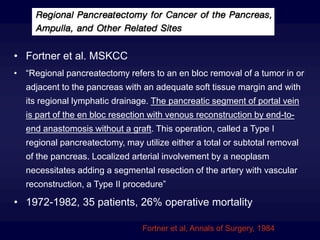
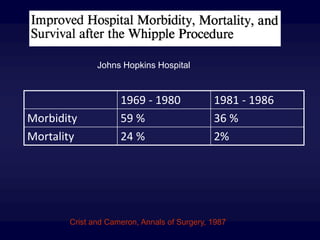
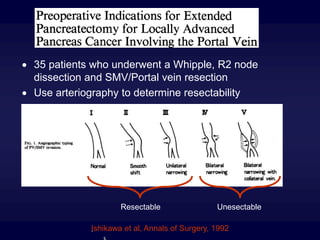
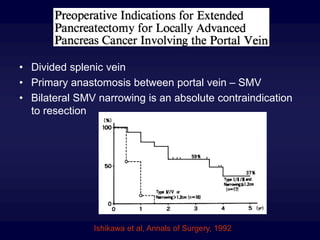
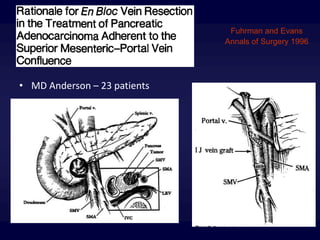
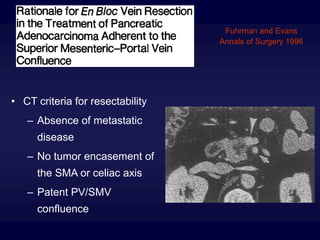
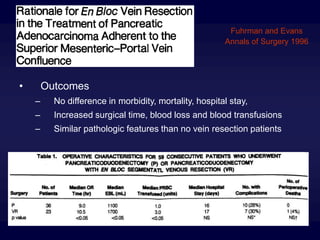
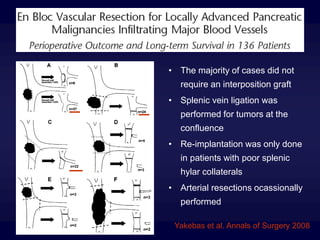
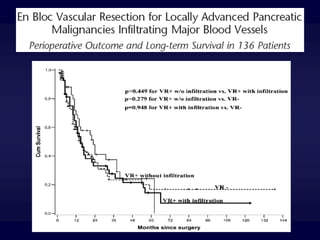
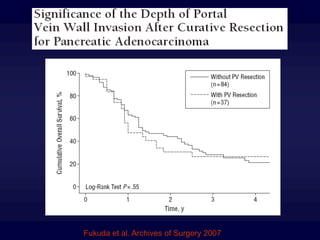
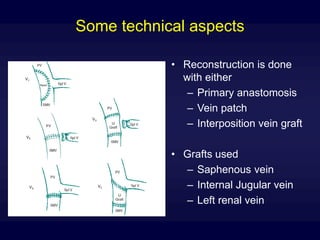
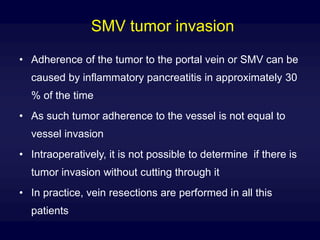
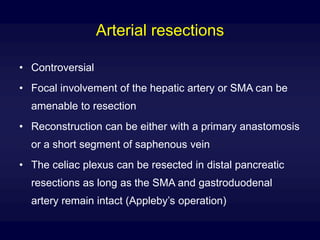
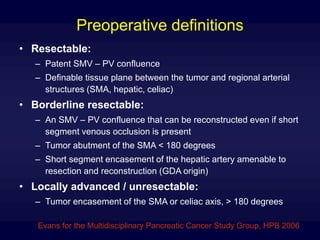
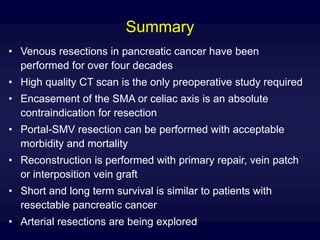
Venous resections of the portal or superior mesenteric vein have been performed during pancreatic cancer surgery for over 40 years. While initially performed to enhance nodal harvest, contemporary data shows that portal-superior mesenteric vein resection can be performed with acceptable morbidity and mortality when needed to achieve a negative margin resection. Preoperative imaging with CT scan is sufficient to determine resectability in most cases. Encasement of the celiac axis or superior mesenteric artery over 180 degrees remains a contraindication. With advances in surgical techniques and postoperative care, vascular reconstruction after venous resection now allows for long term survival similar to upfront resectable pancreatic cancer.