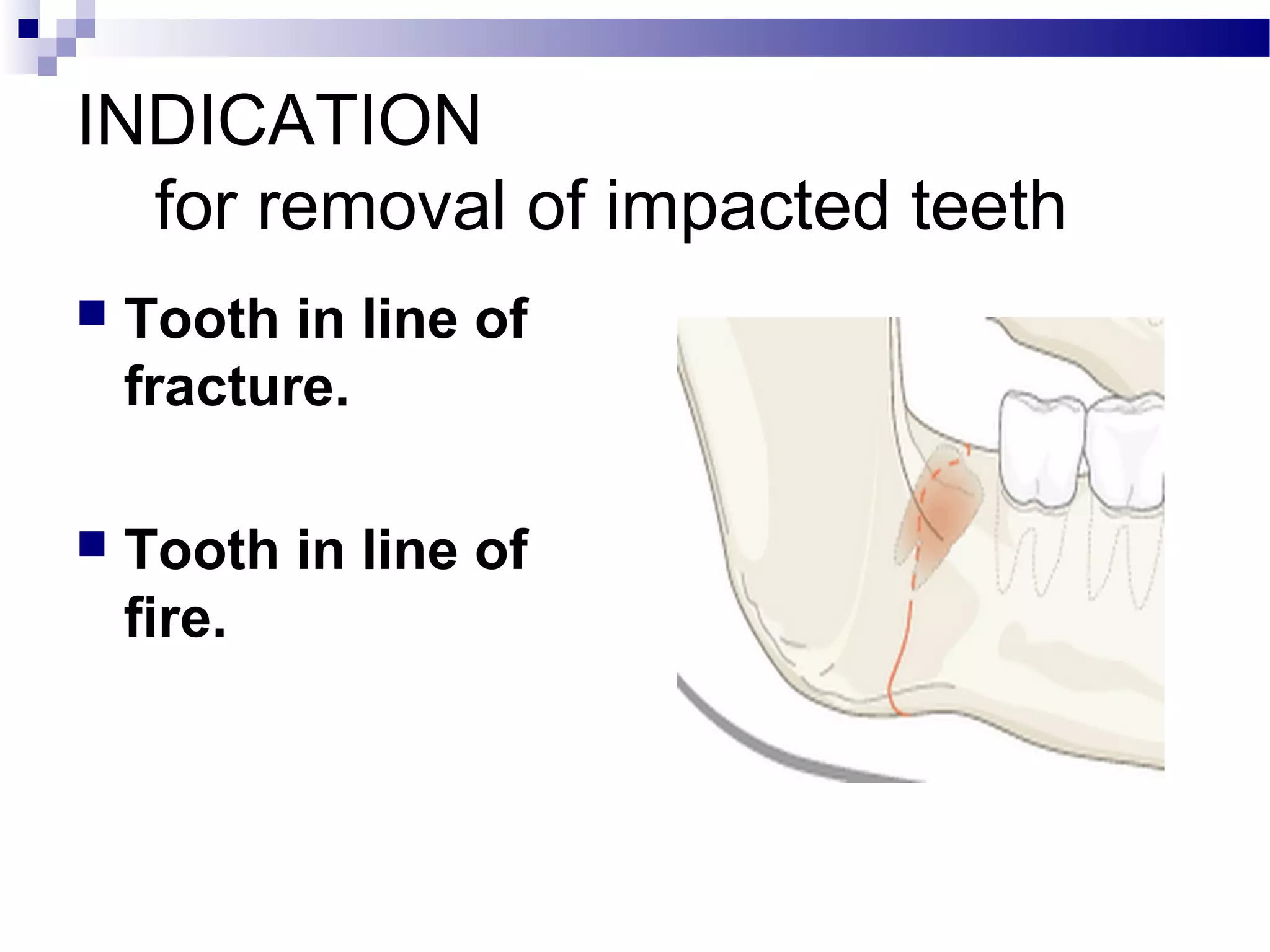
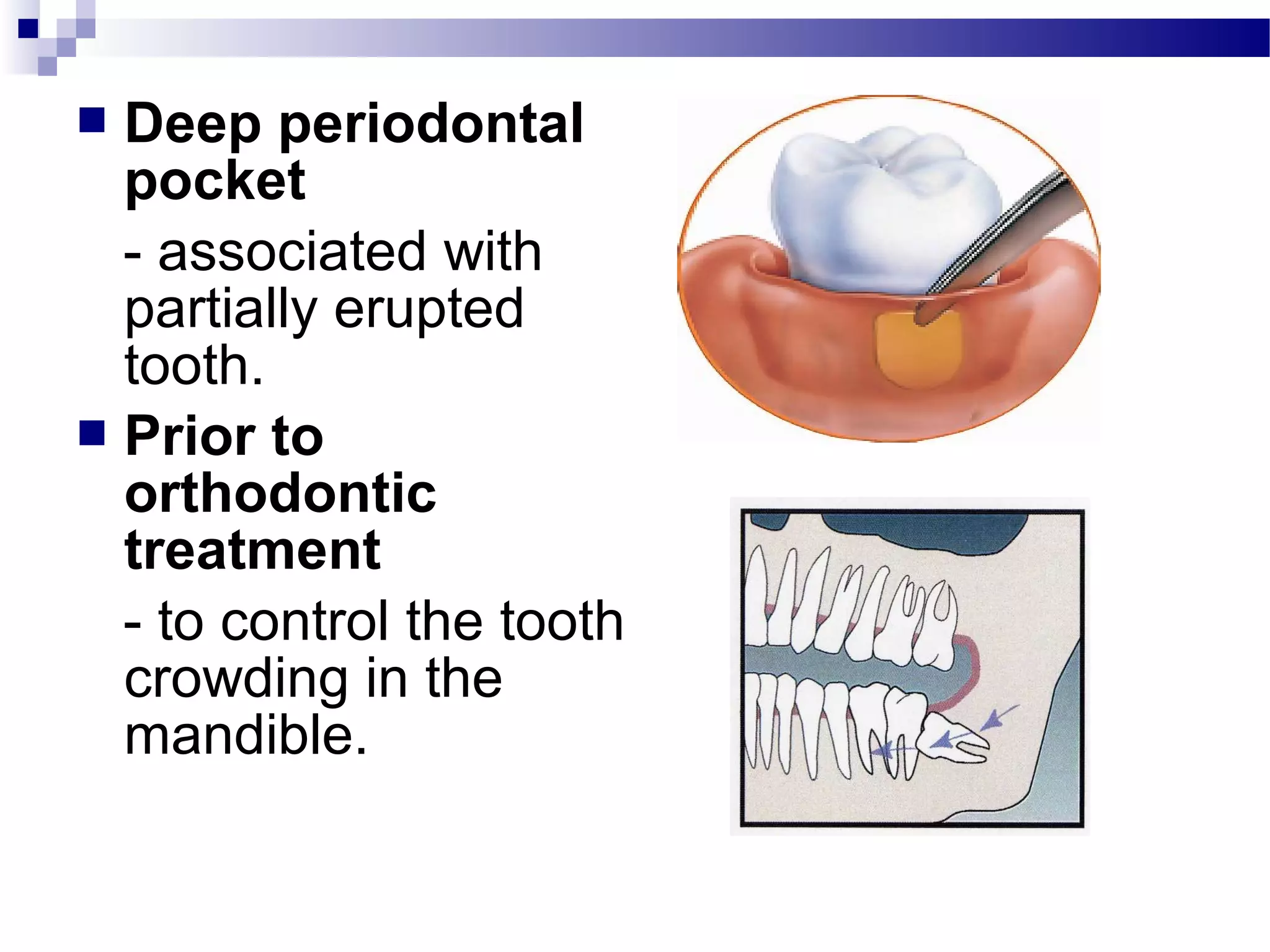
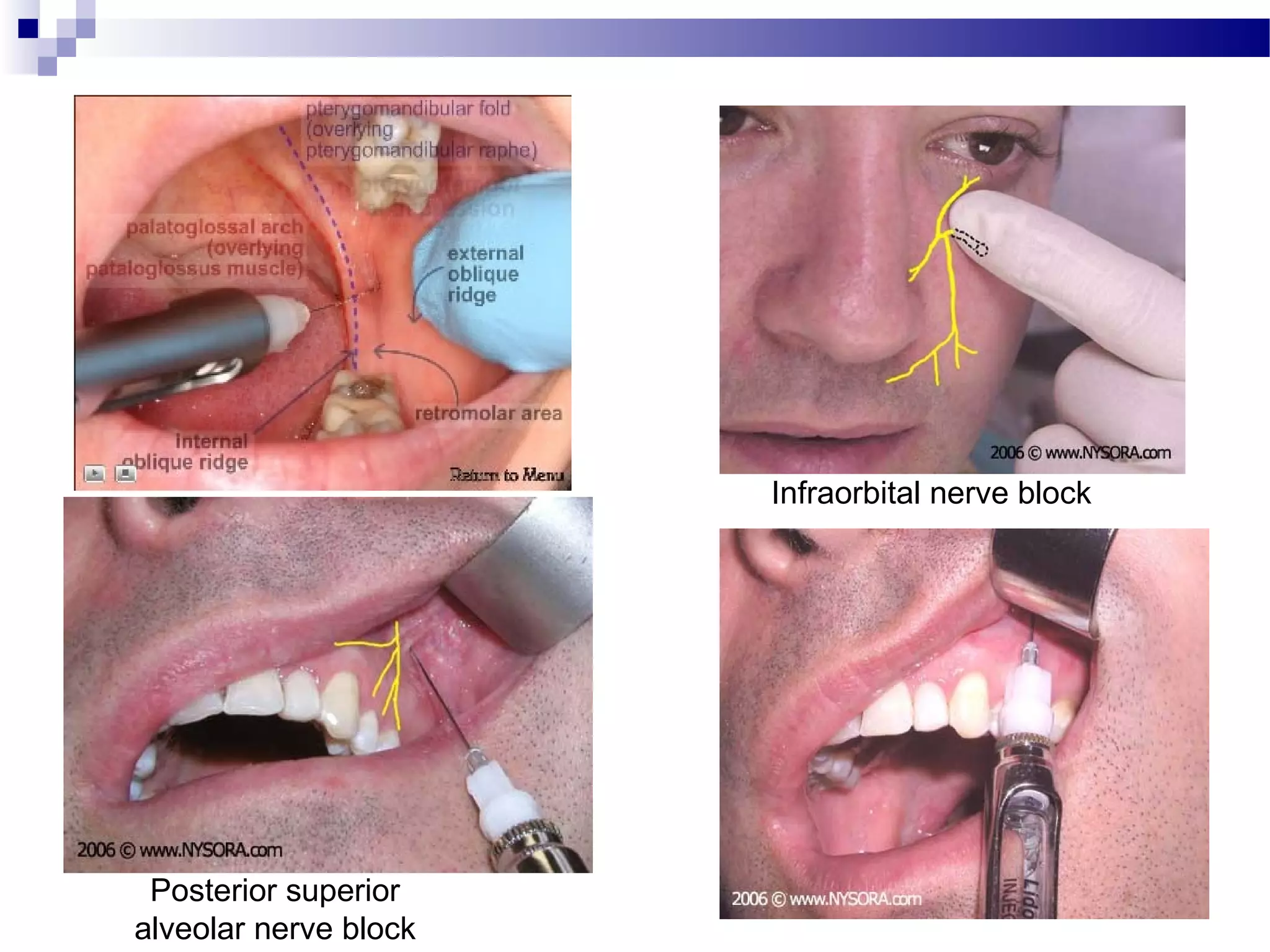
