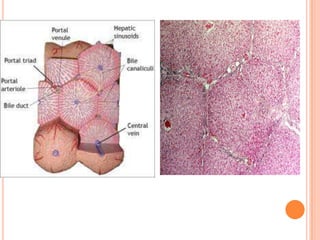
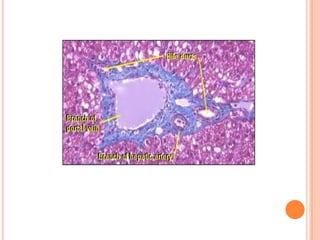
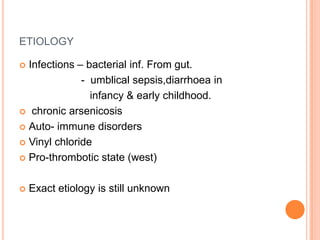
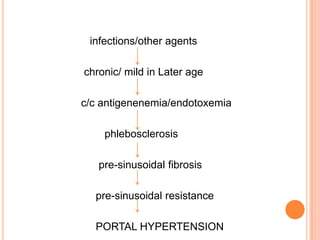
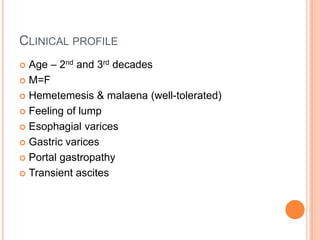
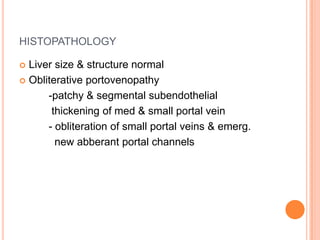
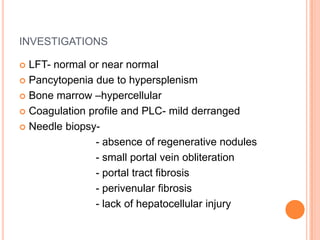
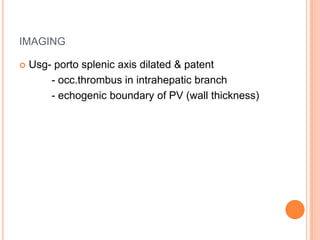
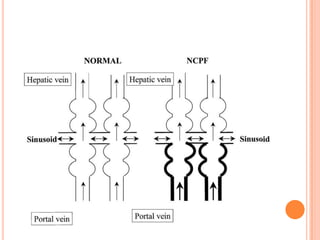
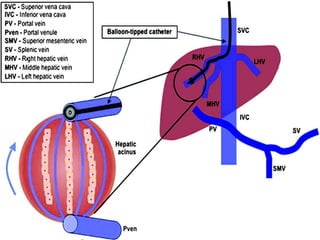
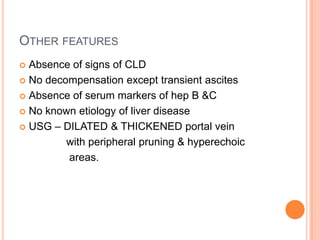
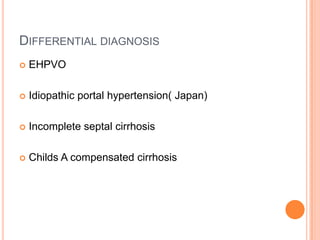
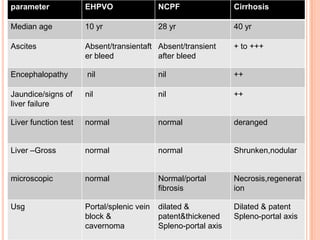
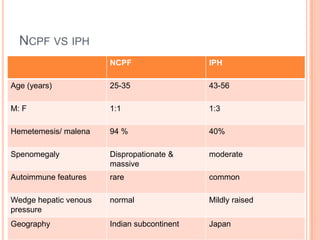
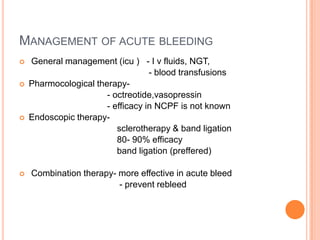
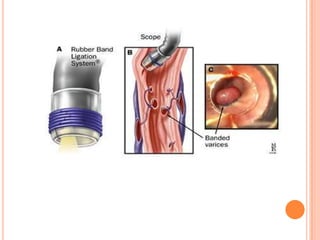
NCPF is a condition characterized by portal fibrosis and involvement of small and medium portal veins, leading to portal hypertension and splenomegaly despite normal liver function and structure. It commonly affects individuals in the Indian subcontinent aged 25-35 years from low socioeconomic backgrounds. Diagnosis involves evidence of portal hypertension and varices with normal liver function tests and histology showing obliteration of small portal veins without cirrhosis or injury. Management focuses on treatment and prevention of variceal bleeding through endoscopic therapies and beta blockers, with an otherwise excellent prognosis.