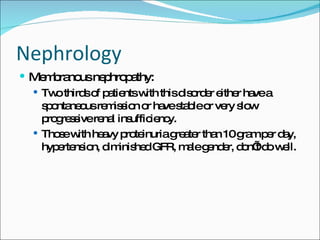
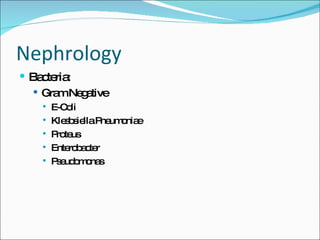
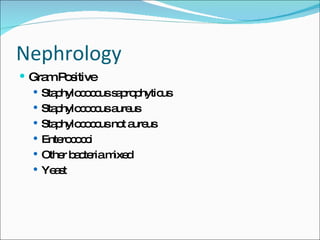
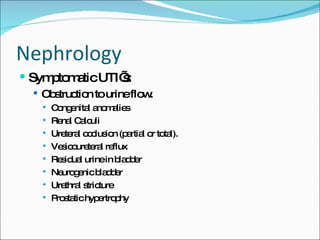
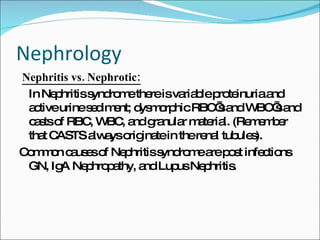
This document provides an overview of urine analysis techniques and findings related to nephrology. It discusses urine dipstick testing and issues that can affect results. It also describes urine casts, crystals, and cells that may be seen during microscopic urine examination and what different findings indicate in terms of kidney conditions and diseases. Common bacteria that cause urinary tract infections are listed. Radiologic techniques used to evaluate the kidneys are briefly outlined.