2) Surgical removal of impacted teeth involves asepsis, anesthesia, incisions, bone removal, tooth sectioning, elevation and extraction while protecting surrounding structures.
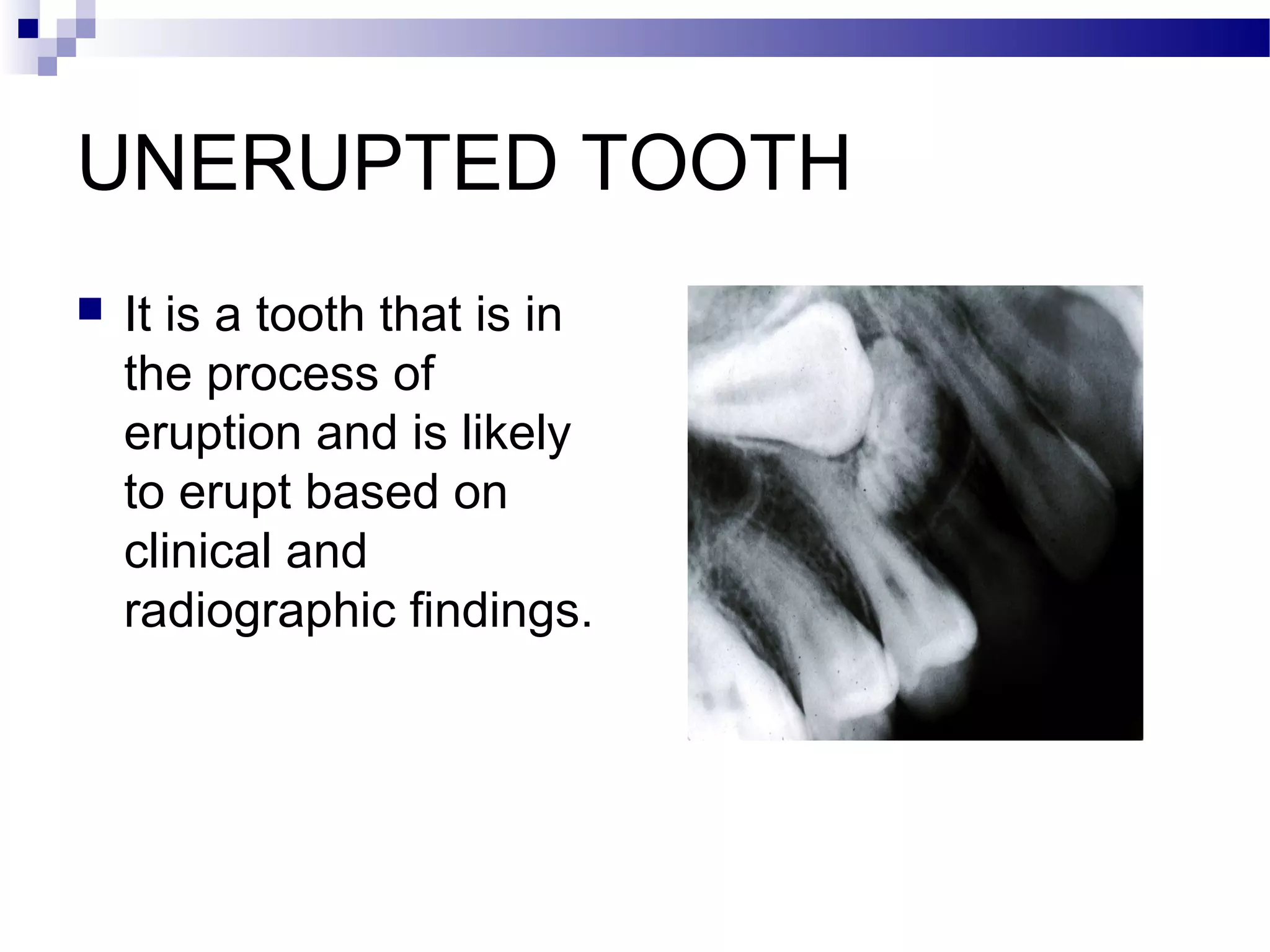
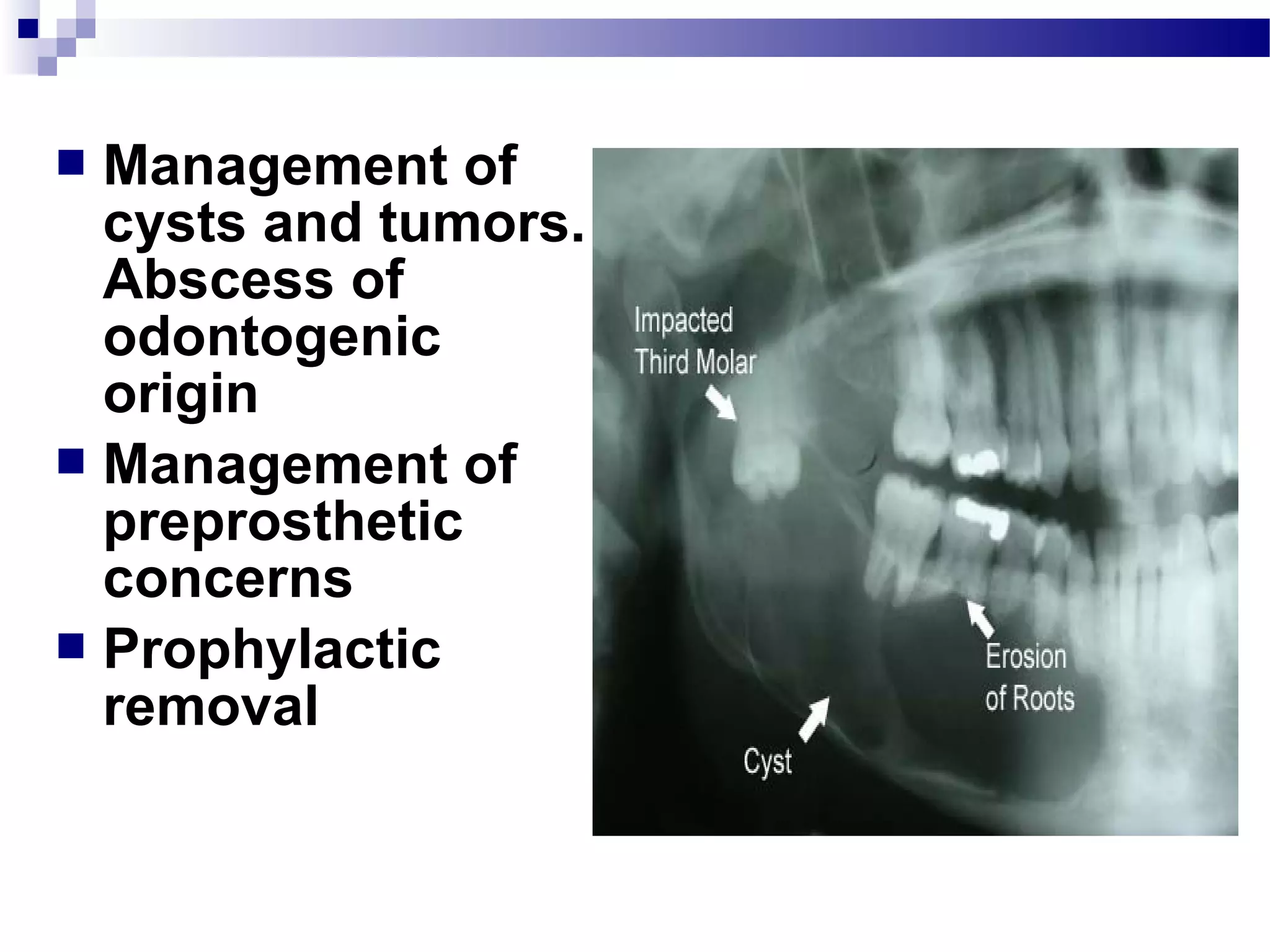
