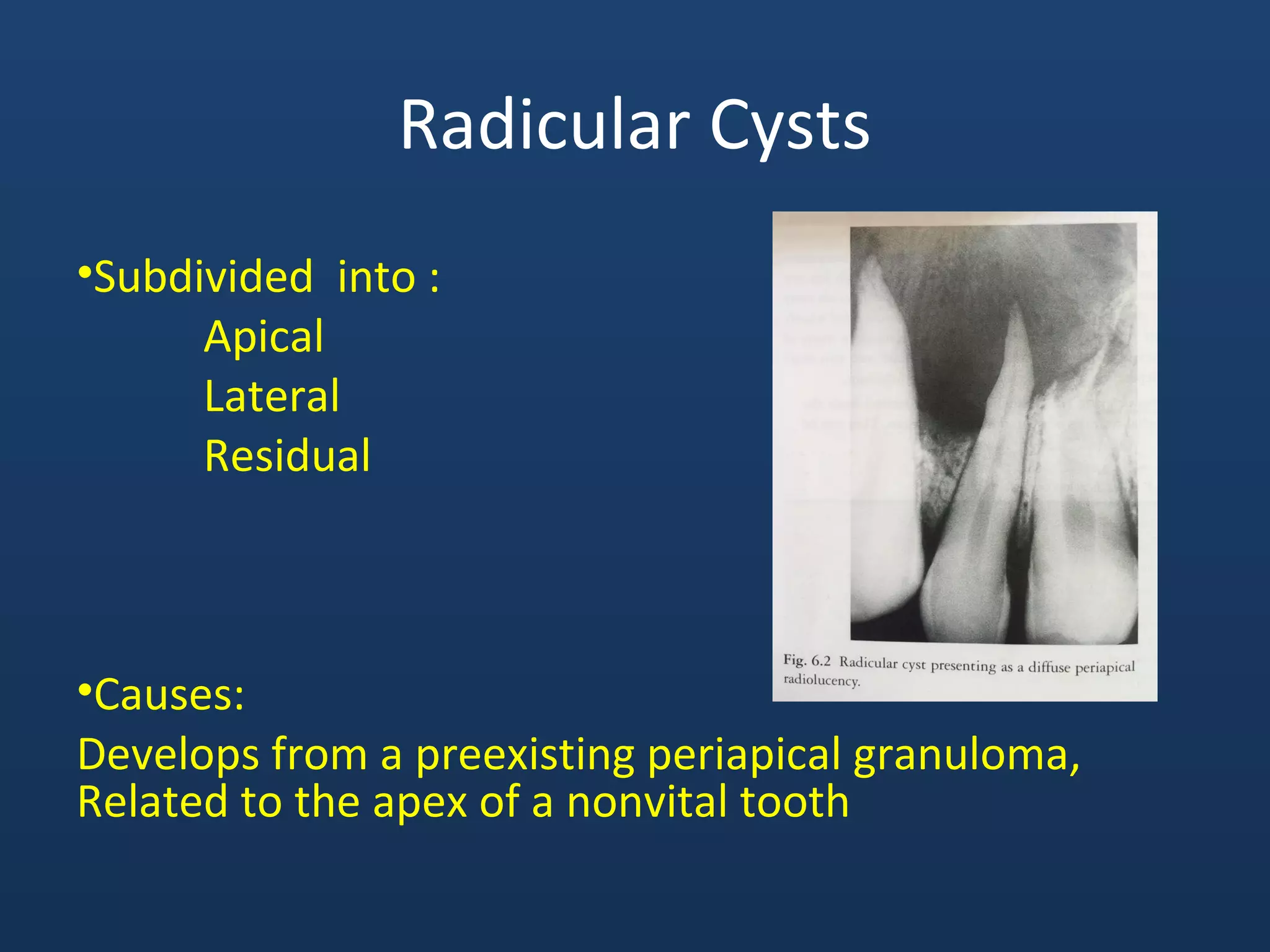
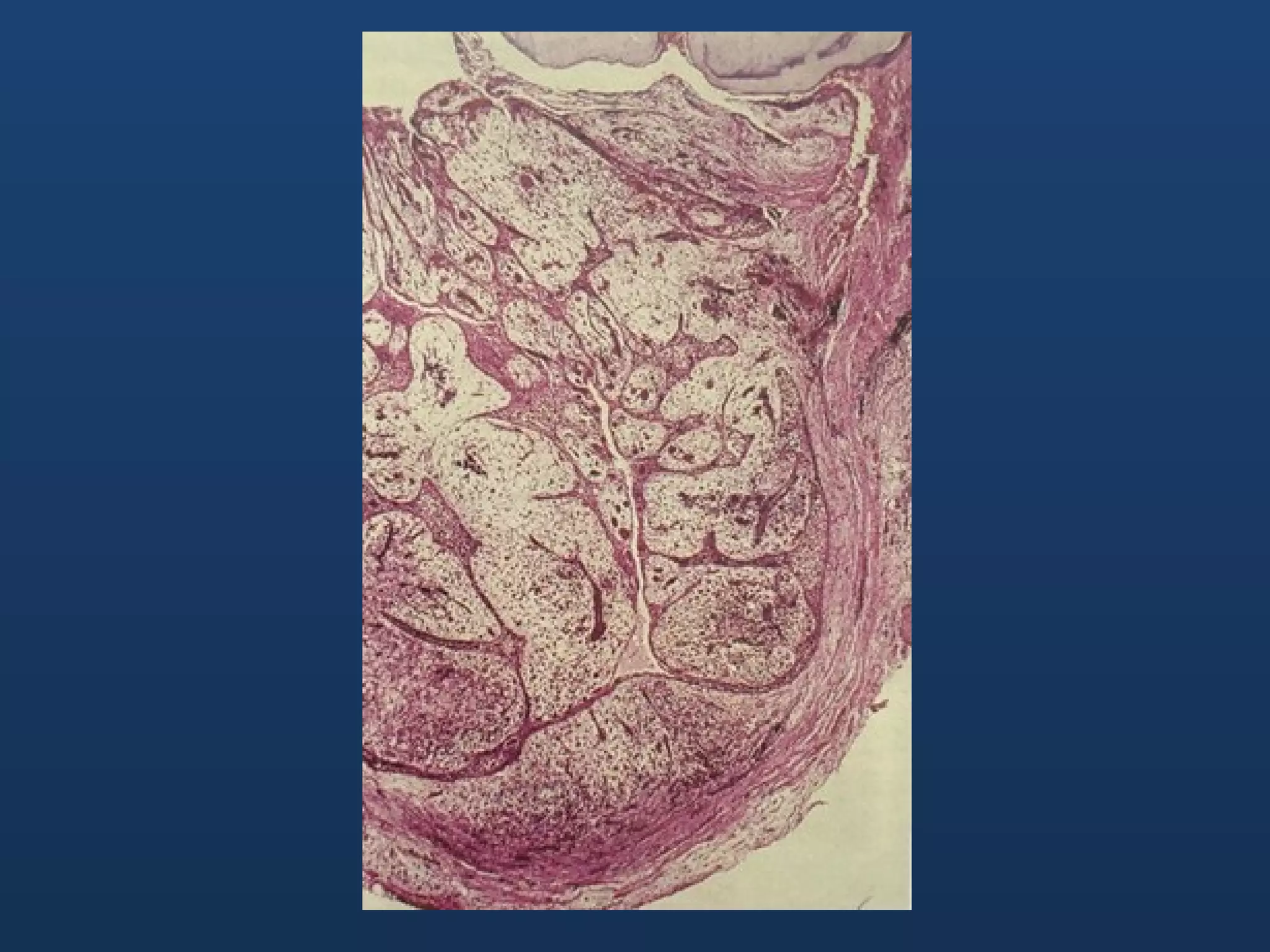
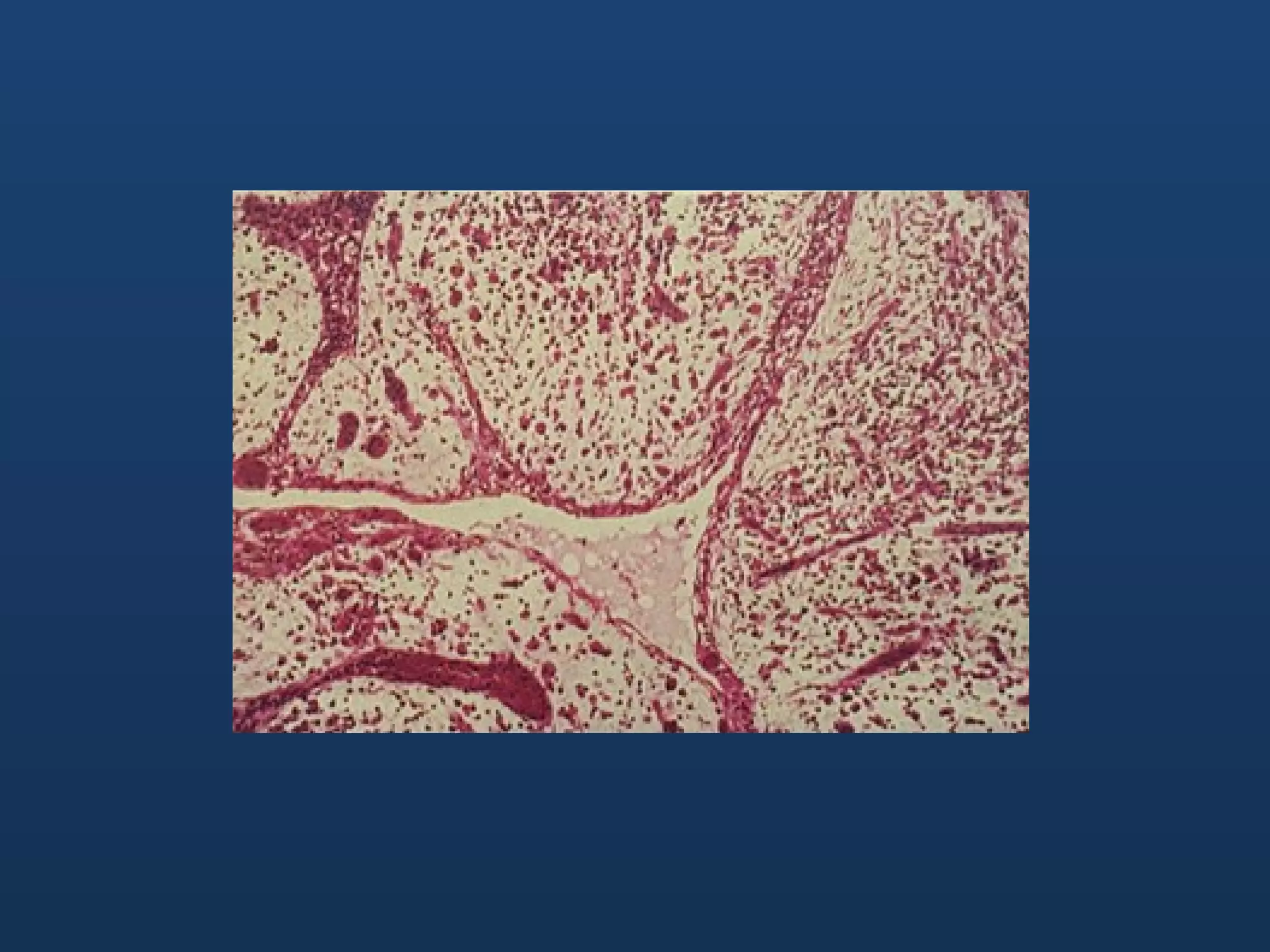
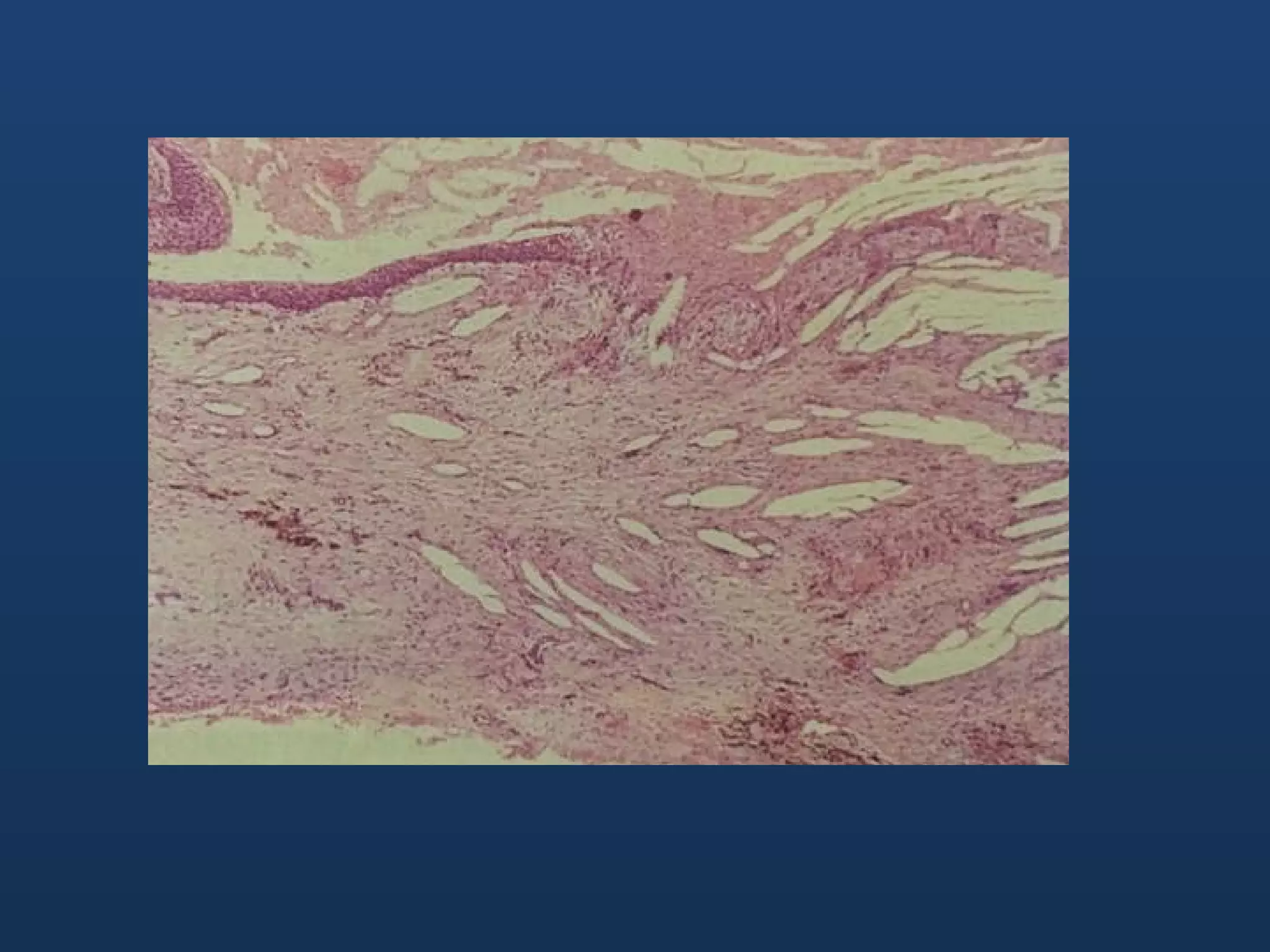
