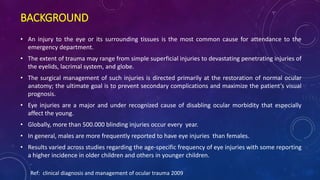
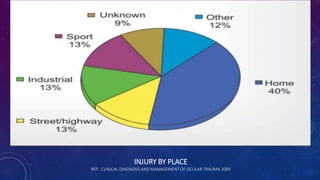
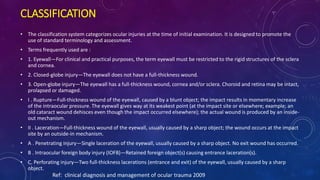
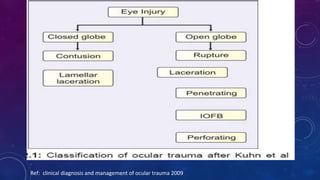
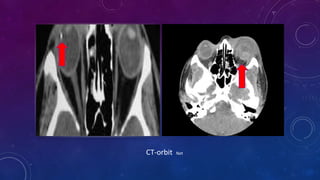
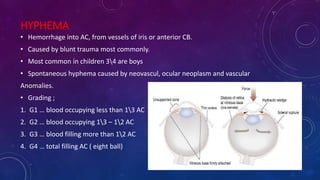
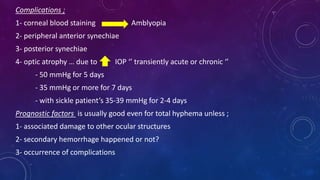
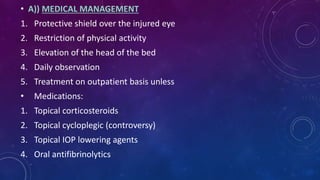
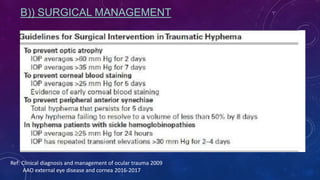
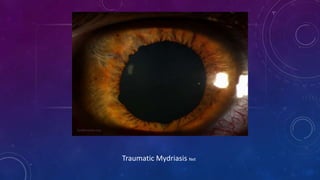
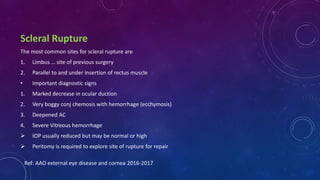
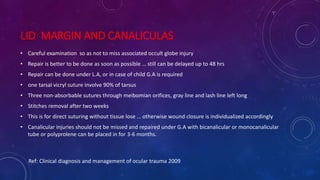
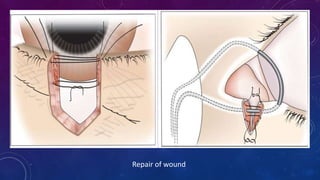
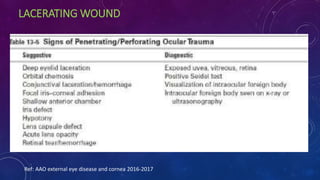
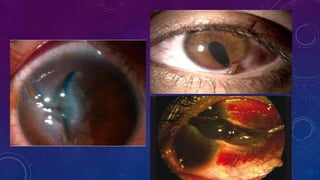
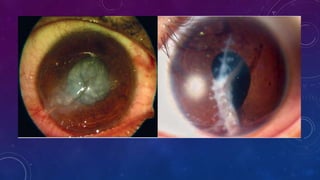
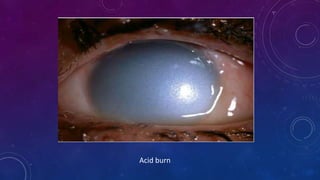
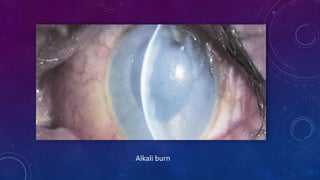
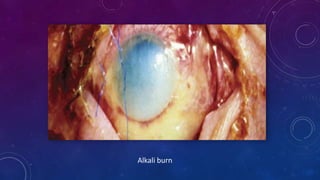
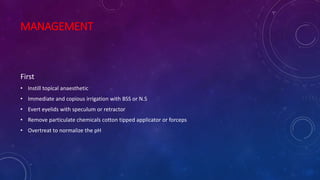
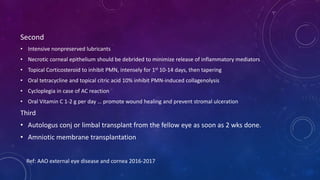
The document discusses ocular trauma, providing classifications and guidelines for clinical evaluation and management. It describes the epidemiology of eye injuries and classifications for closed and open globe injuries. Evaluation involves history, exam, and potential investigations. Closed injuries include contusions while open injuries include ruptures and lacerations. Management depends on the injury type and aims to repair anatomy and maximize vision. Chemical burns require copious irrigation and treatments to normalize pH.