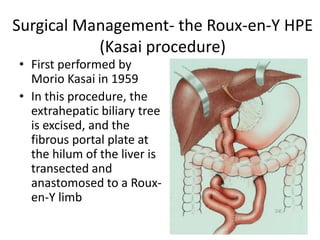
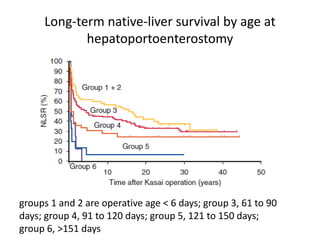
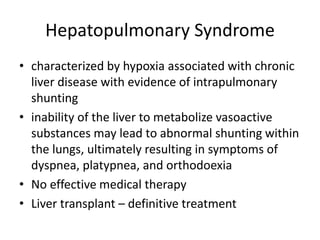
Biliary atresia is a progressive disease affecting the bile ducts in infants. It is the most common cause of liver transplantation in children. The Kasai procedure involves removing the damaged bile ducts and connecting the liver to the intestine to restore bile flow, but only half of patients achieve long-term native liver survival. Even after a successful Kasai procedure, patients remain at risk of complications like cholangitis, portal hypertension, and hepatopulmonary syndrome that may eventually require liver transplantation.