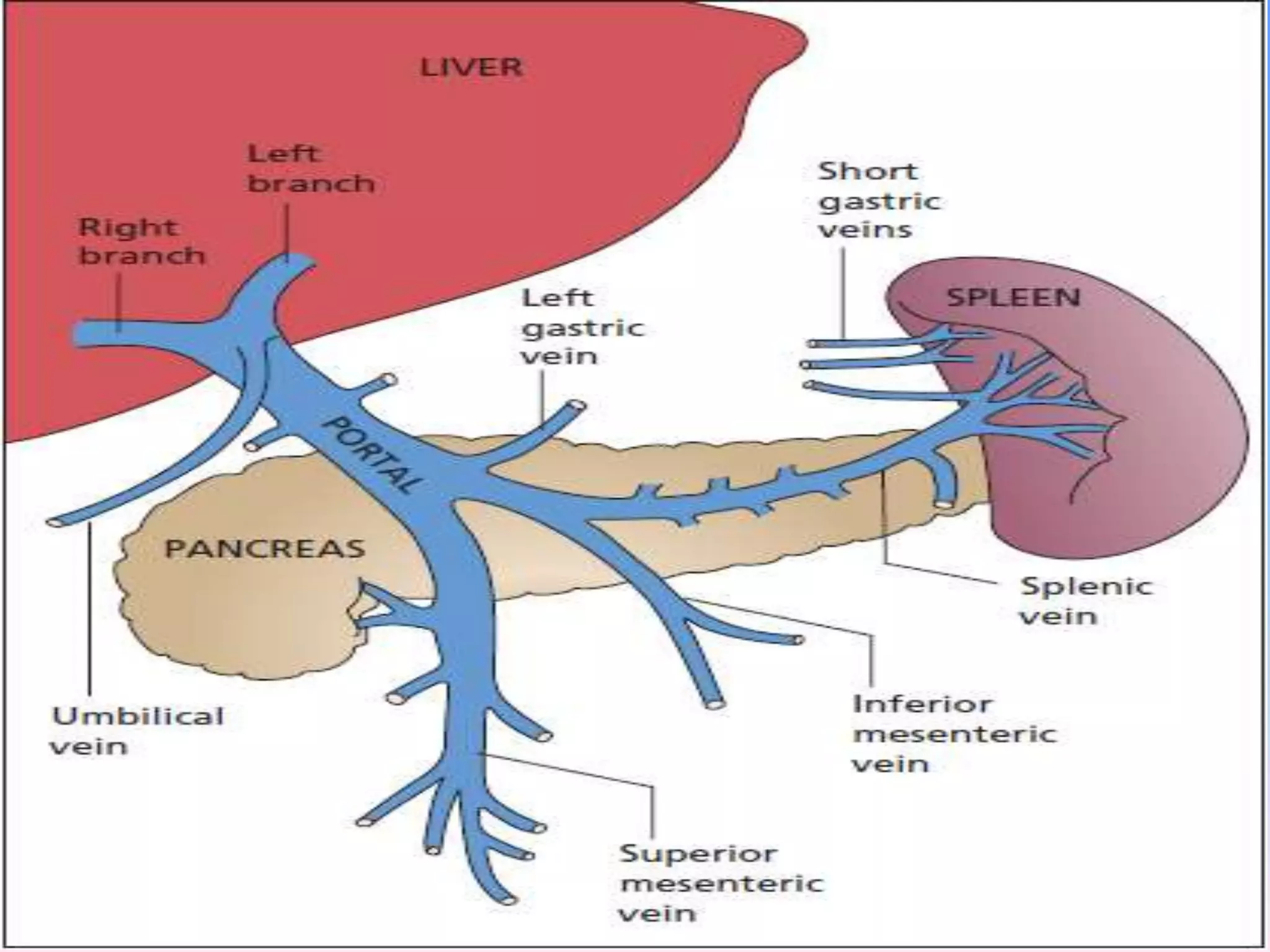
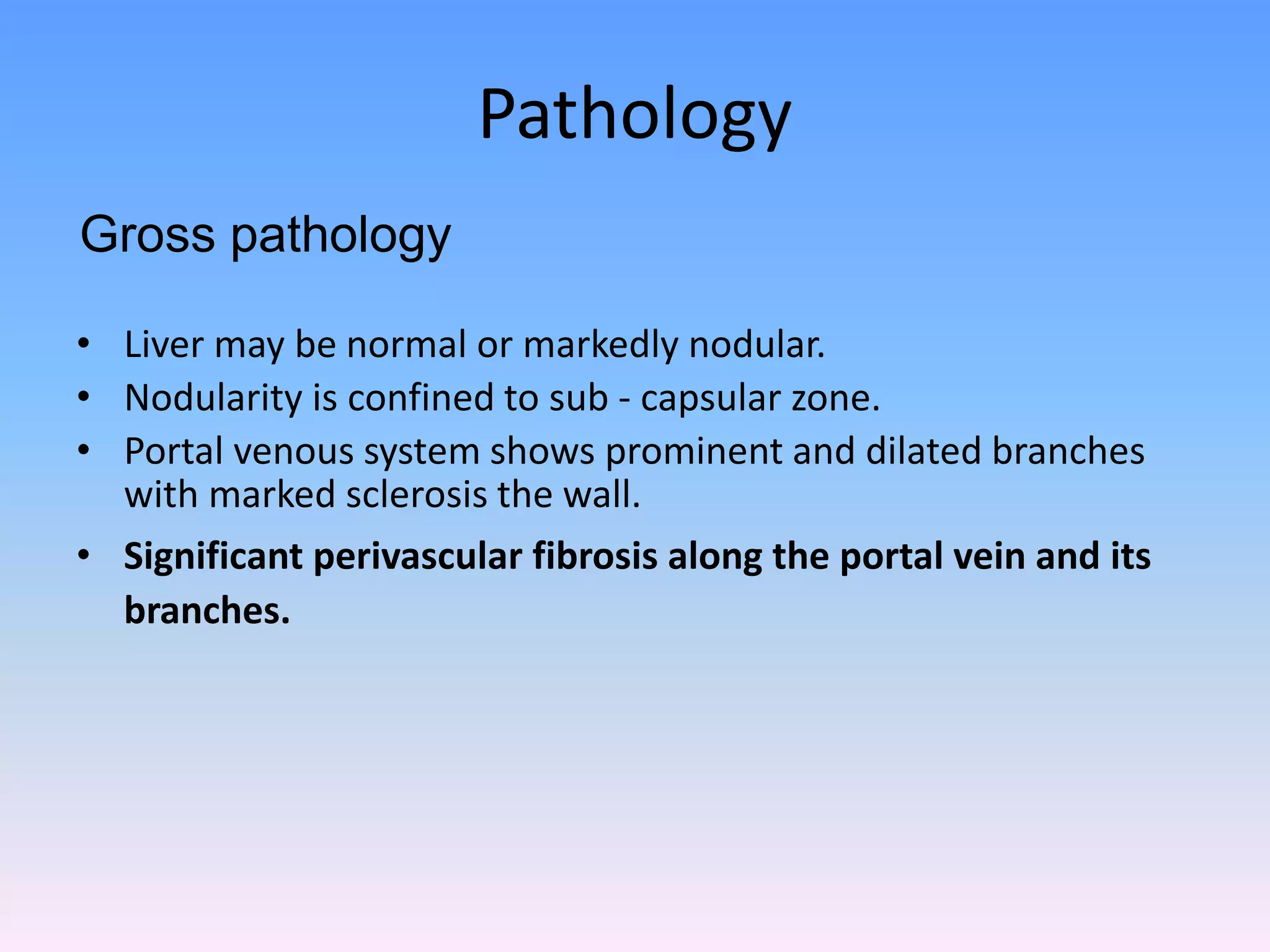
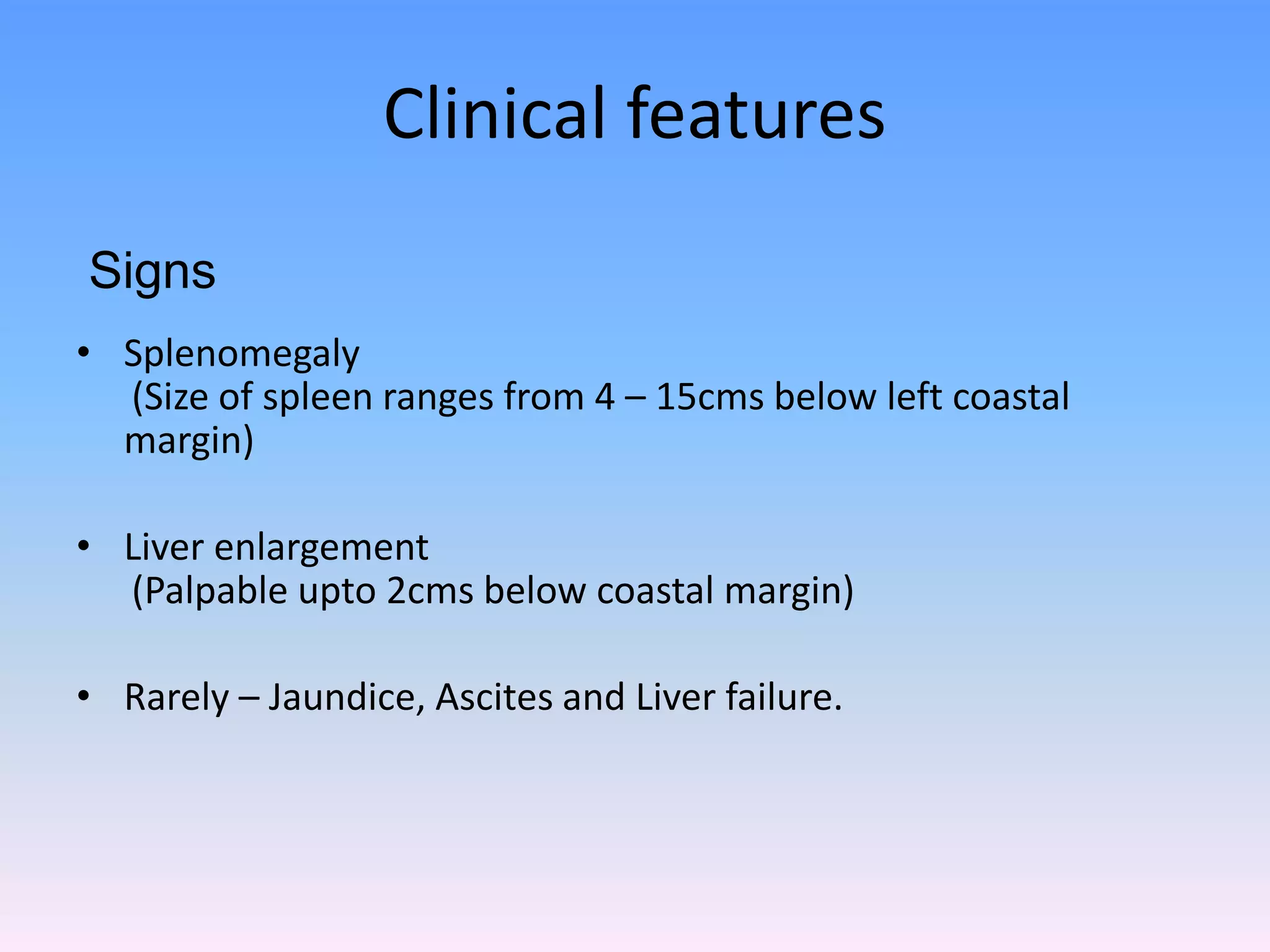
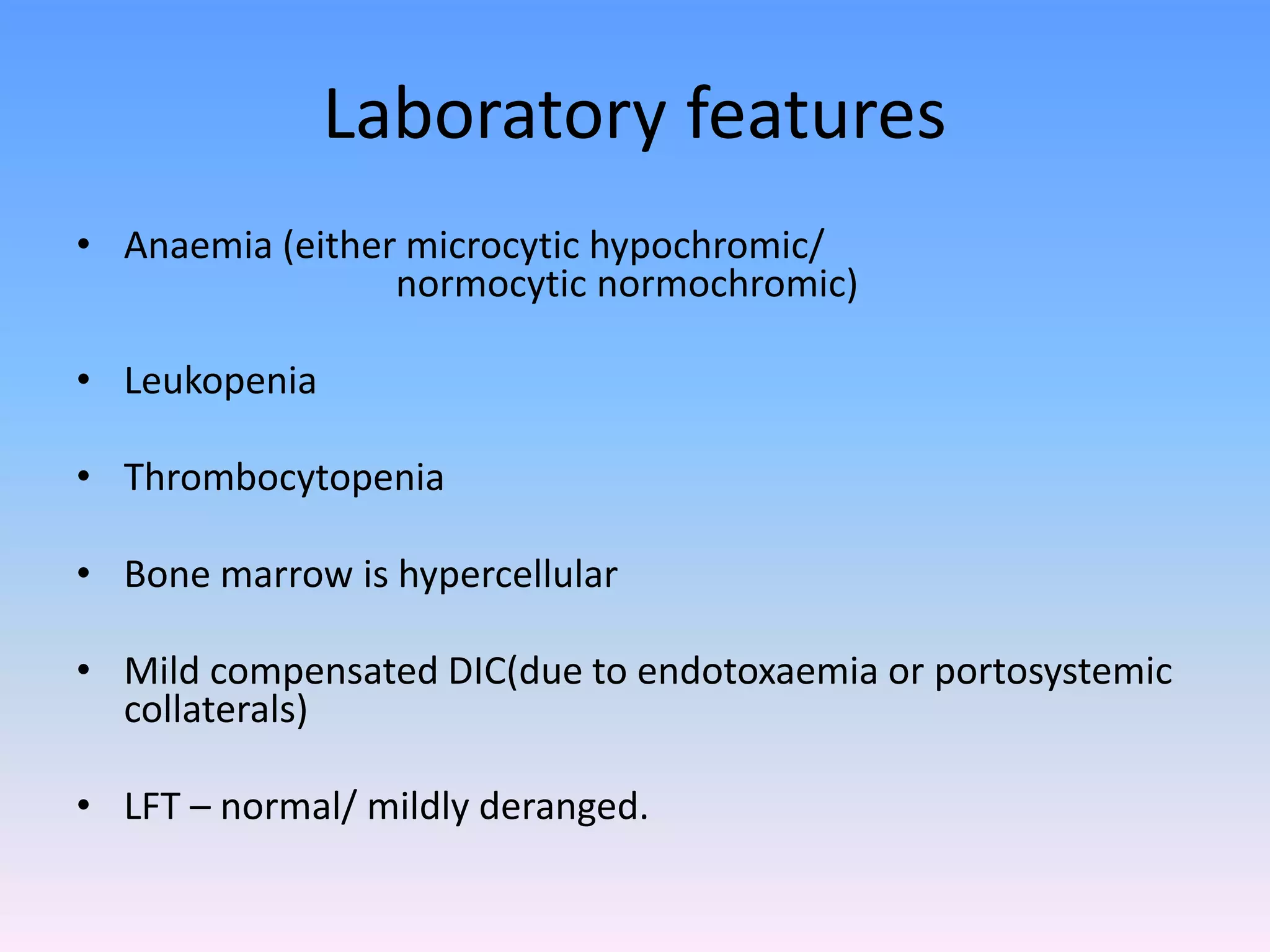
