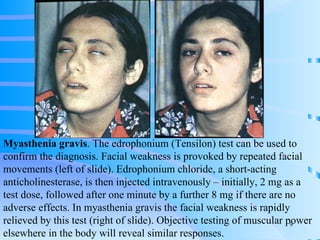
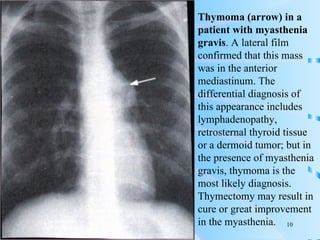
Neuromuscular junction diseases interfere with the transmission of signals from nerves to muscles and can be acquired or inherited. Myasthenia gravis is an acquired autoimmune disorder where antibodies induce acetylcholine receptor deficiency at the neuromuscular junction, causing weakness that fluctuates with activity. Symptoms are tested using drugs like edrophonium, and treatment includes anticholinesterases, immunosuppressants, thymectomy, and plasmapheresis. Lambert-Eaton myasthenic syndrome is another autoimmune condition where antibodies affect calcium channels, and is associated with lung cancer. Certain drugs can also induce myasthenic syndrome symptoms.