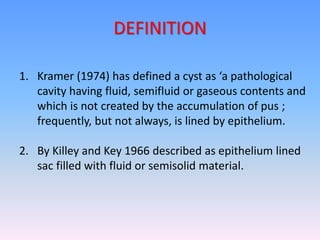
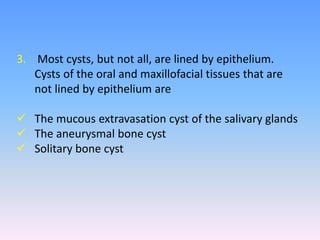
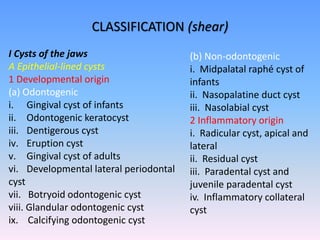
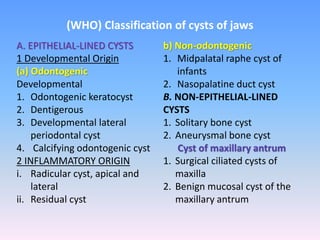
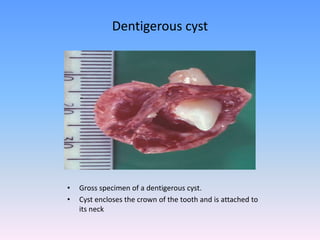
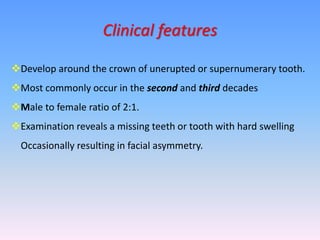
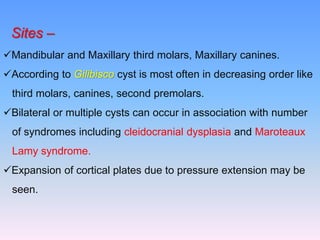
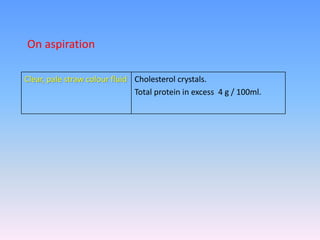
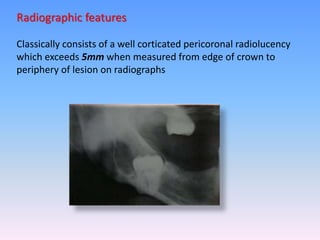
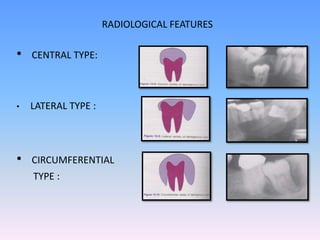
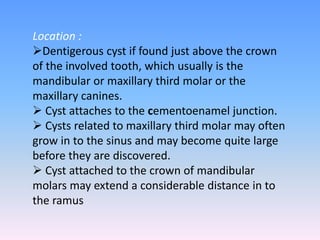
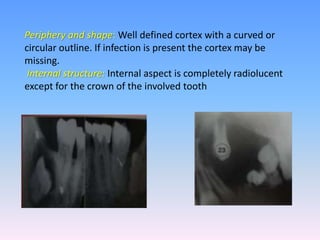
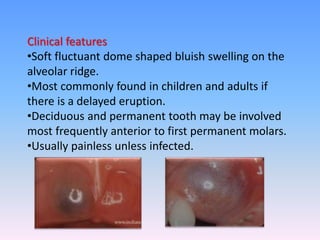
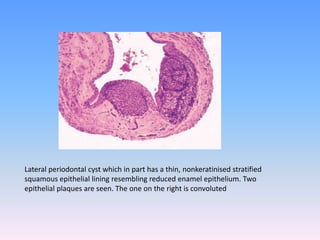
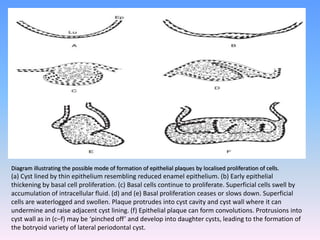
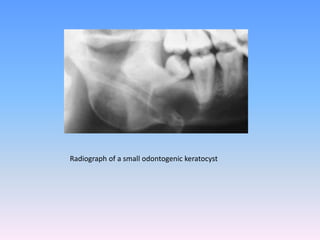
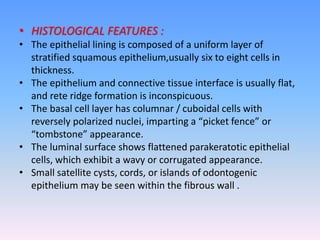
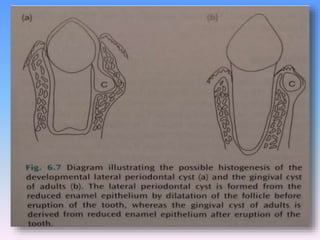
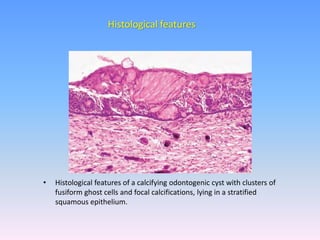
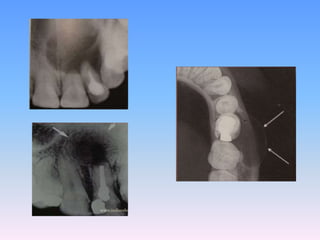
The document discusses various types of odontogenic cysts that develop in the jaws. It defines odontogenic cysts and provides classifications based on etiology and location. Key cysts discussed in detail include the dentigerous cyst, which forms around the crown of an unerupted tooth, and the lateral periodontal cyst, which occurs on the root surface of a vital tooth. For each cyst, the document outlines clinical features, radiographic appearance, histology, pathogenesis and treatment.