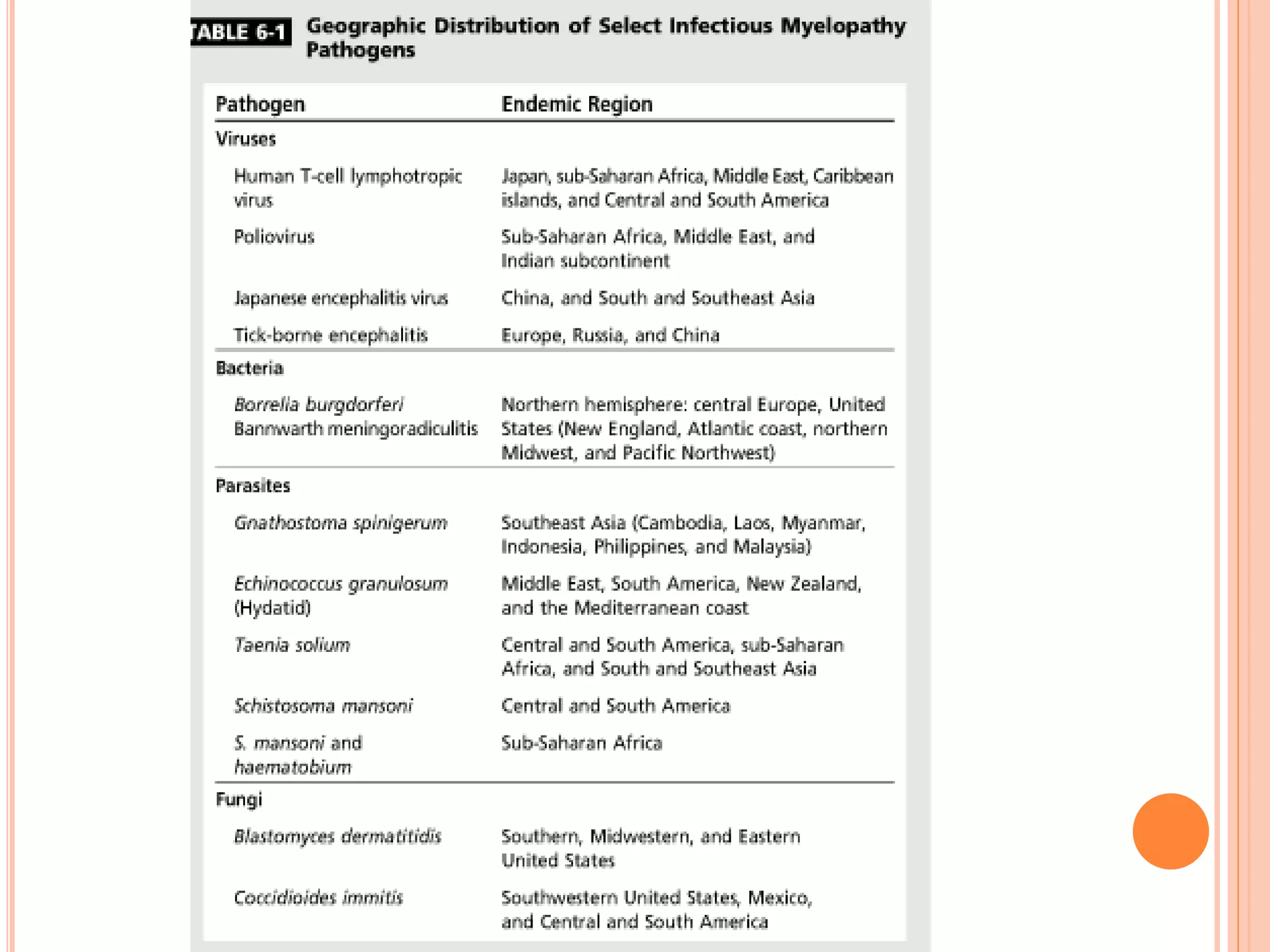
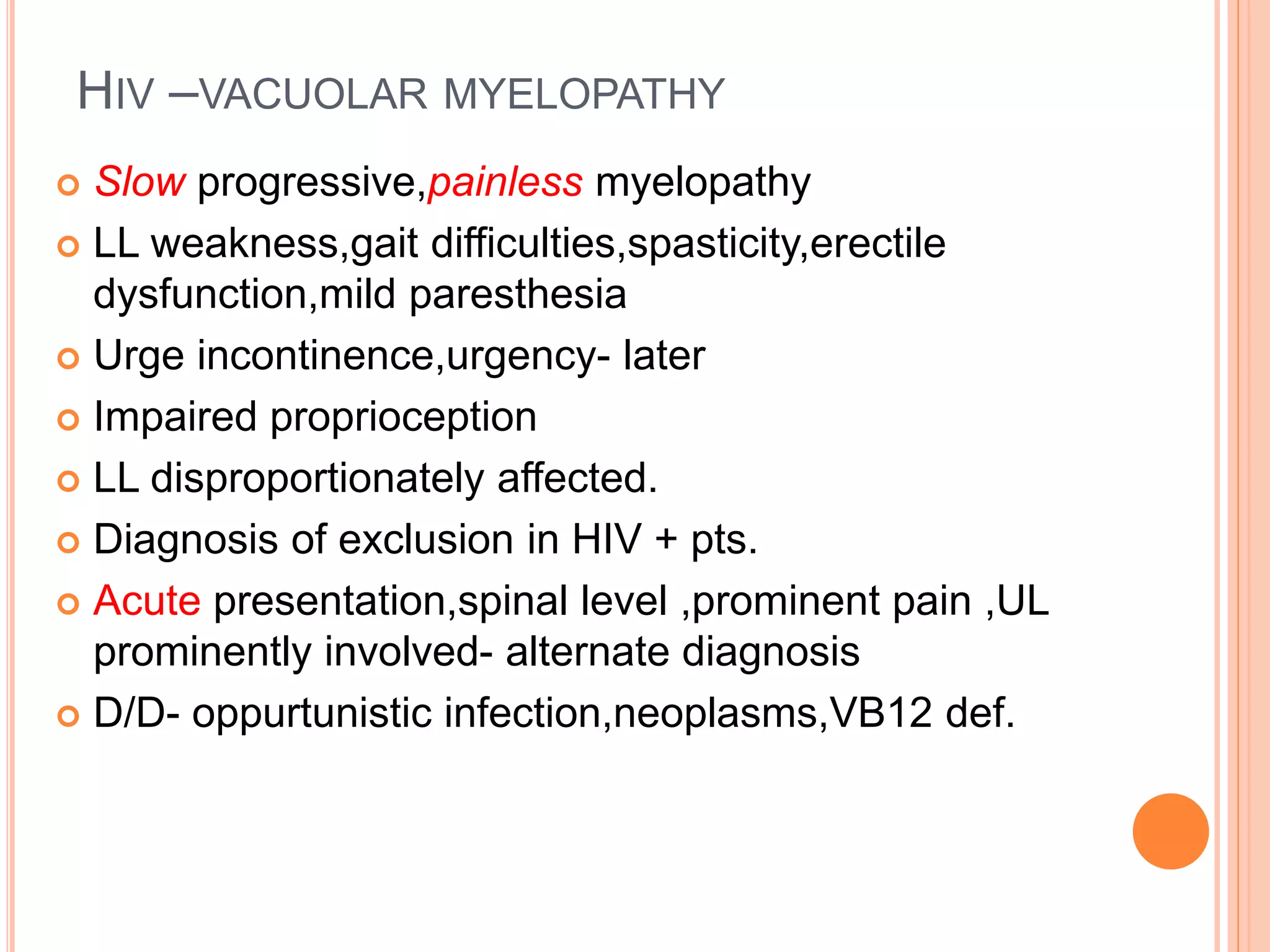
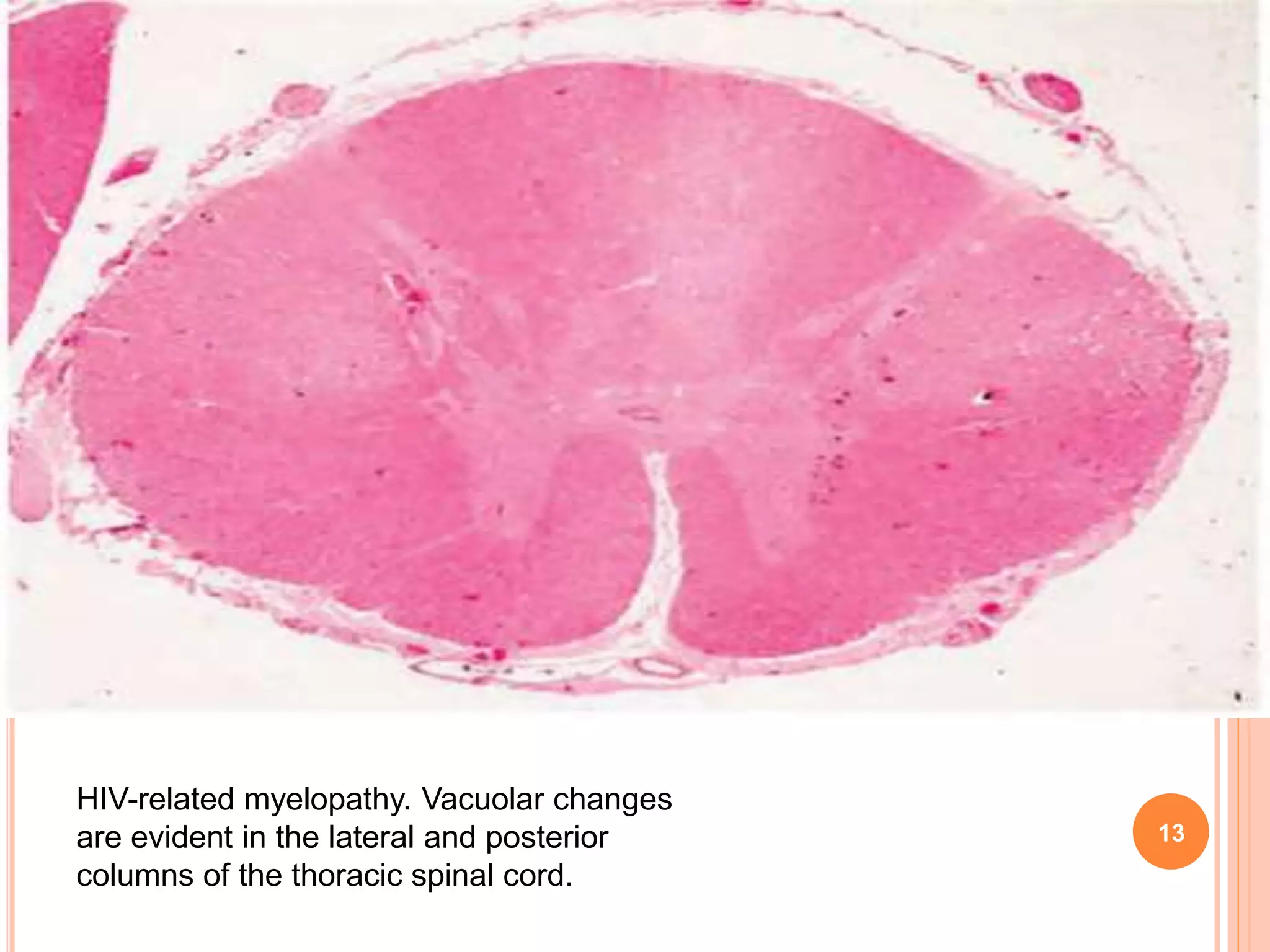