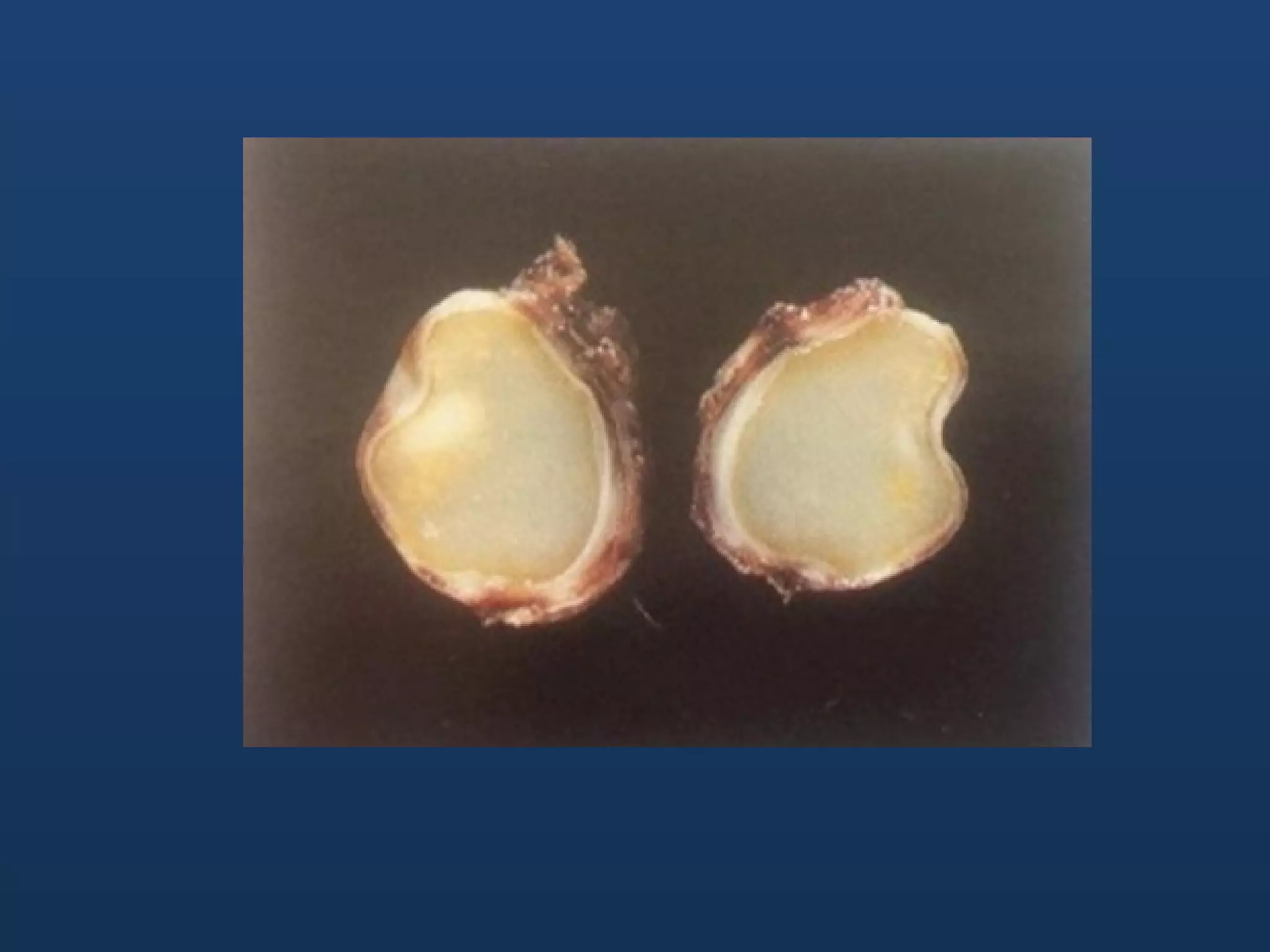
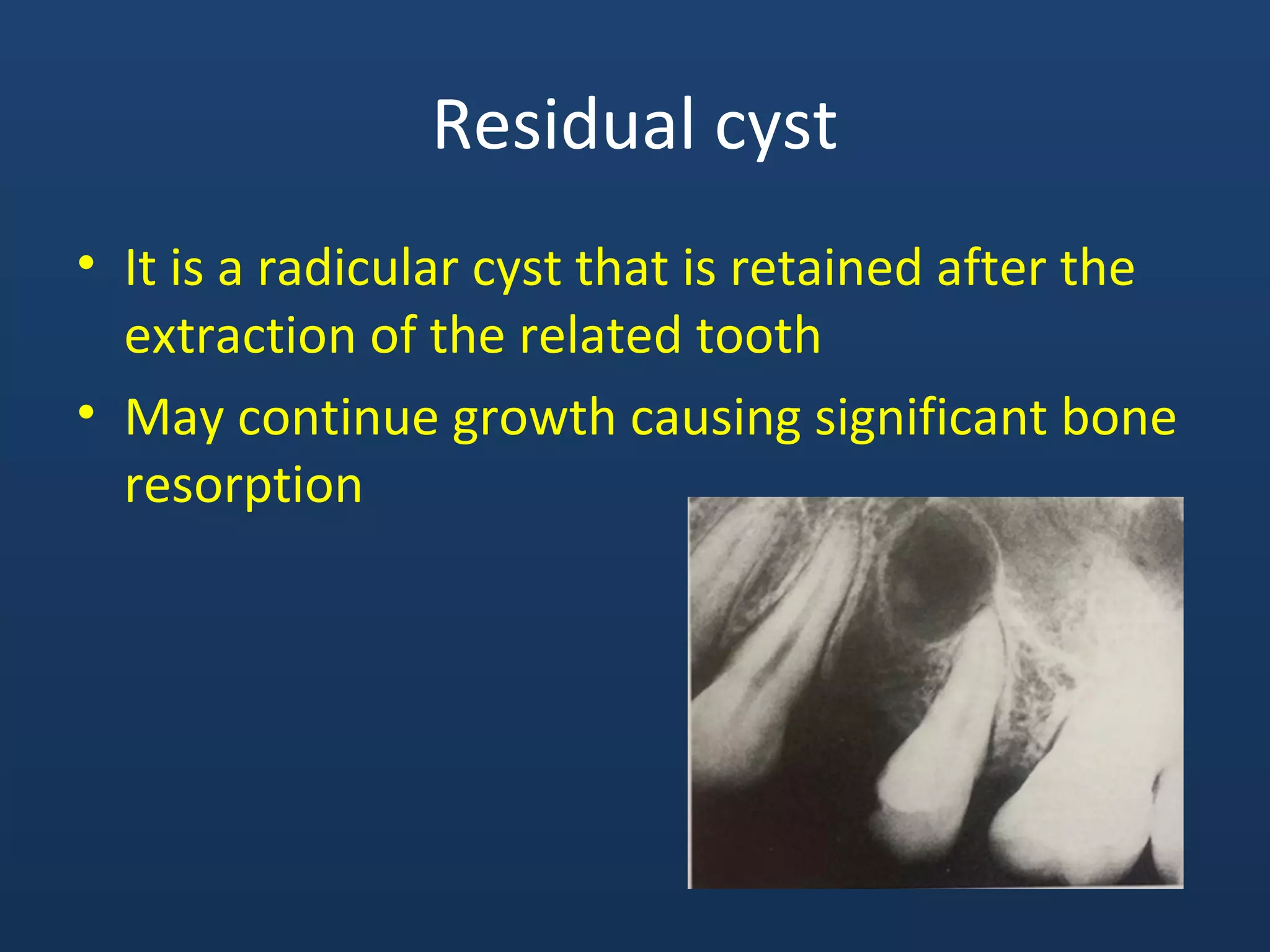
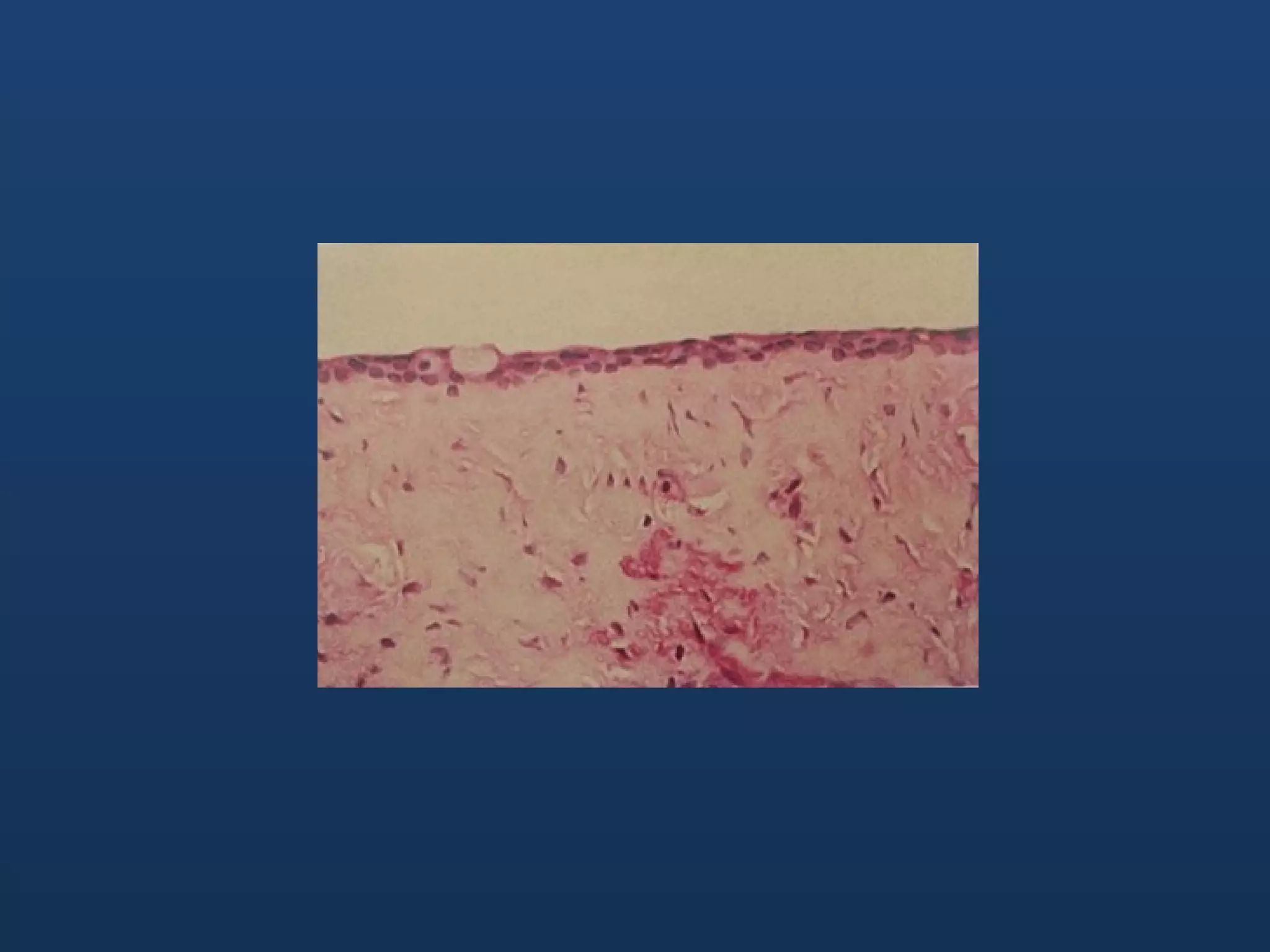