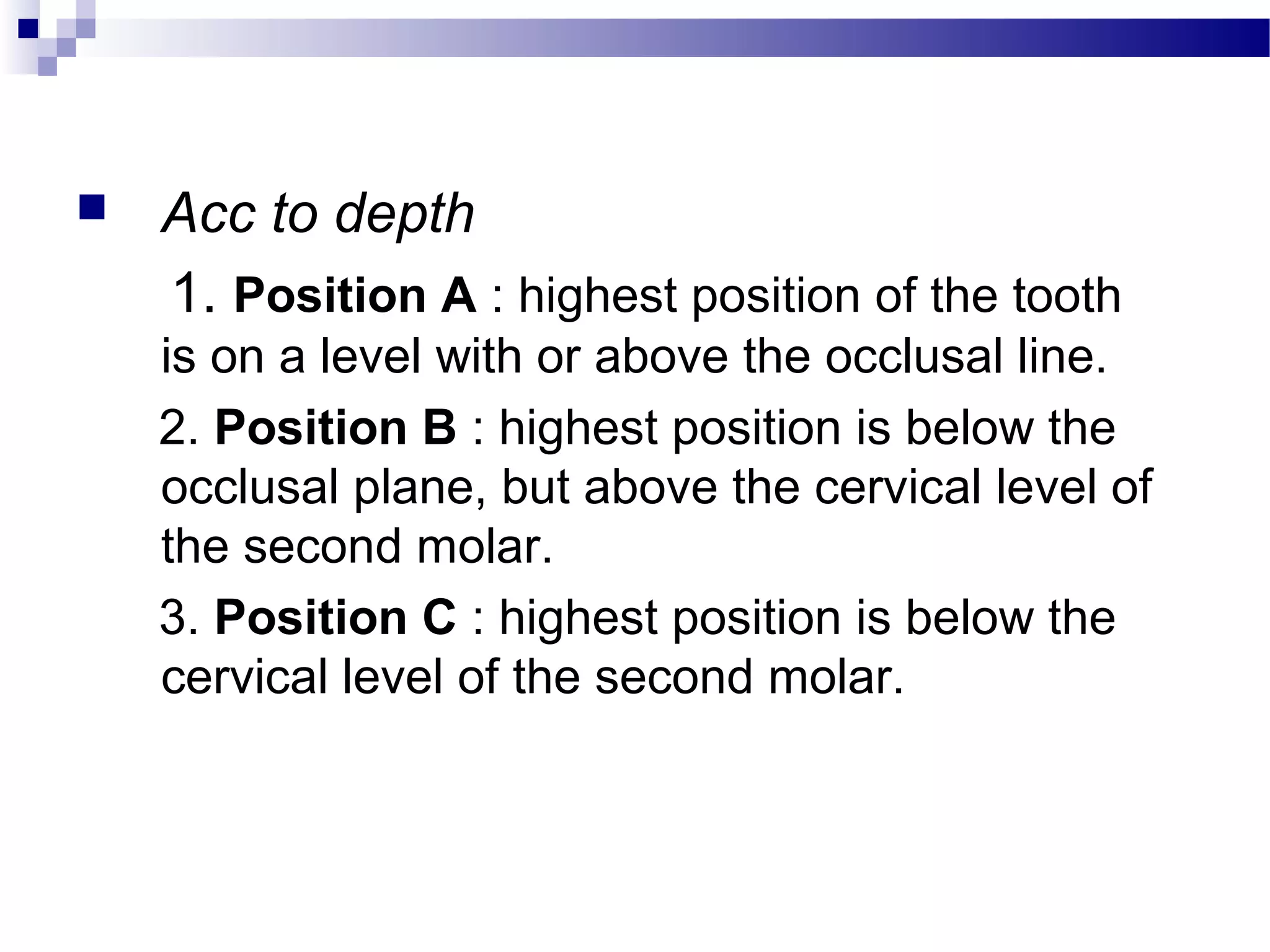
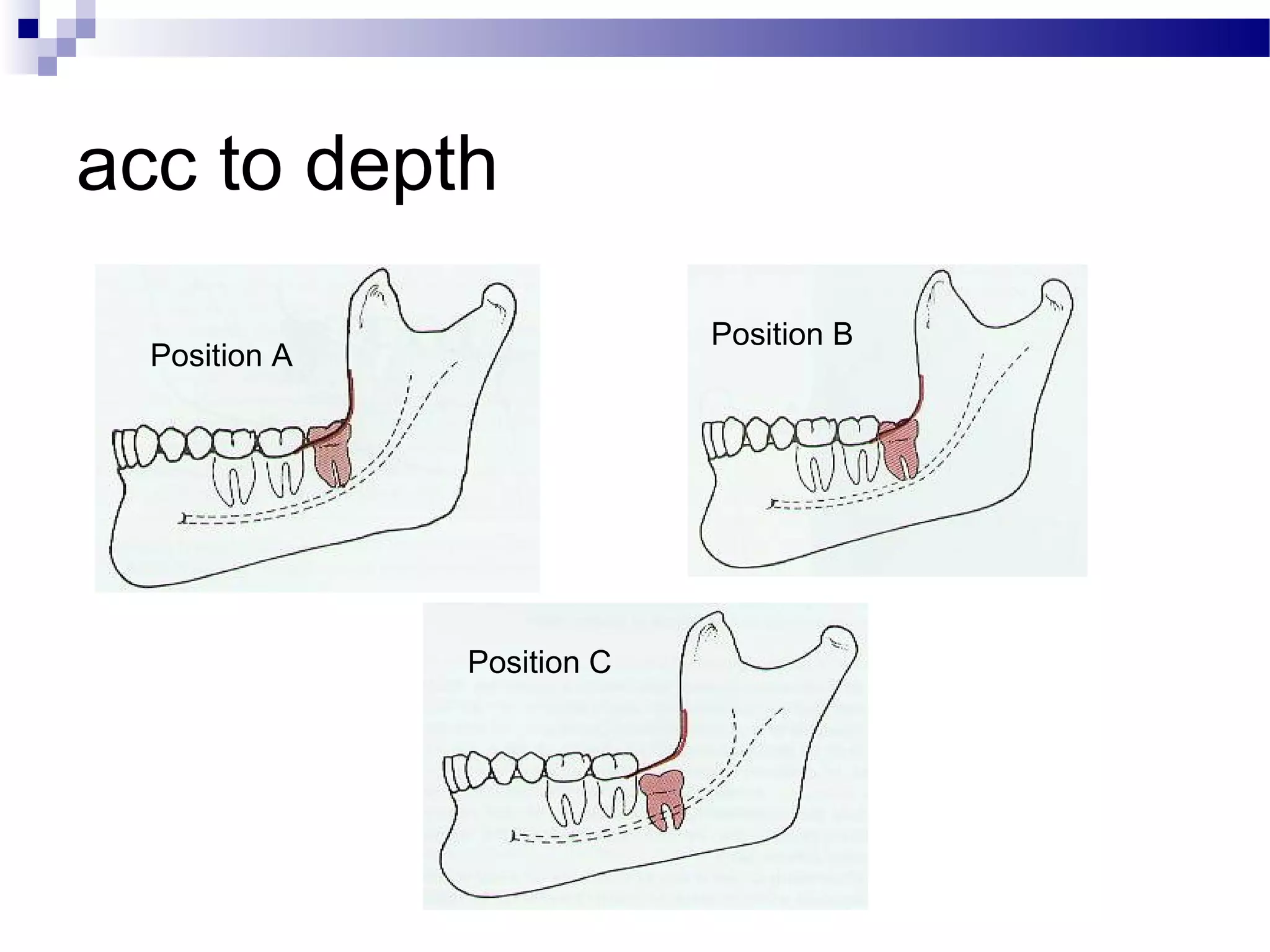
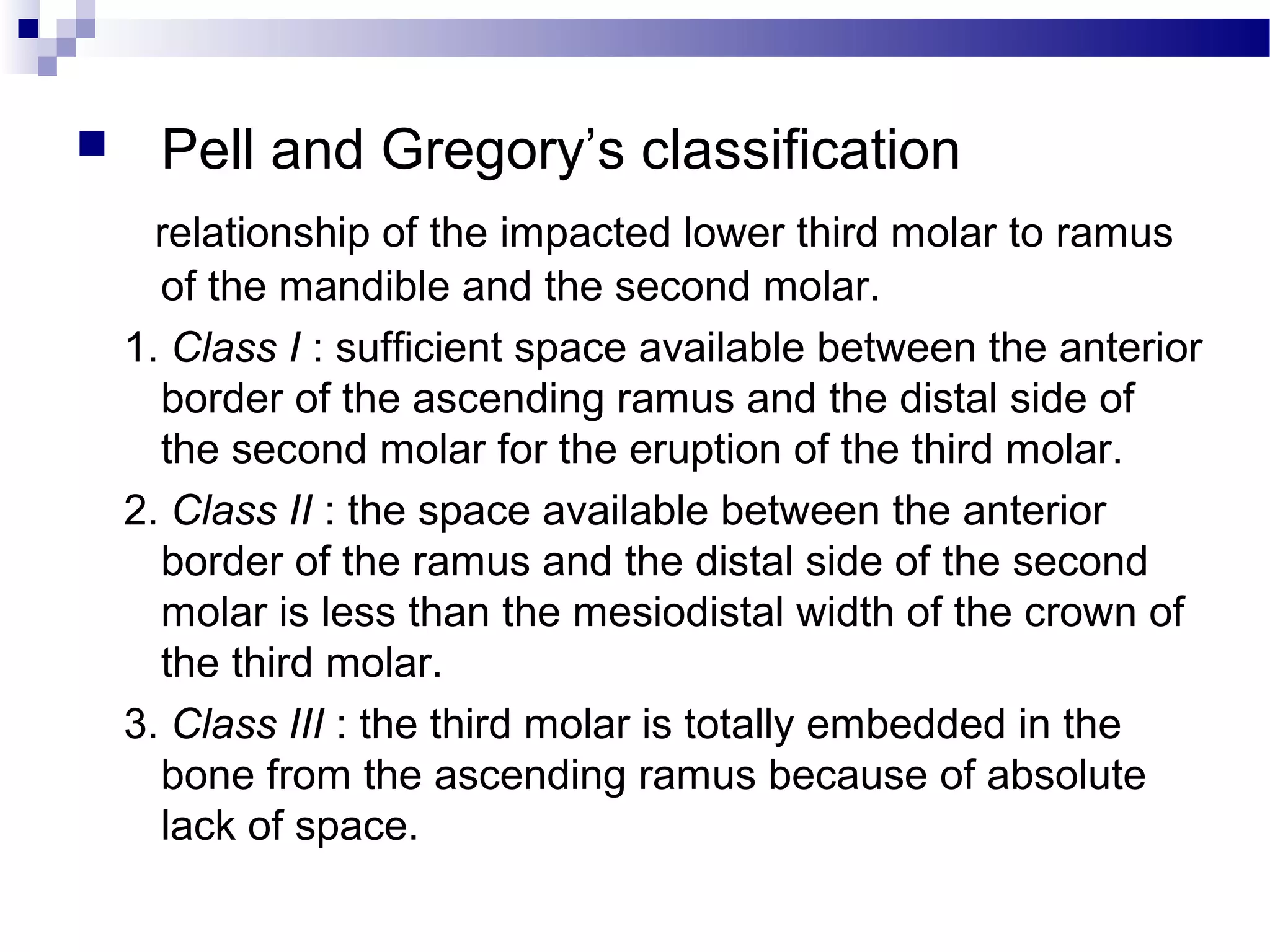
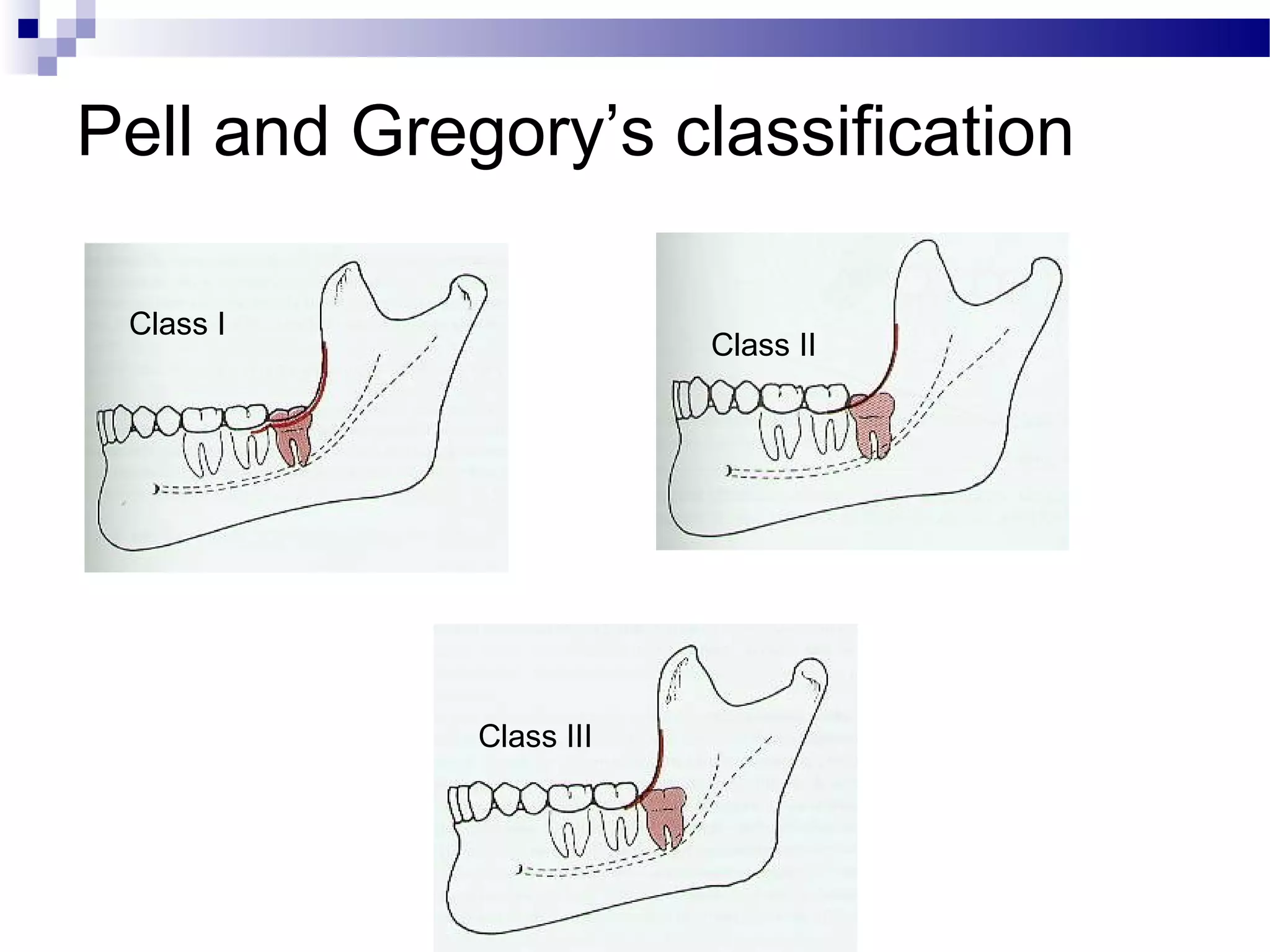