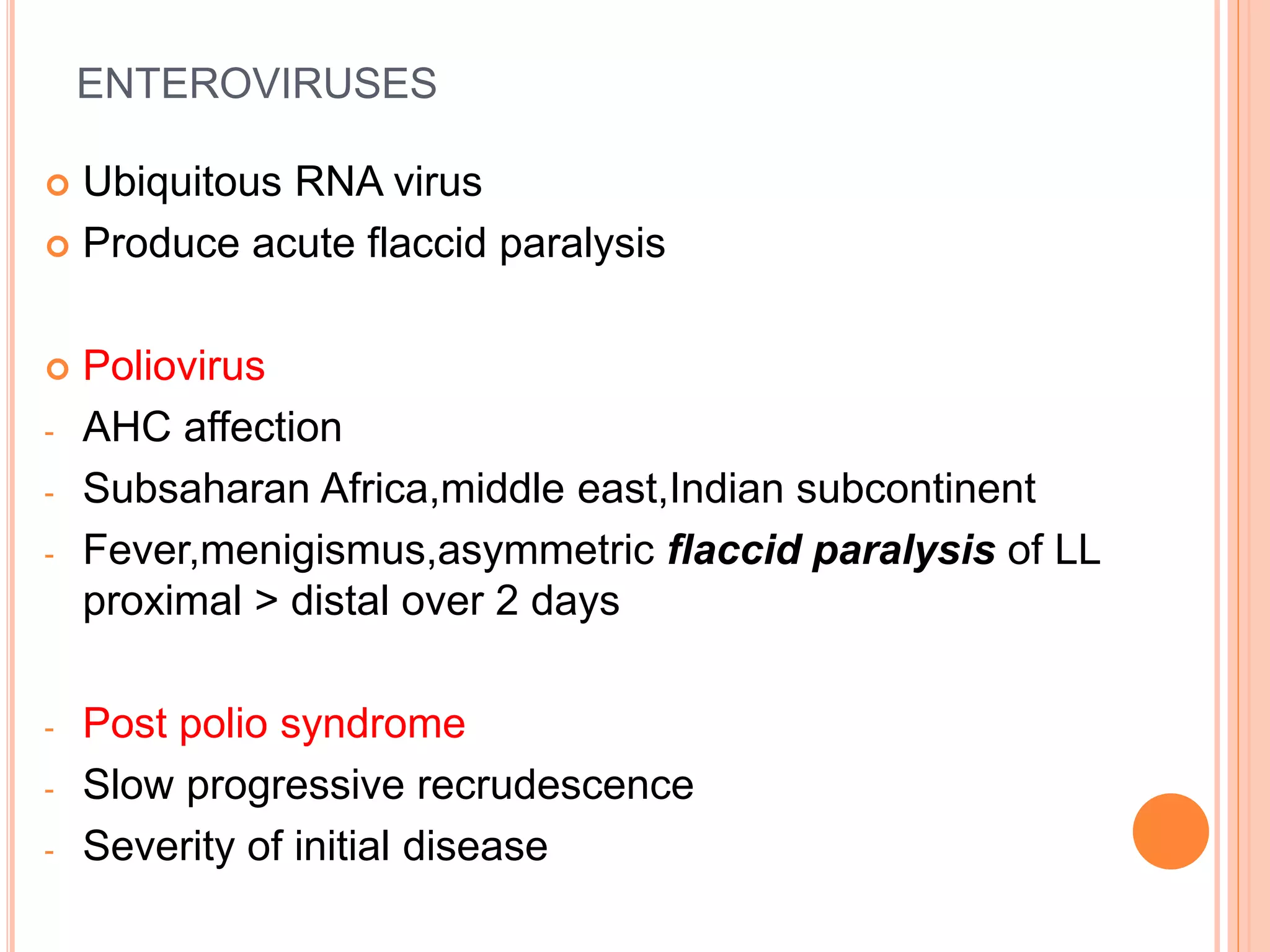
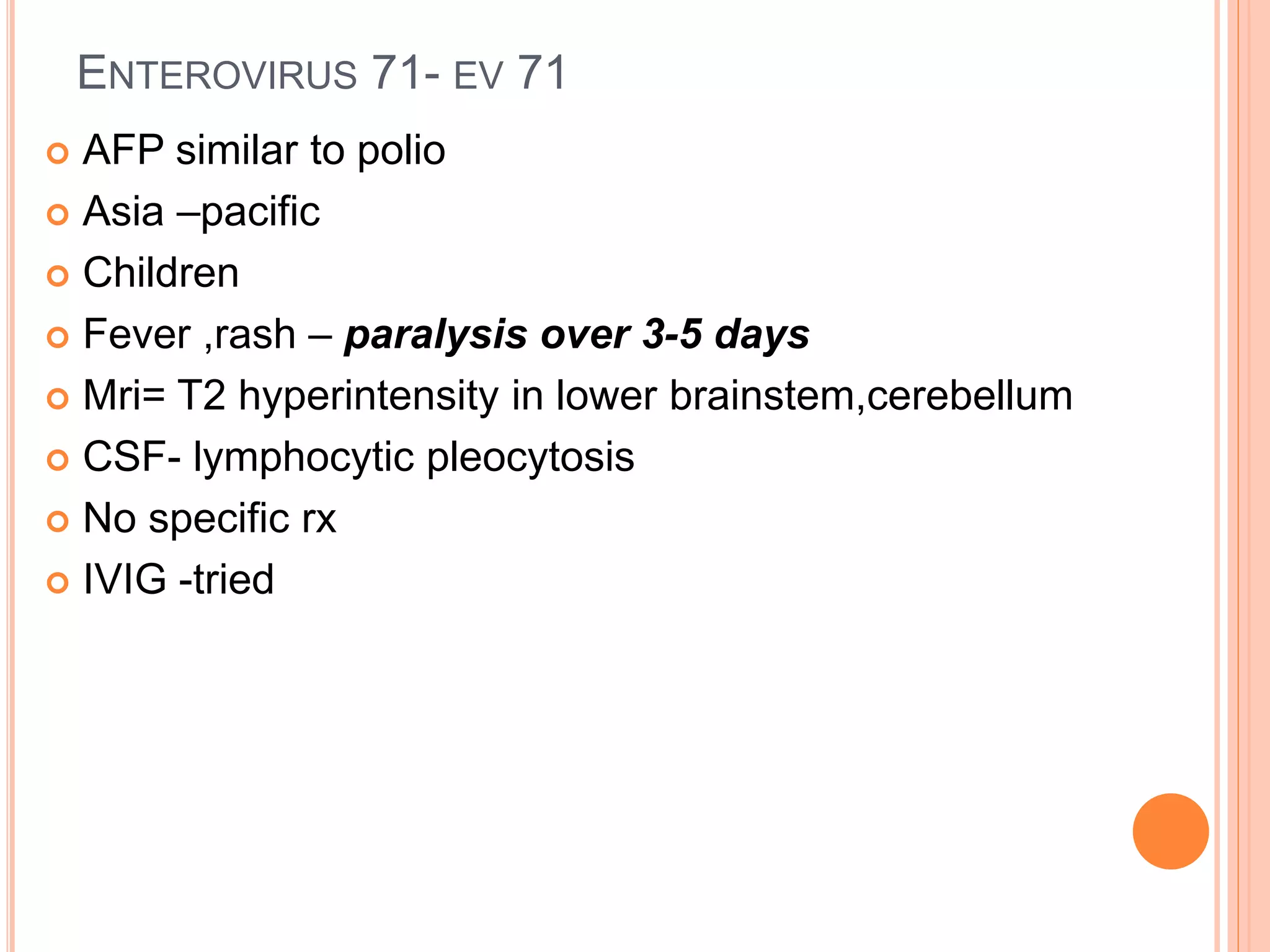
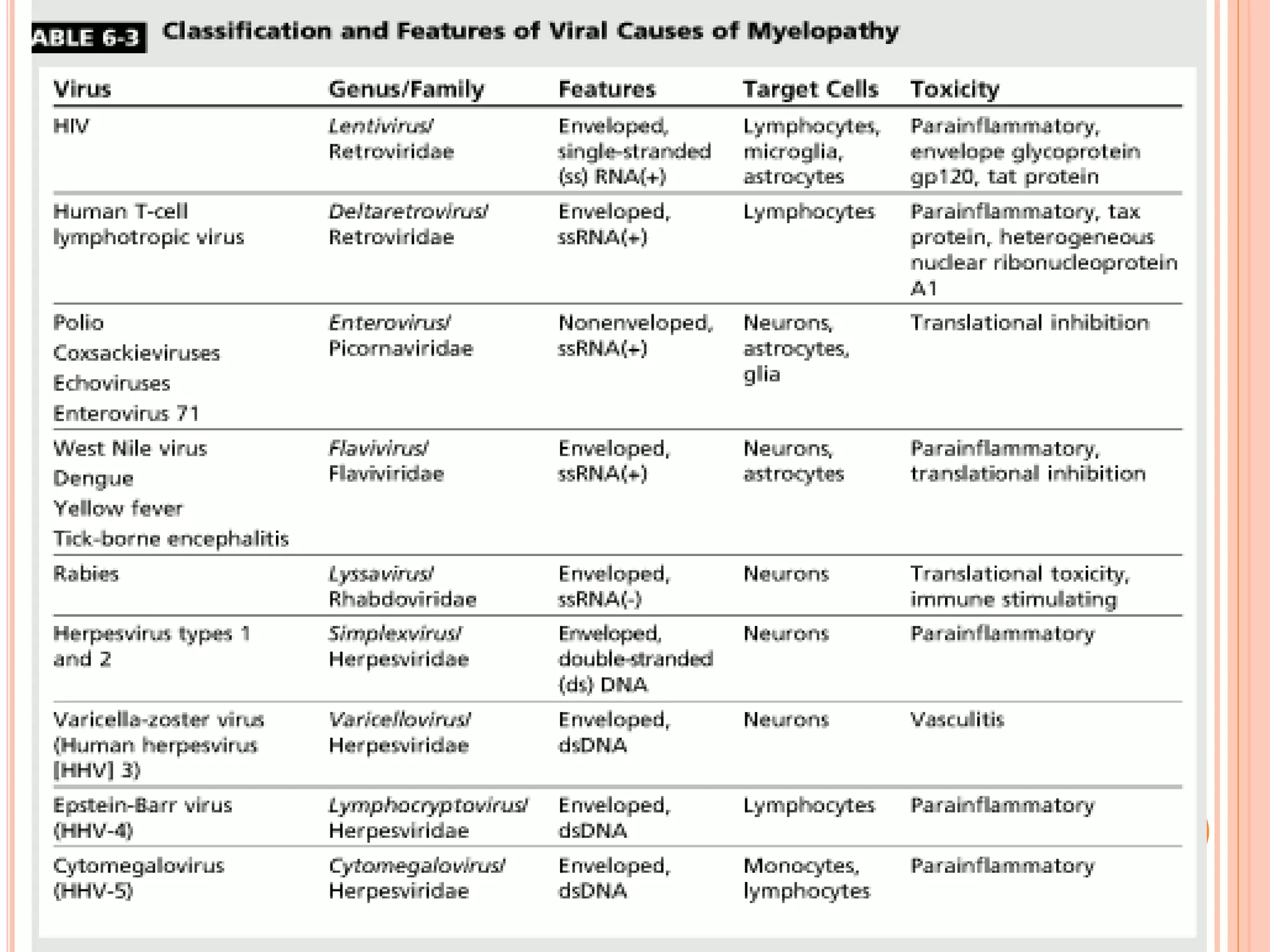
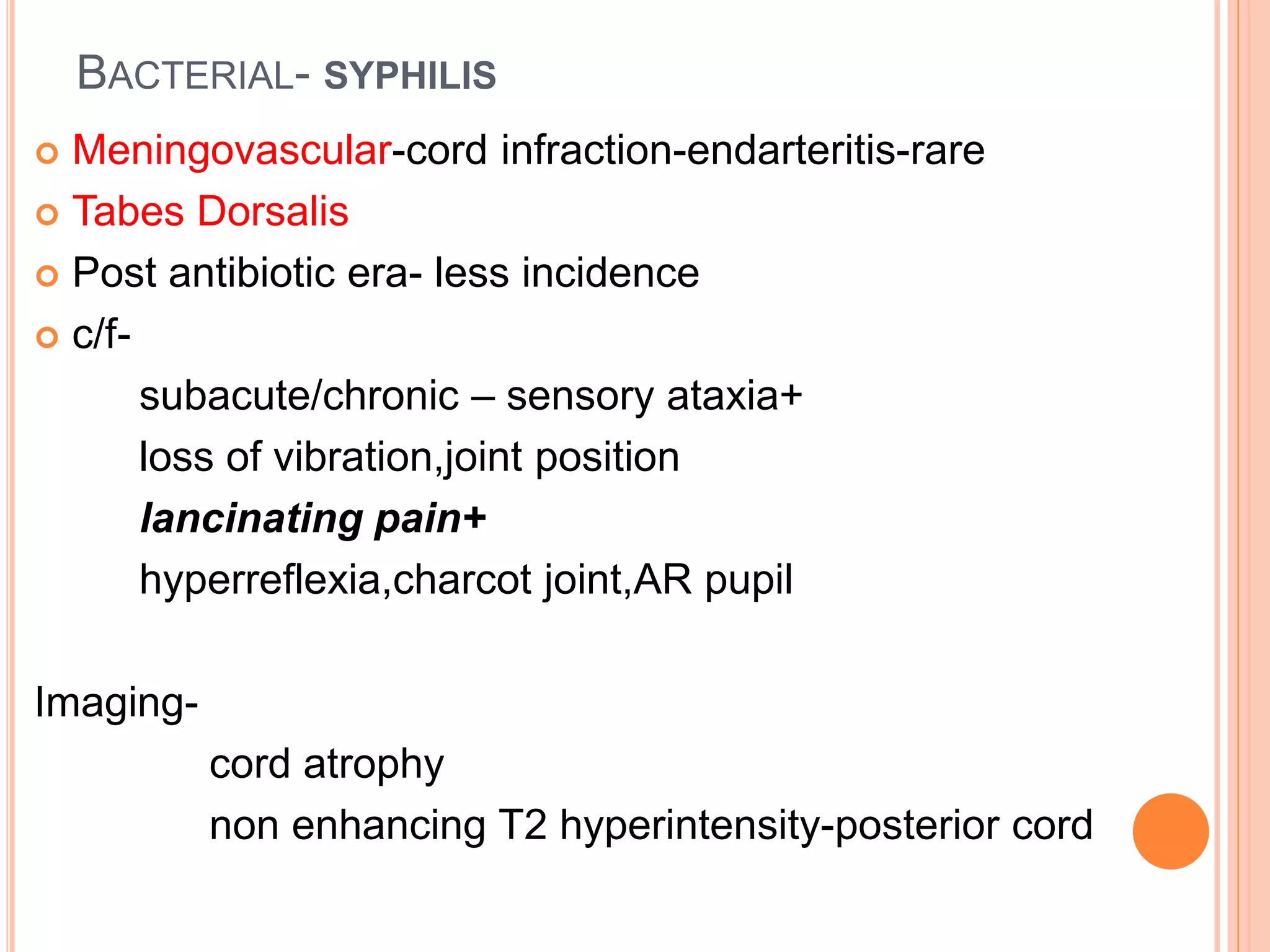