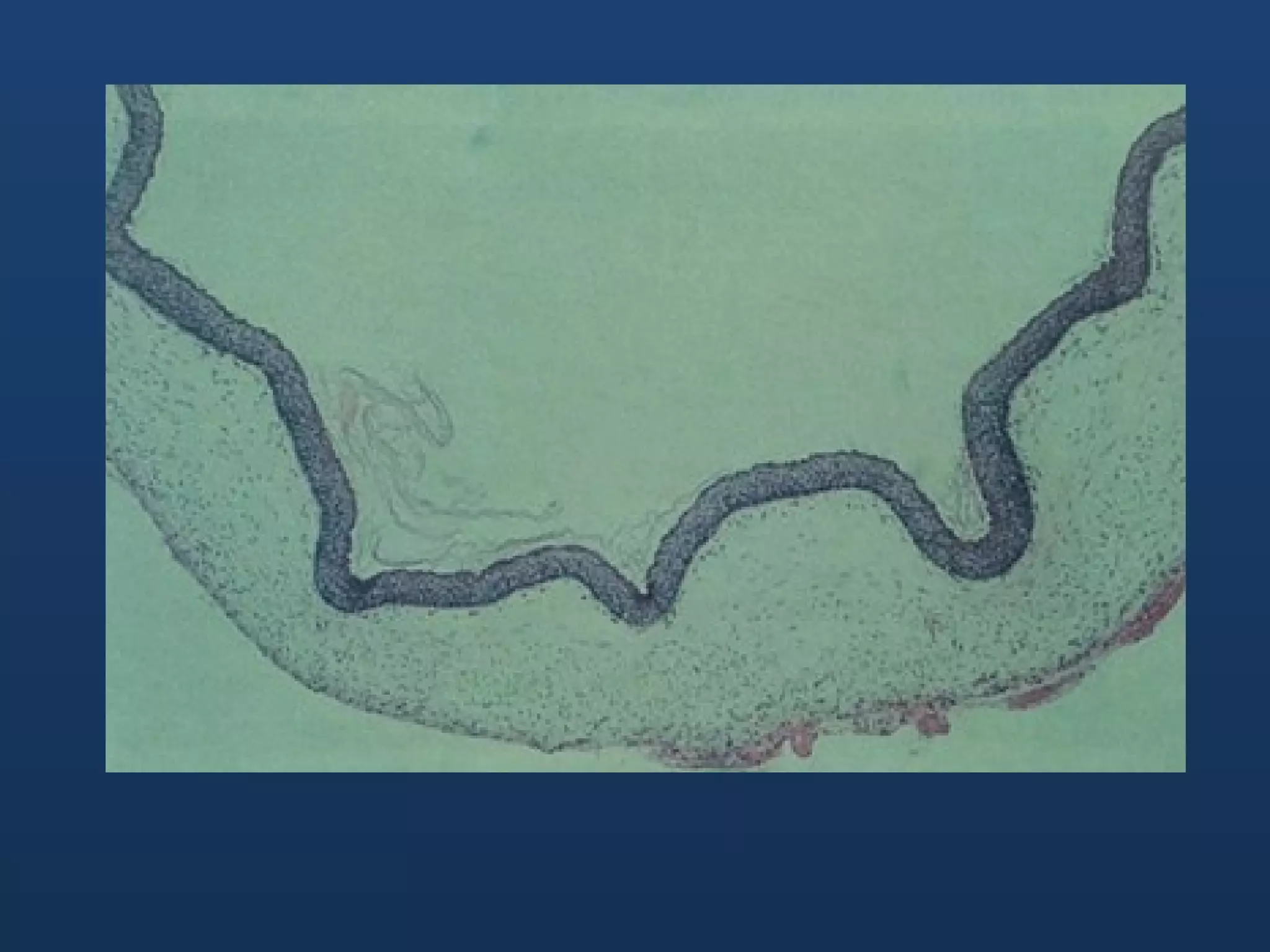
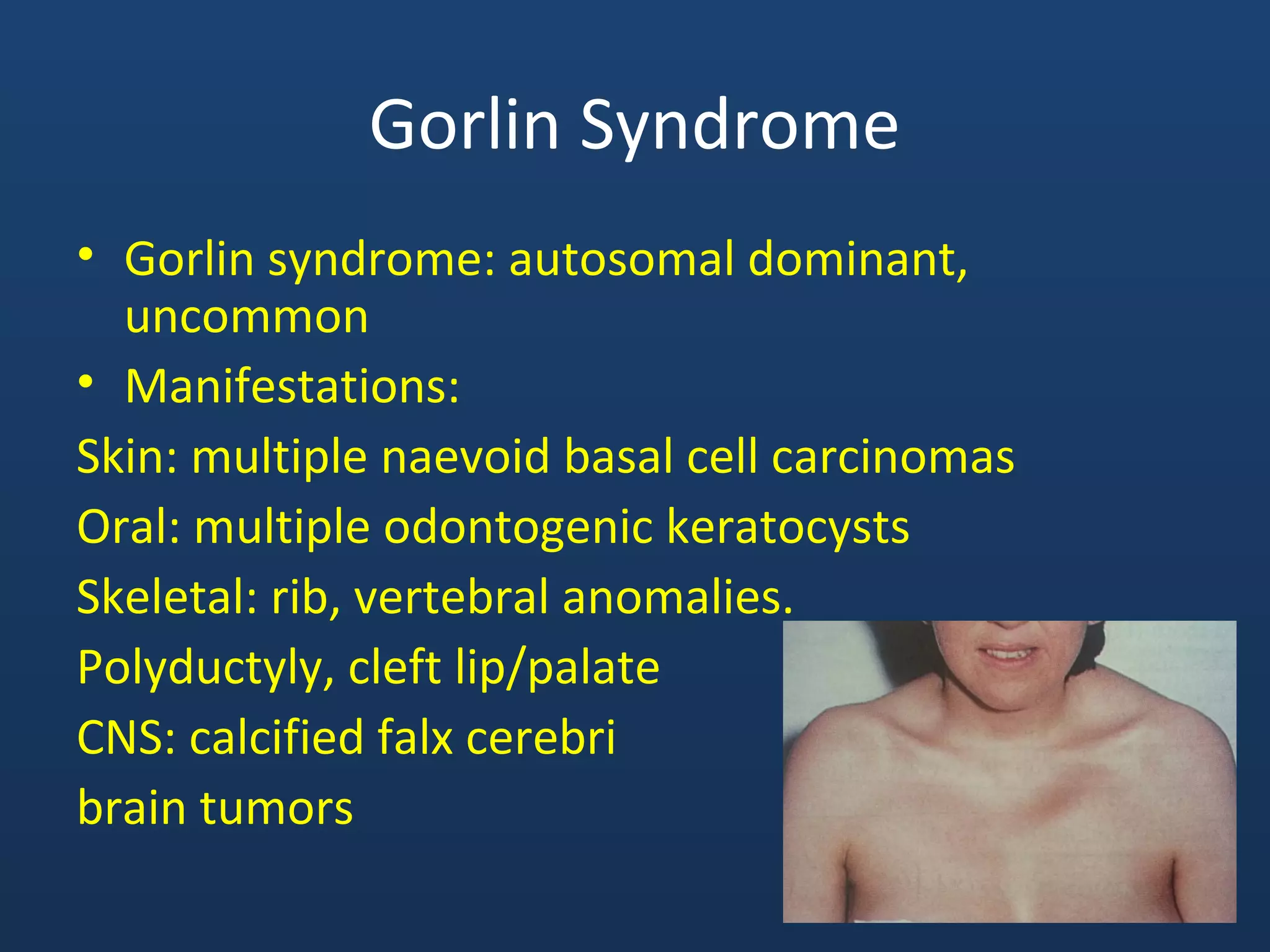
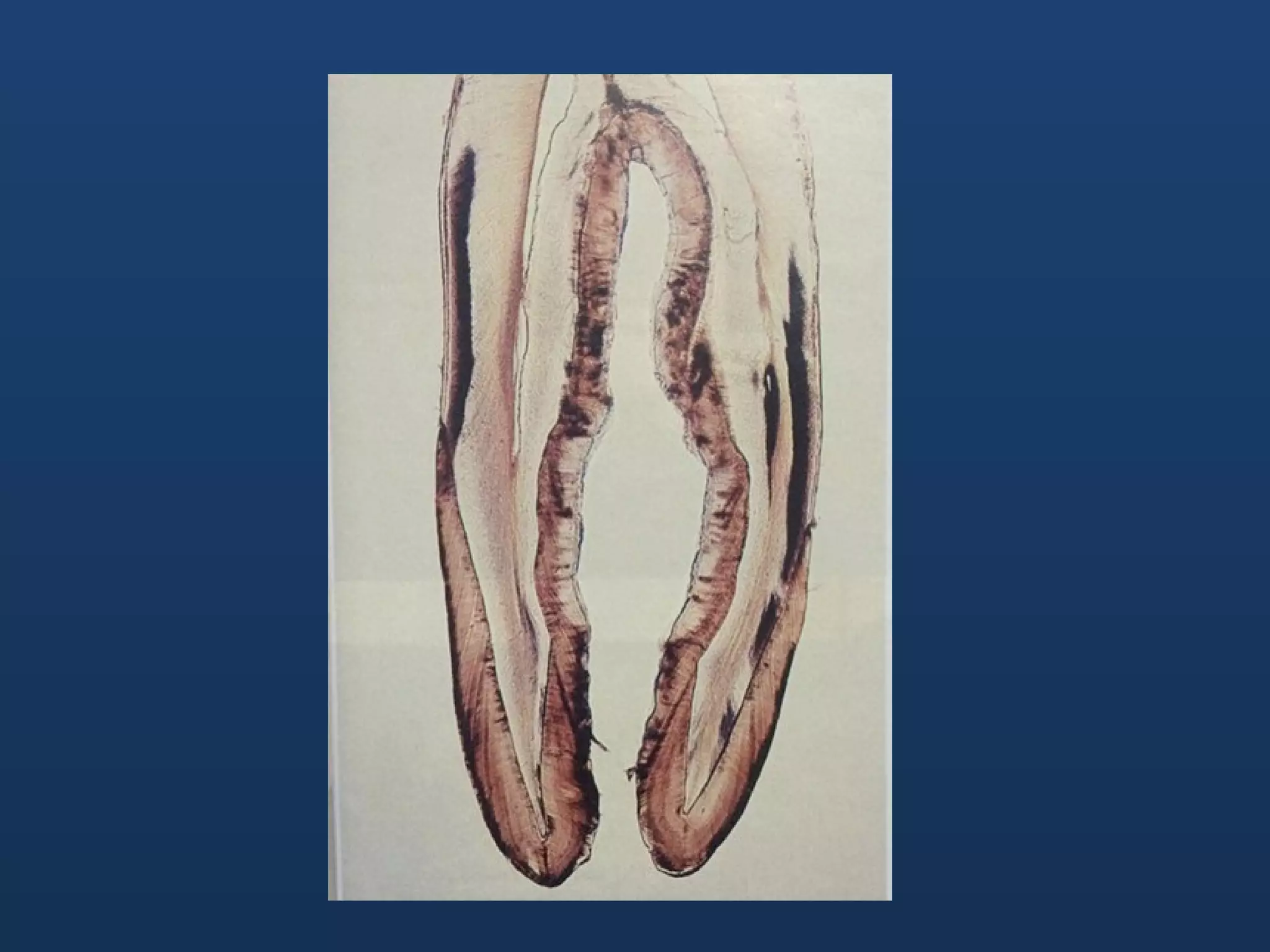
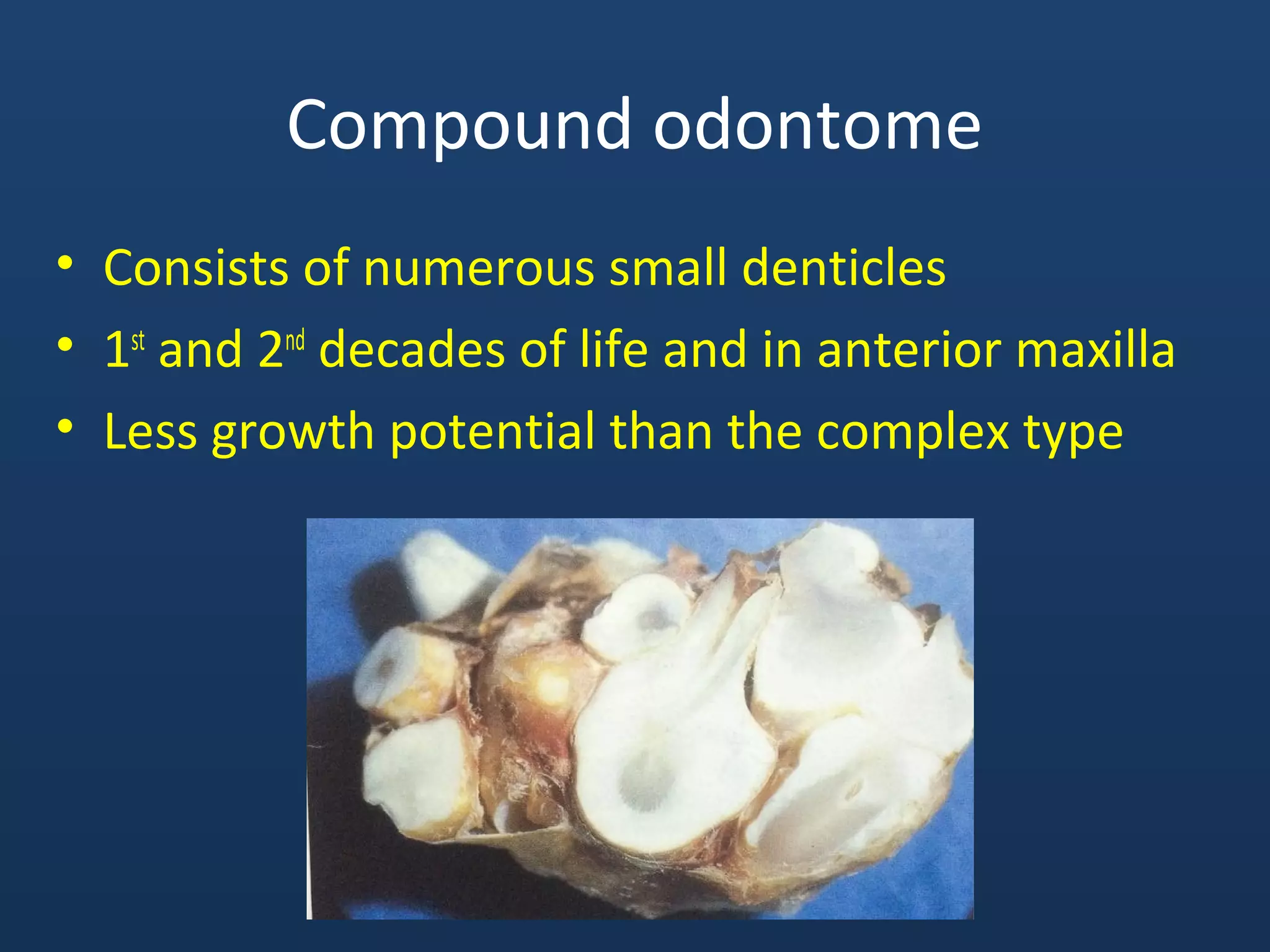