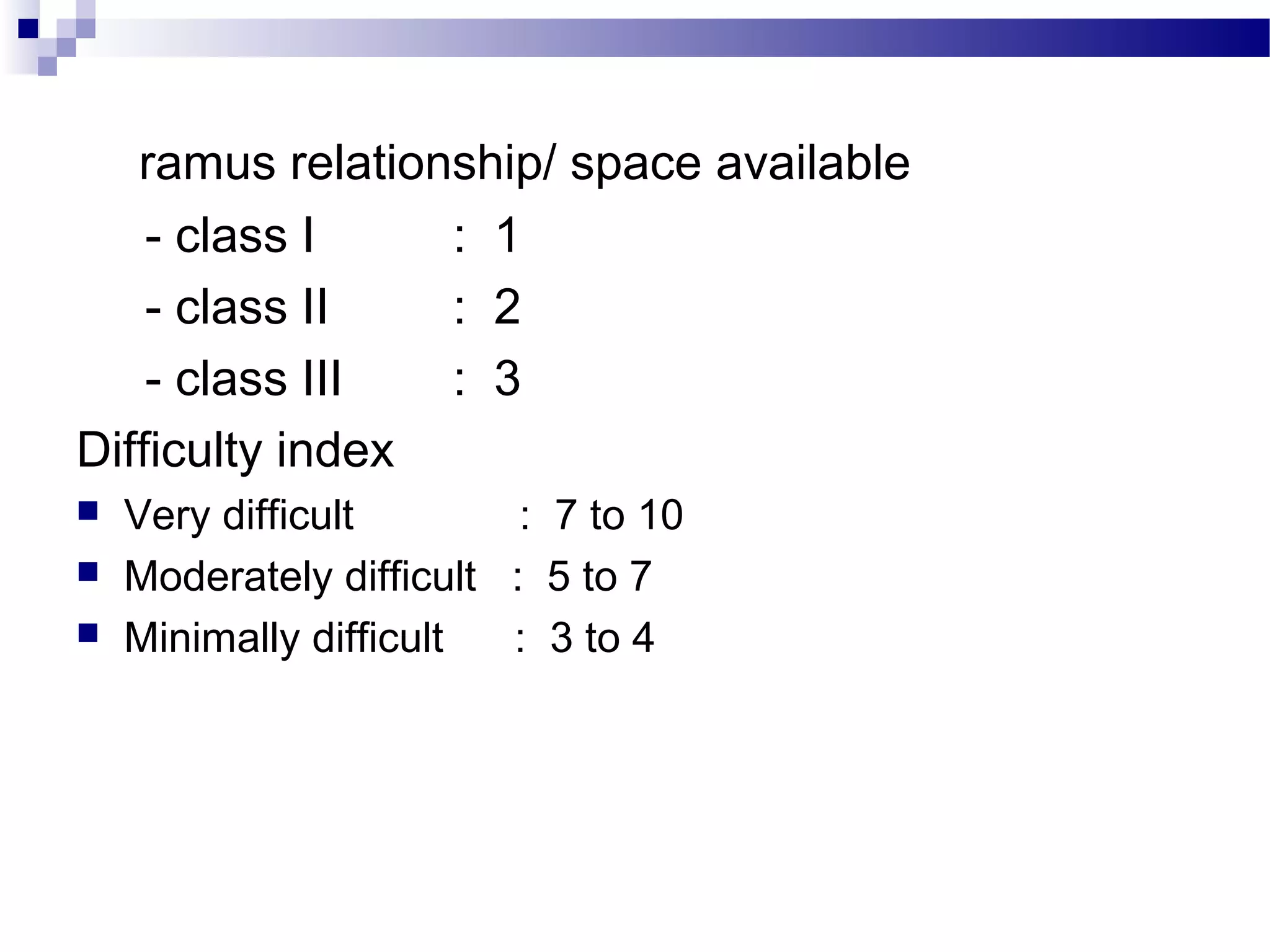
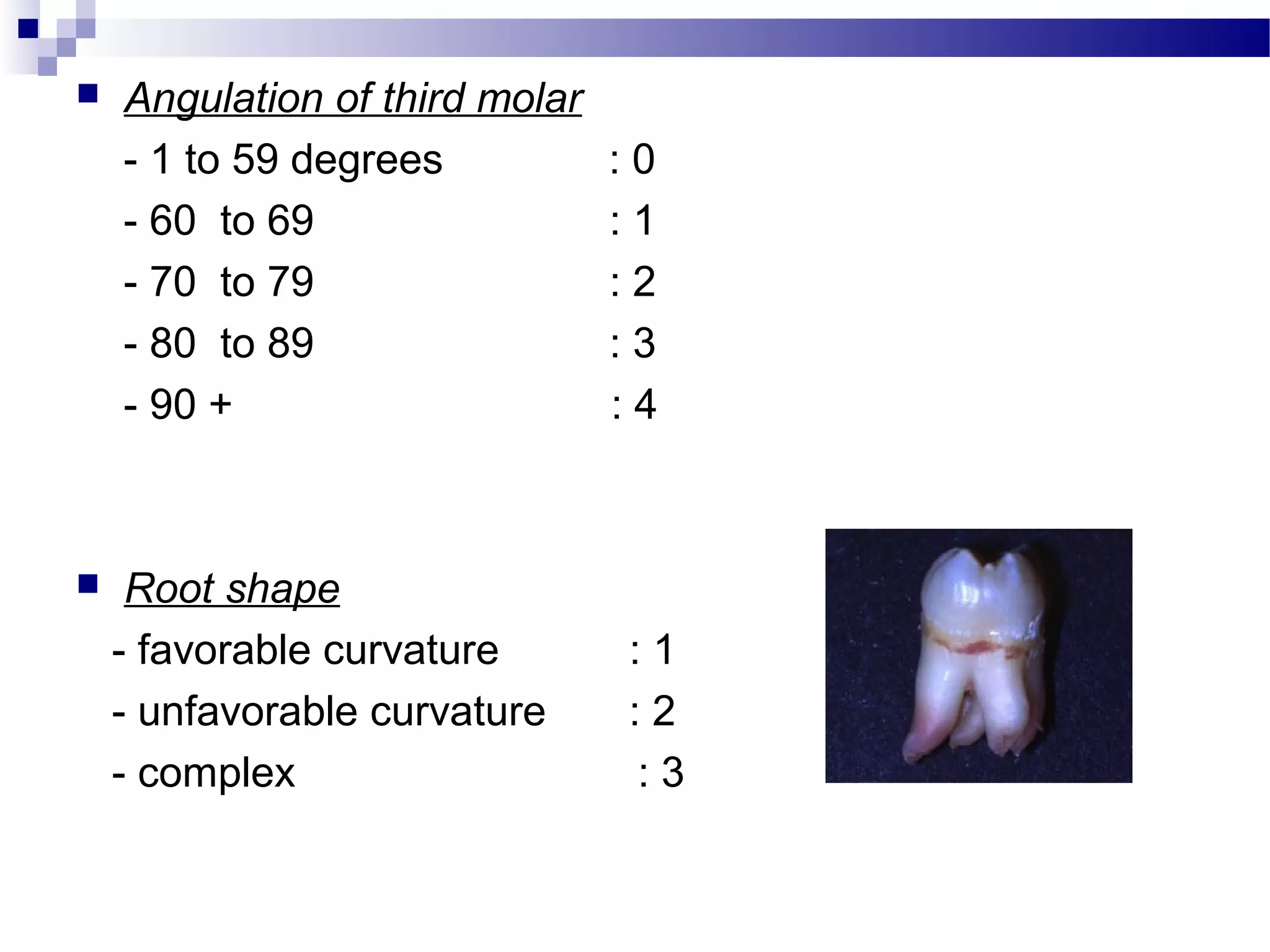
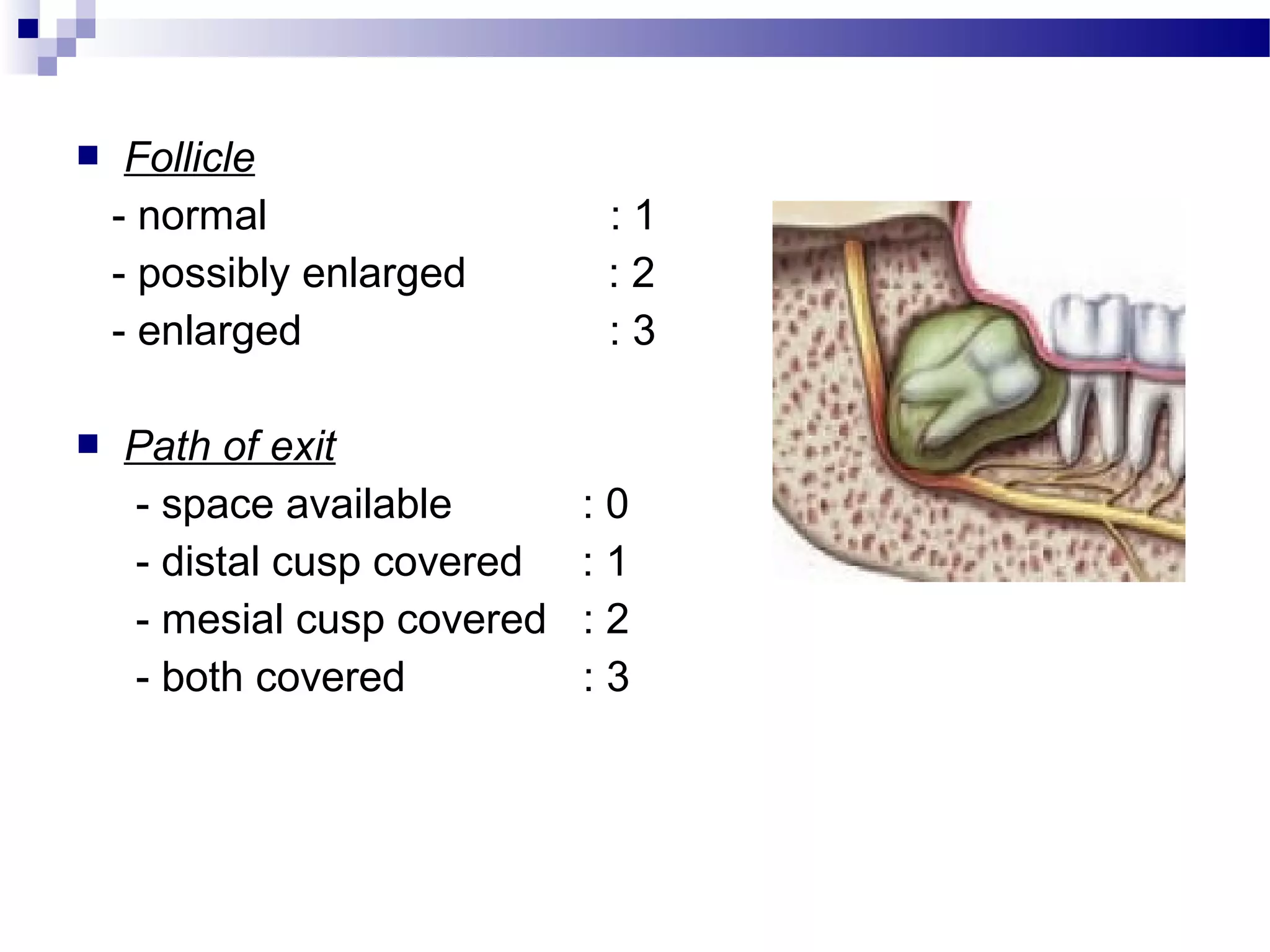
