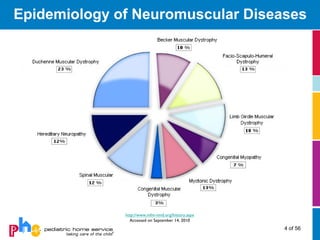
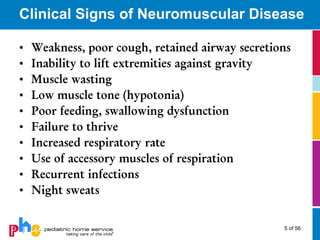
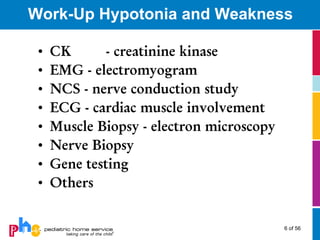
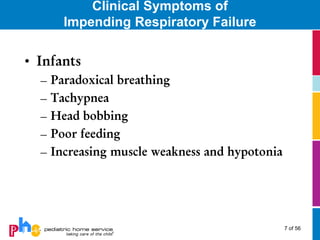
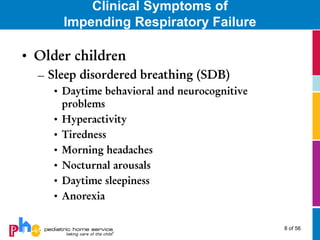
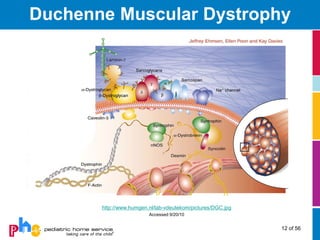
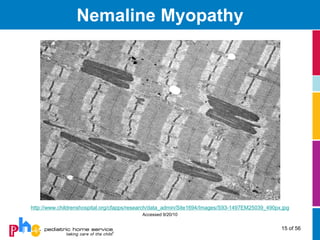
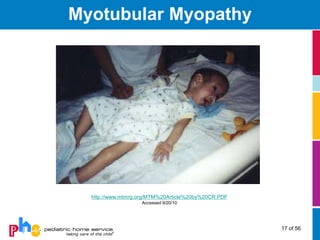
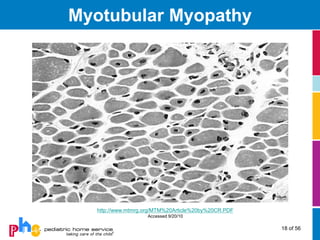
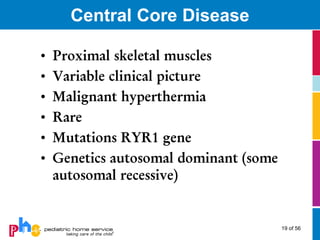
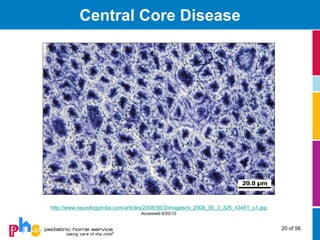
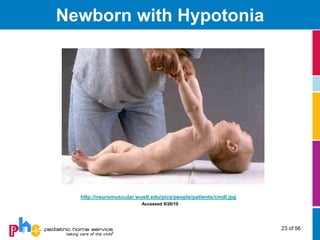
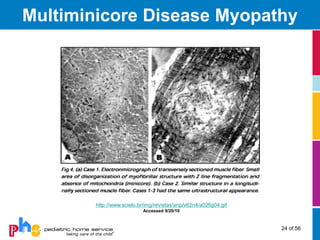
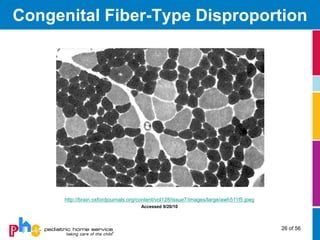
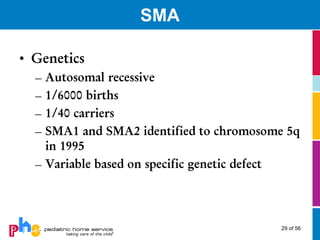
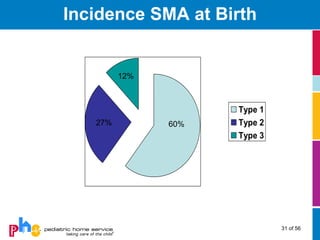
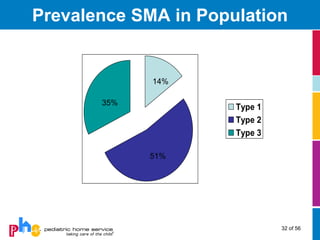
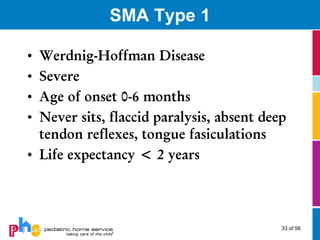
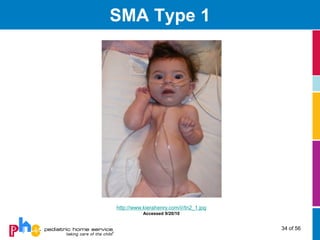
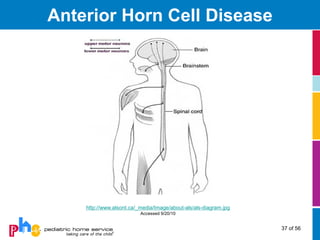
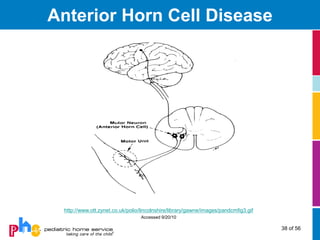
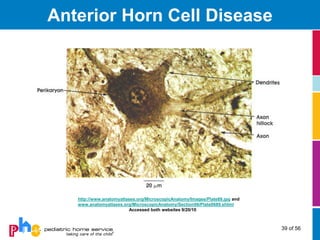
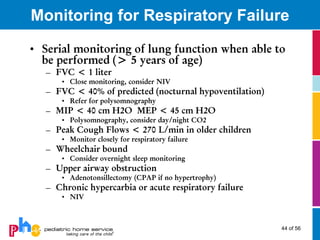
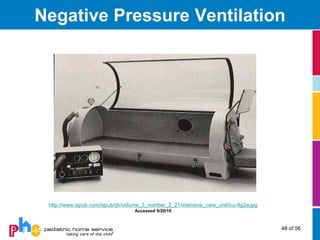
This document provides an overview of neuromuscular diseases, including classifications, signs and symptoms, and details on specific conditions. It covers muscular dystrophies like Duchenne, congenital myopathies such as nemaline and myotubular myopathy, anterior horn cell disorders including spinal muscular atrophy (SMA), and metabolic myopathies. For each, it discusses genetics, clinical presentation, management considerations, and includes illustrative images. The goal is to help clinicians identify impending respiratory failure and monitor patients using tests like pulmonary function tests.