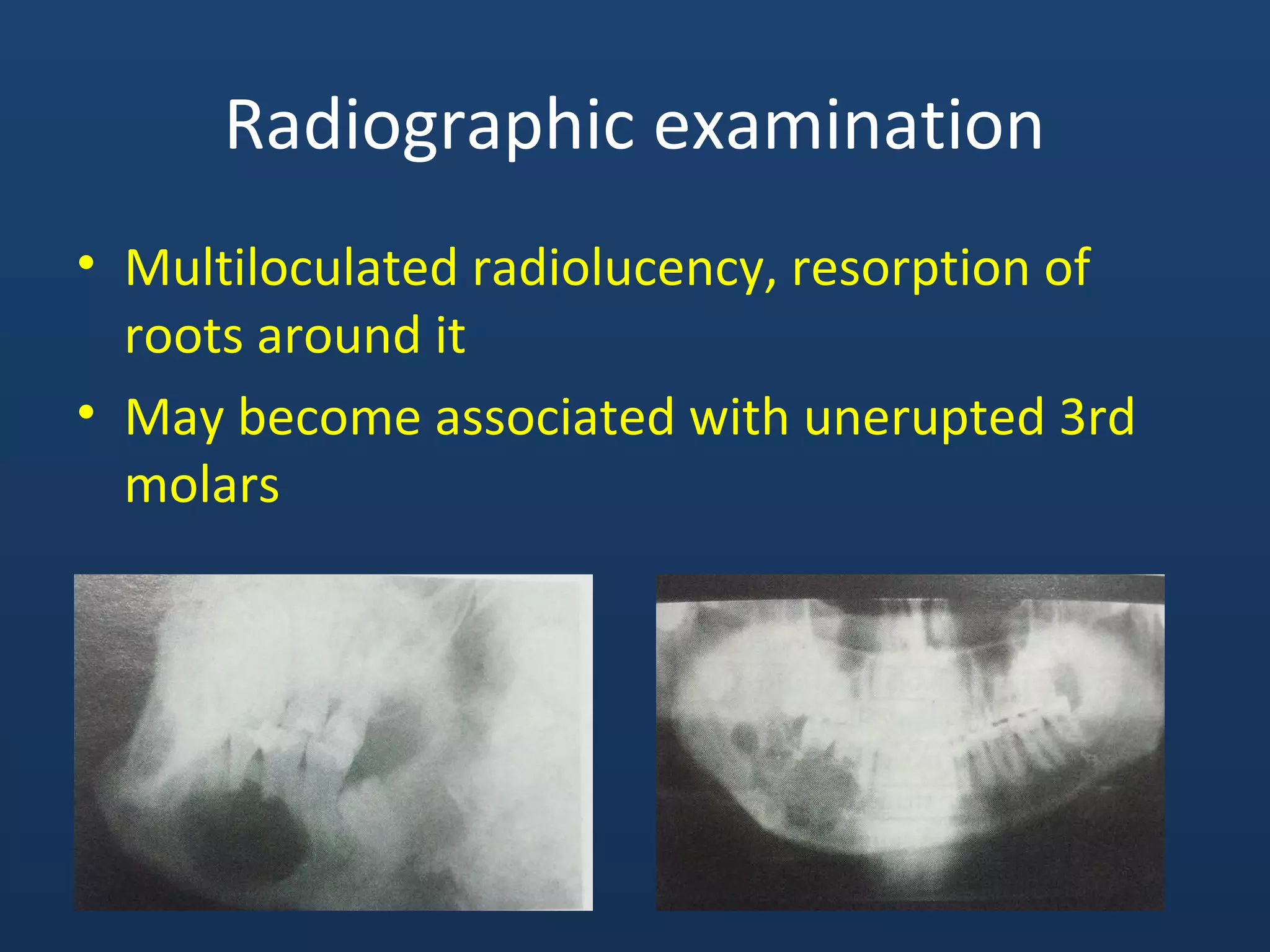
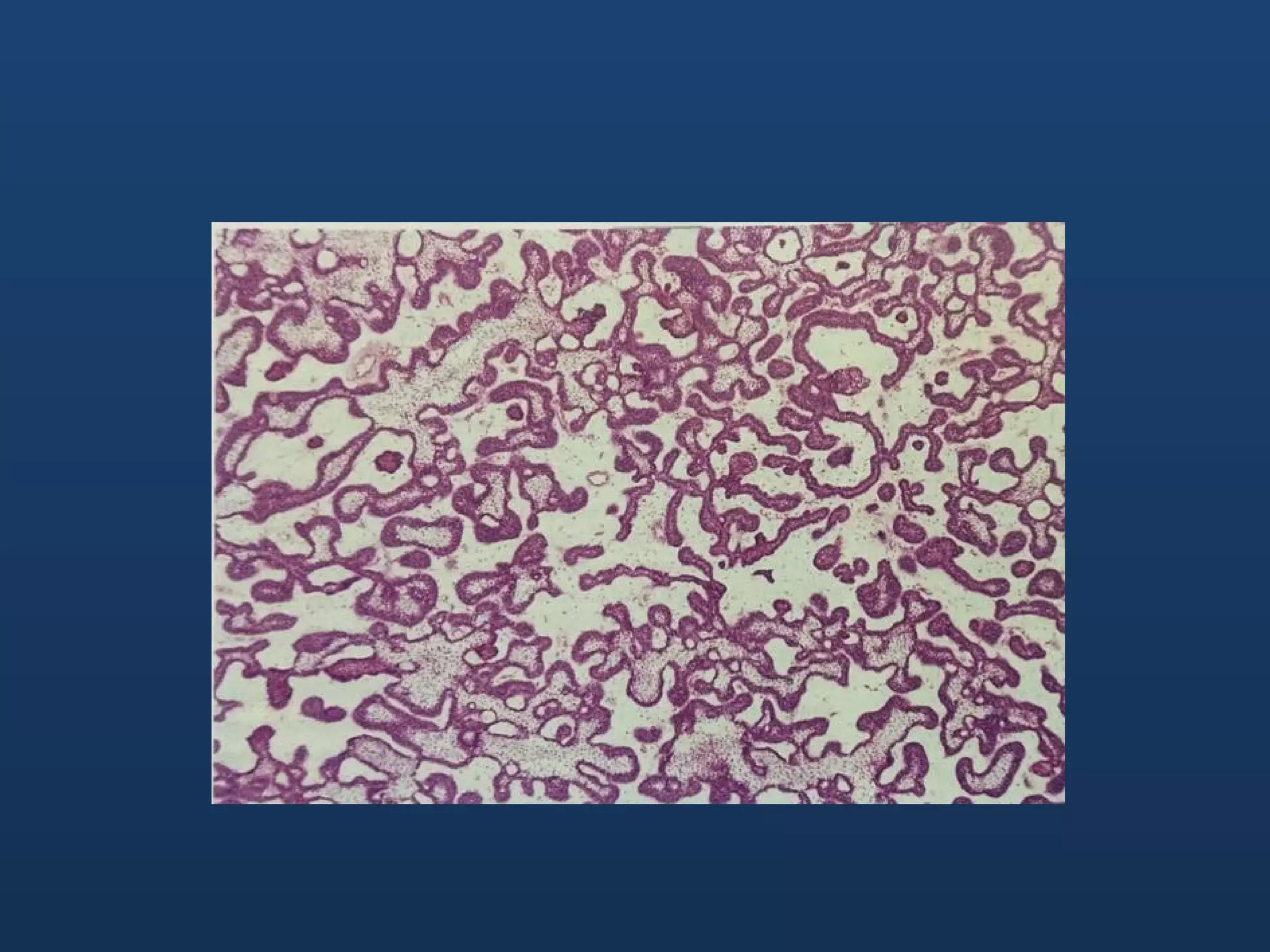
Odontogenic cysts and tumors originate from tooth-forming tissues. The most common cyst is the radicular cyst, which develops from inflammation around the root apex of a nonvital tooth. Dentigerous cysts encase the crown of an unerupted tooth. Odontogenic keratocyst is lined by keratinizing epithelium and has a high recurrence rate. Odontomas are benign odontogenic tumors composed of enamel and dentin. The most common odontogenic tumor is the ameloblastoma, which is locally invasive and has a high recurrence rate if not completely excised. Calcifying odontogenic tumor demonstrates epithelial cells and calcified material.