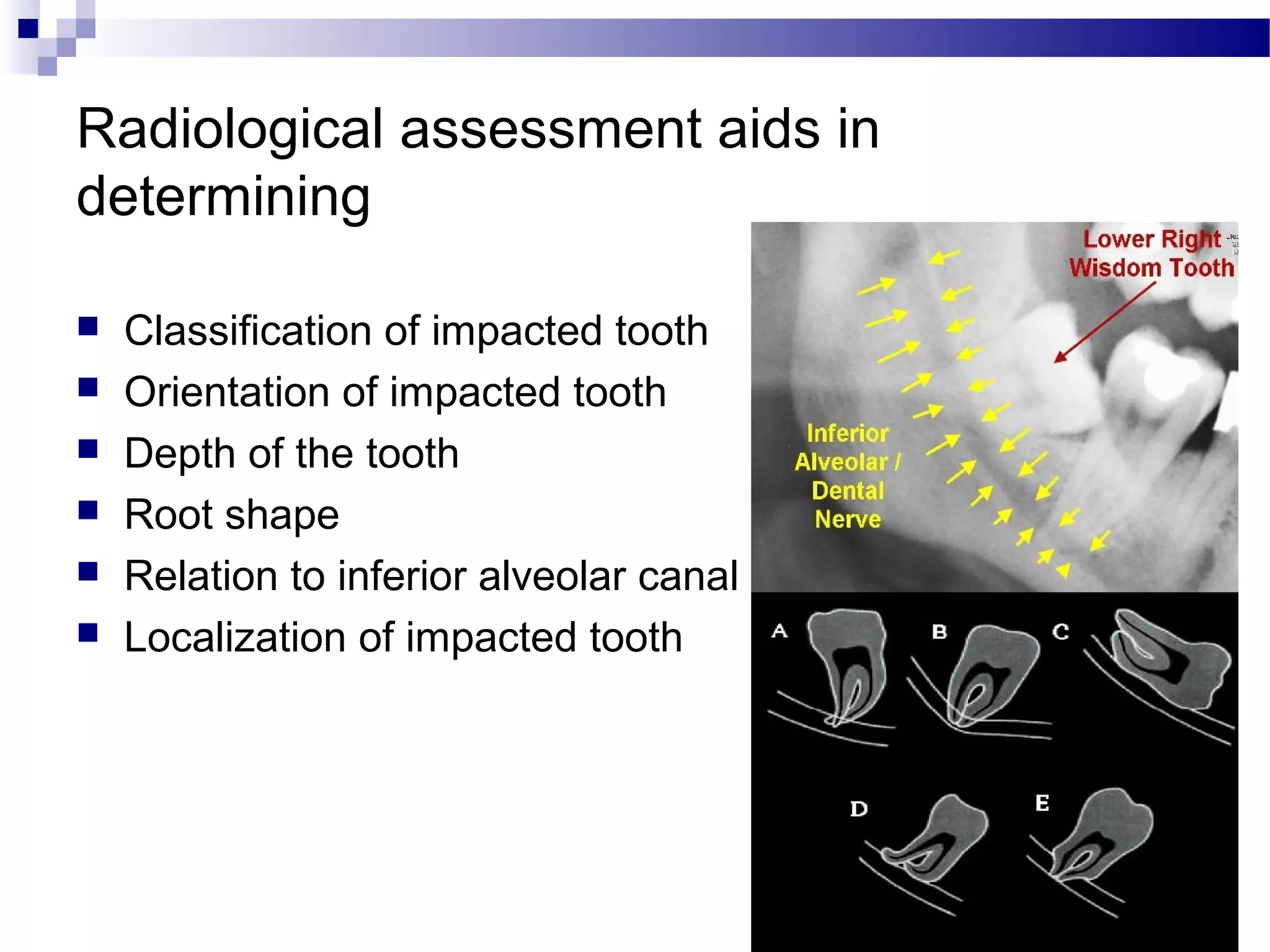
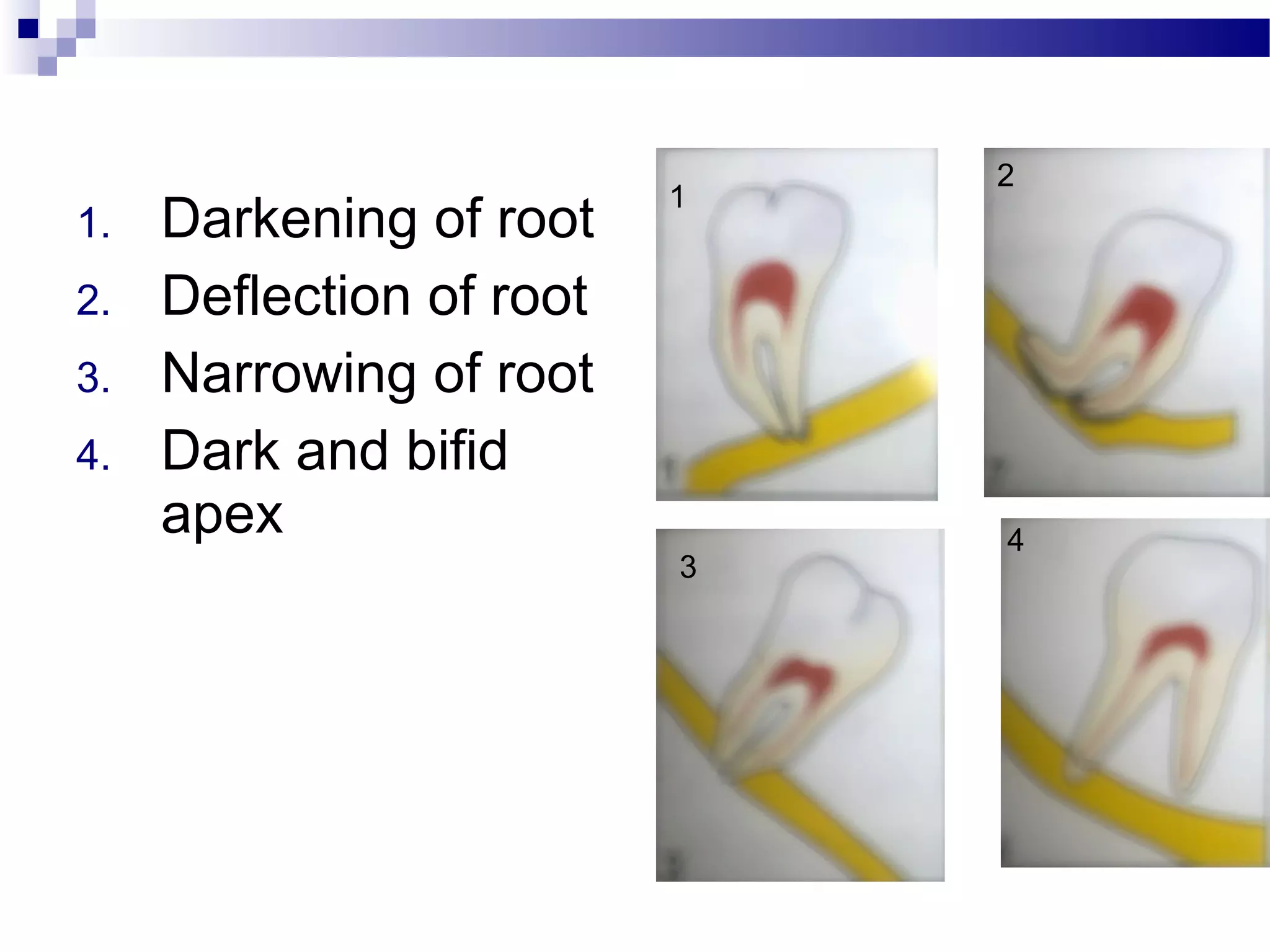
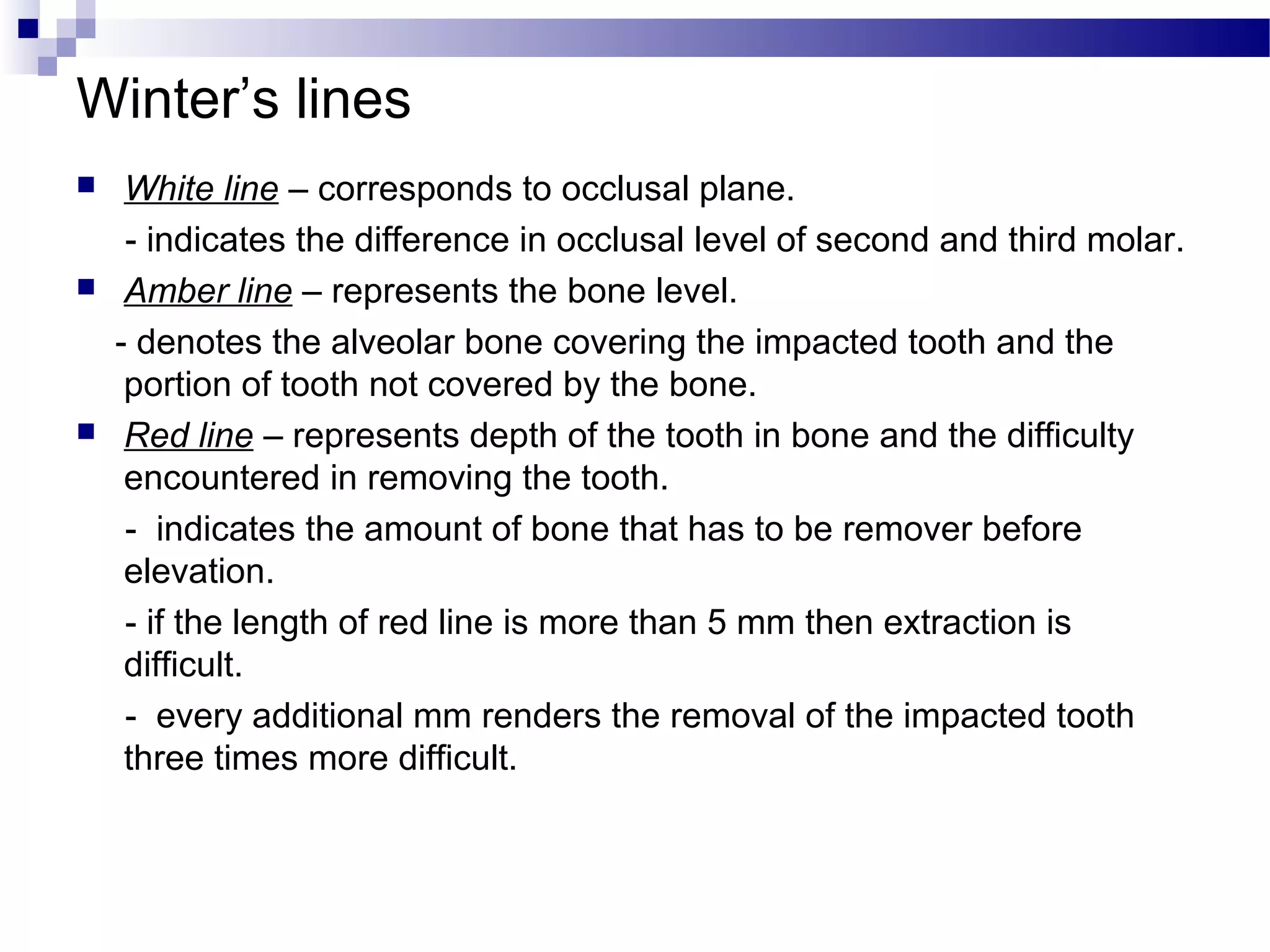
