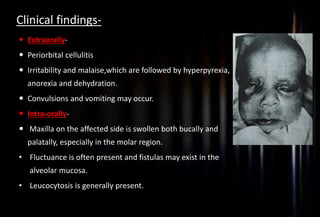
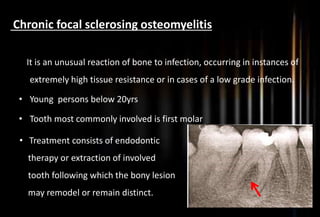
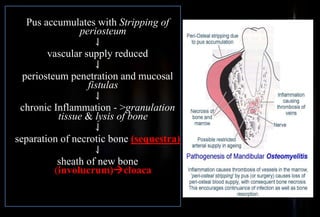
This document provides information about osteomyelitis and osteoradionecrosis of the jaws. It defines osteomyelitis as an inflammatory condition of bone that begins as an infection of the medullary cavity. Predisposing factors include fractures, radiation damage, and systemic diseases. Acute osteomyelitis is characterized by pain, fever, and identifiable cause, while chronic osteomyelitis involves fistulas and induration. Imaging techniques include radiography and scintigraphy. Treatment involves antibiotics, sequestrectomy, decortication, and reconstruction. Infantile osteomyelitis usually involves the maxilla and is treated with drainage and antibiotics.


















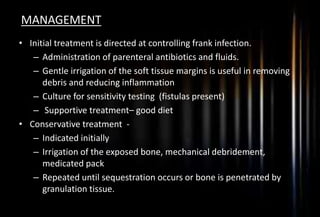
![MANAGEMENT
Conservative management
(Medical management)
Surgical management
[A] Conservative management
1. Complete bed rest
2. Supportive therapy (nutritional
support)
3. Rehydration
4. Blood transfusion (If RBC, Hb% are
low)
5. Control of Pain
Antibiotic therapy
-Systemic antibiotics
-Local antibiotic
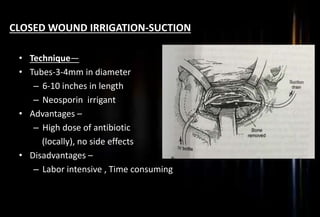
Closed wound irrigation – suction
Antibiotic impregnated beads
Hyperbaric oxygen therapy](https://image.slidesharecdn.com/mypptosteomyelitis-190307062600/85/Osteomyelitis-and-osteoradionecrosis-of-jaws-22-320.jpg)
![[B] Surgical management
1. Extraction of offending teeth
2. Incision and drainage
3. Sequestrectomy
4. Saucerisation
5. Decortication
6. Resection and Reconstruction
7. Post operative care](https://image.slidesharecdn.com/mypptosteomyelitis-190307062600/85/Osteomyelitis-and-osteoradionecrosis-of-jaws-23-320.jpg)