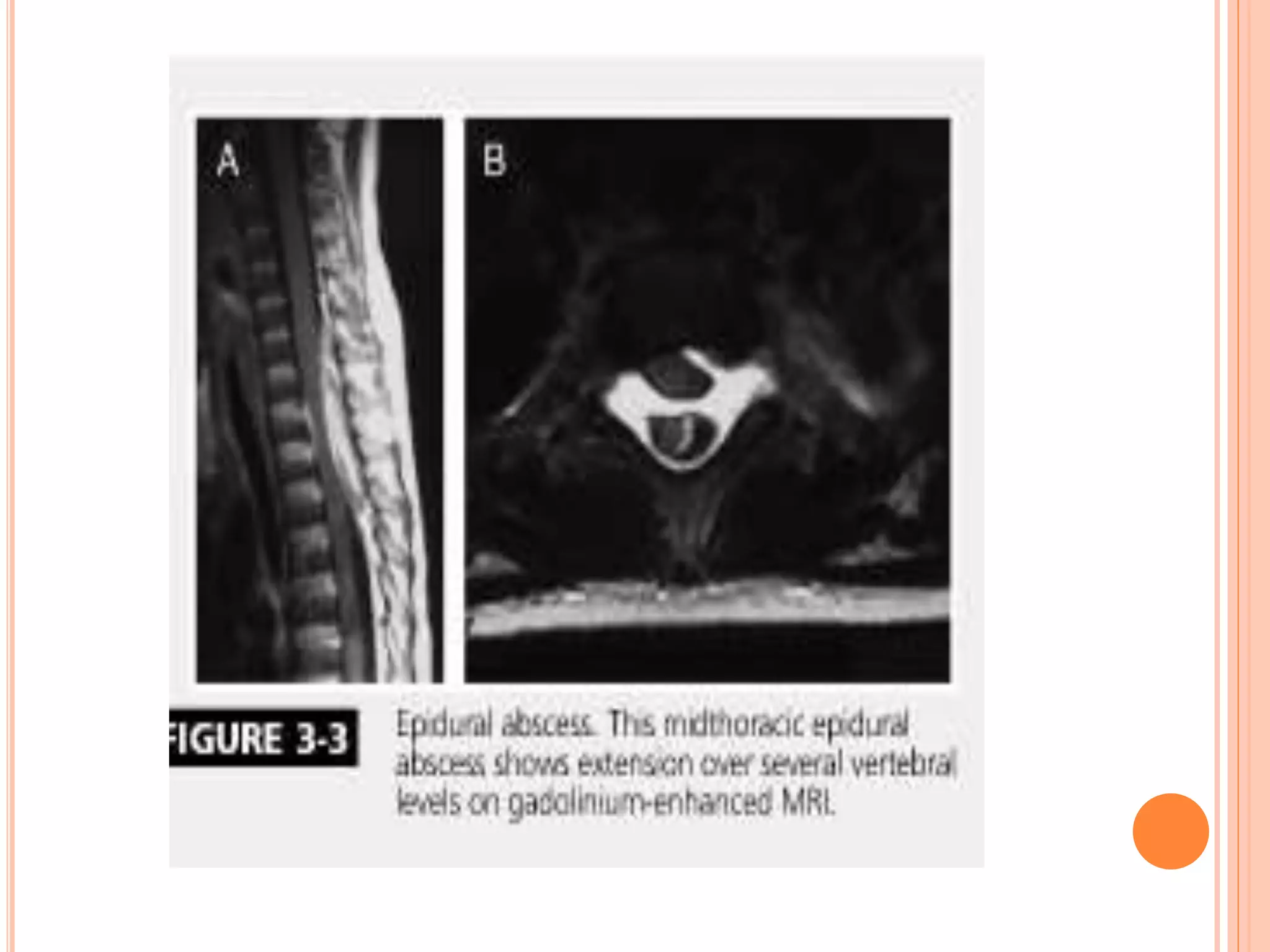
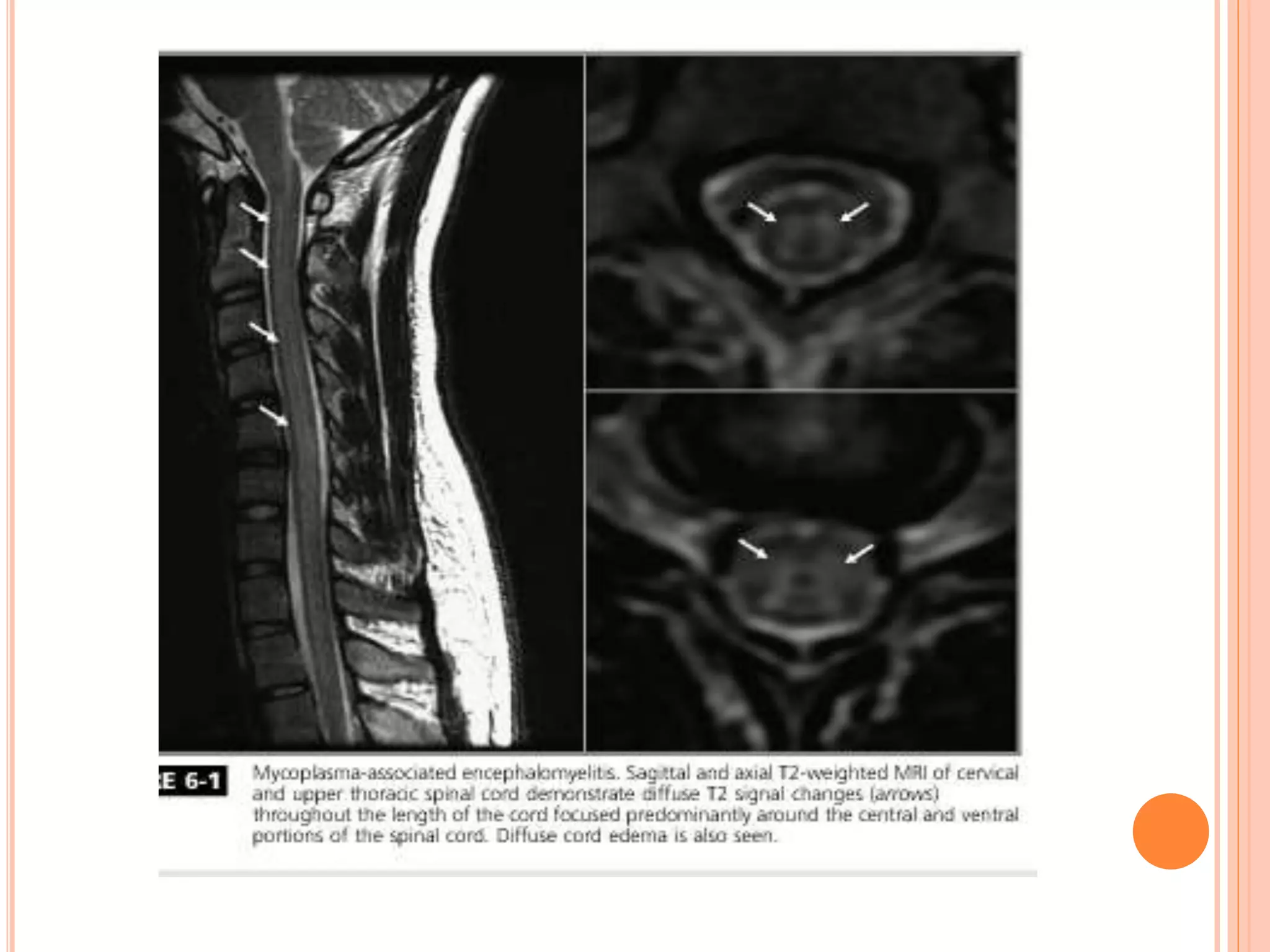
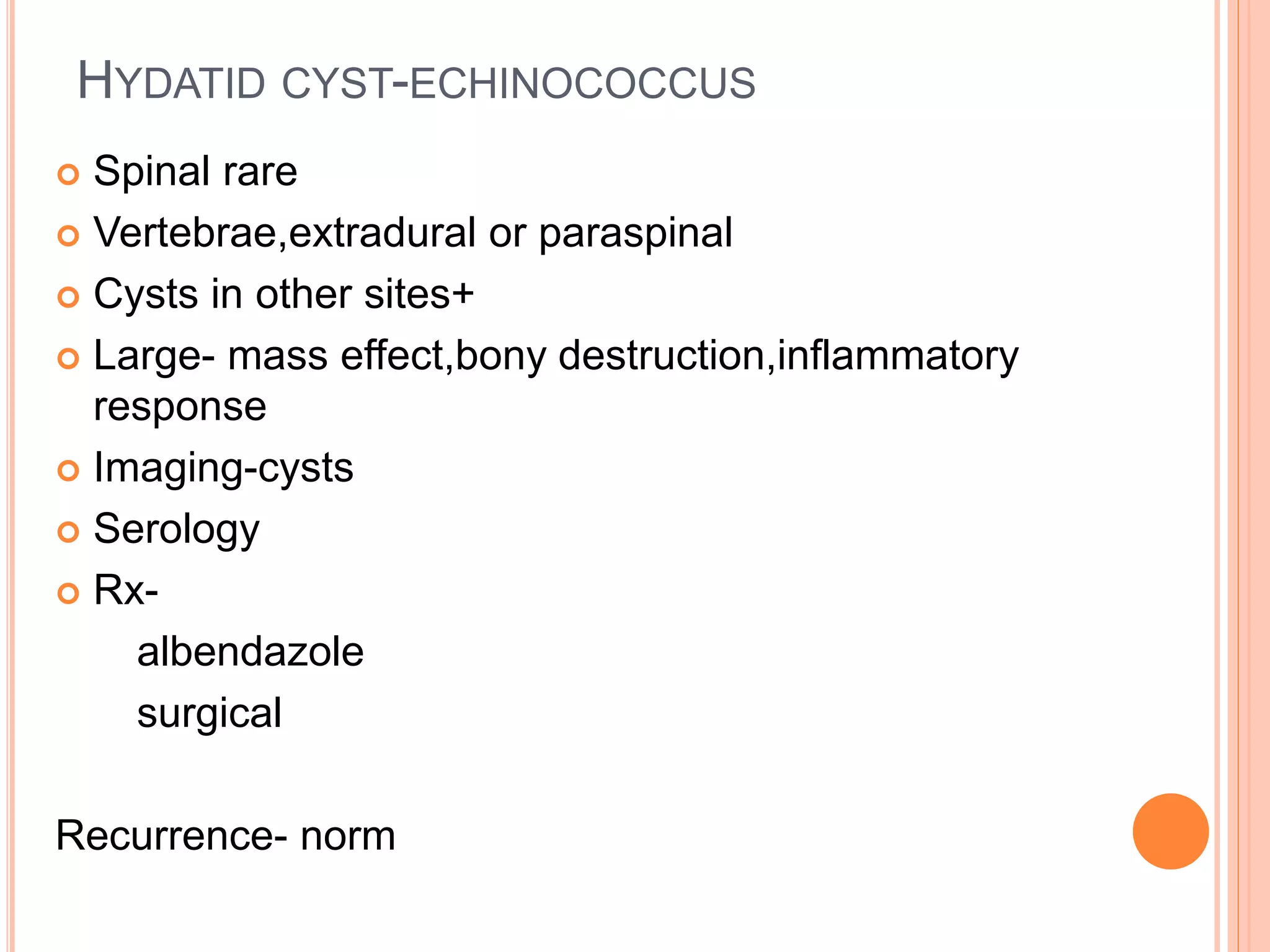