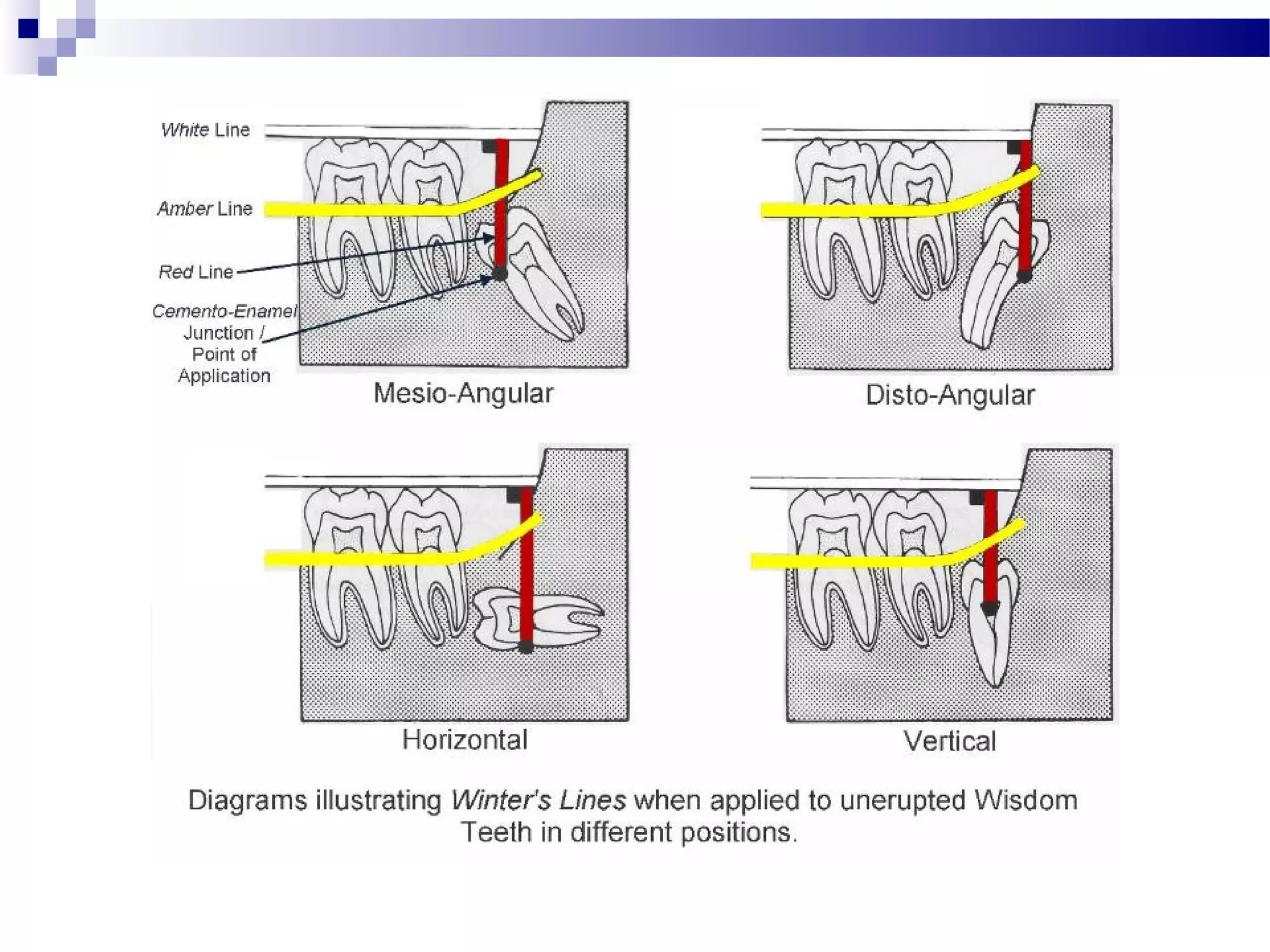
3) Radiographs aid in determining the depth, orientation and relationship to nearby anatomy to assess difficulty prior to surgery. Careful treatment planning is important for safe and effective removal of impacted teeth.