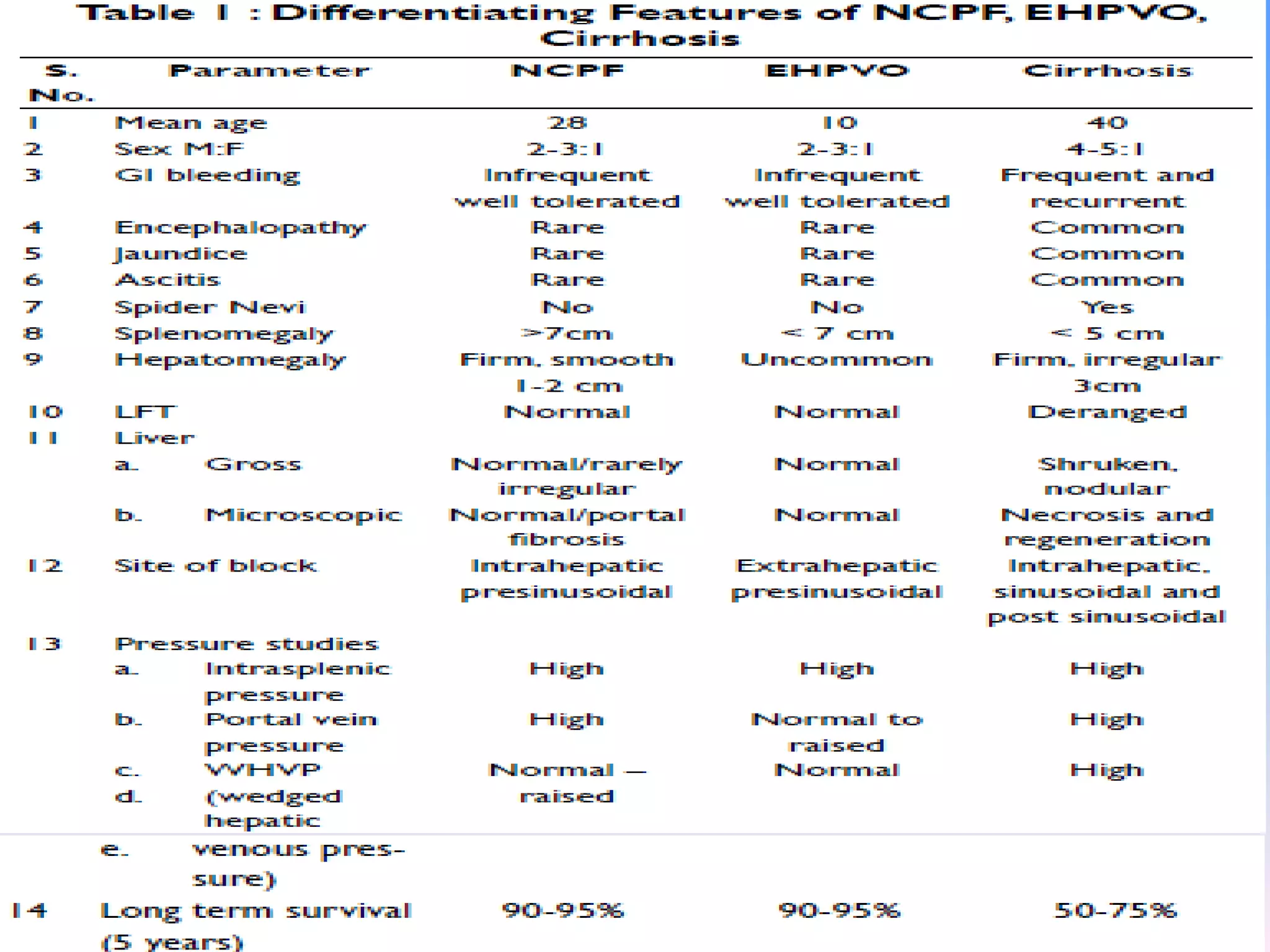
Non Cirrhotic Portal Fibrosis (NCPF) is a syndrome of obscure etiology characterized by obliterative portovenopathy leading to portal hypertension and massive splenomegaly in young adults from low socioeconomic backgrounds. The exact cause is unknown but is hypothesized to be related to malnutrition, recurrent infections, exposure to toxins or metals. Pathology shows sclerosis of portal vein branches. Clinical features include gastrointestinal bleeding, splenomegaly, and abdominal pain. Management involves controlling acute bleeding episodes and preventing rebleeding through medications or surgery like portosystemic shunts. Prognosis is generally good if bleeding can be controlled.