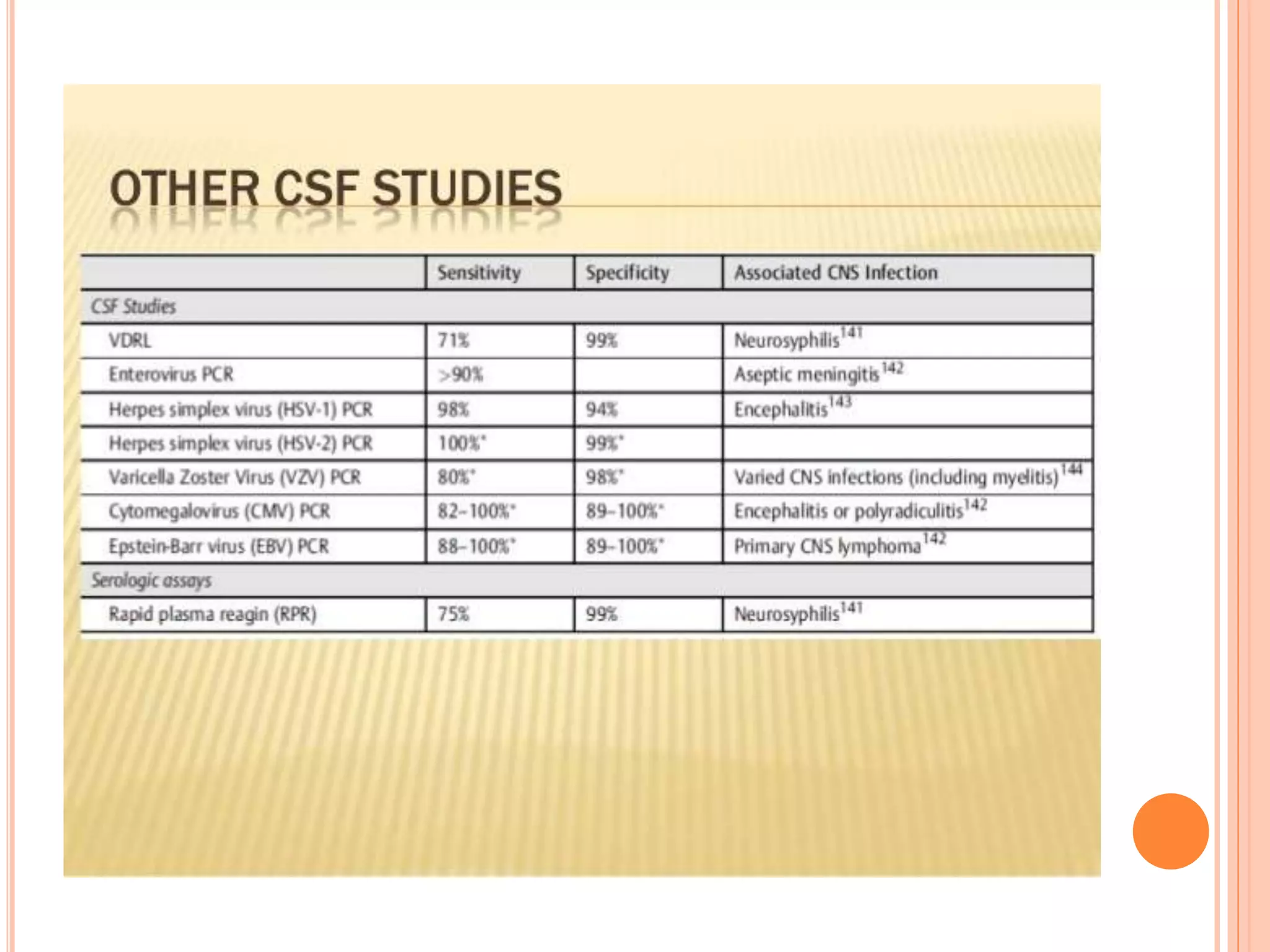
This document discusses various infectious causes of myelopathy or spinal cord dysfunction. It covers viral, bacterial, parasitic and fungal pathogens that can directly invade or cause inflammatory changes in the spinal cord. Key points include discussions of viruses like HIV, HTLV-1, poliovirus, West Nile virus and herpes viruses as well as bacteria like syphilis, tuberculosis, Lyme disease and pyogenic organisms. Parasitic infections involving the spinal cord from organisms such as schistosomiasis, toxoplasmosis and neurocysticercosis are also outlined. Clinical presentations, diagnostic approaches and treatment options are provided for many of the infectious etiologies of myelopathy.