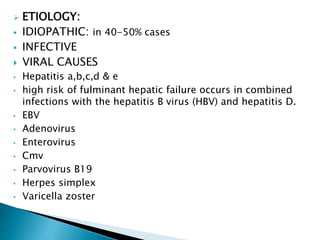
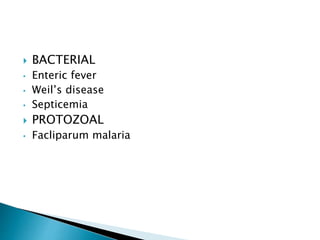
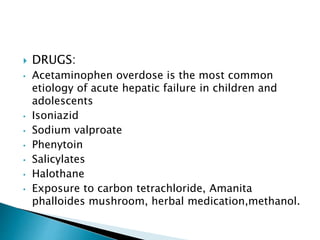
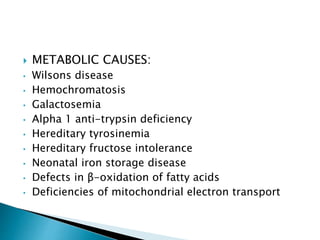
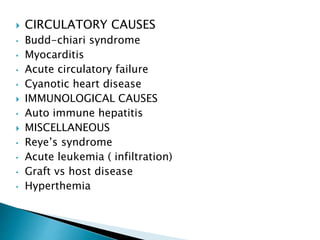
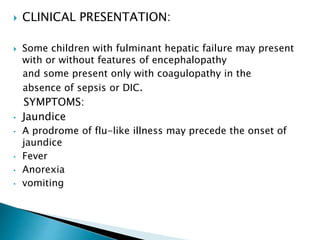
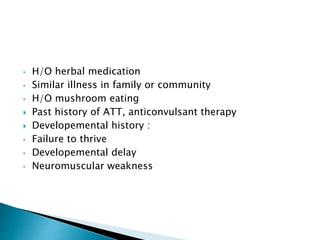
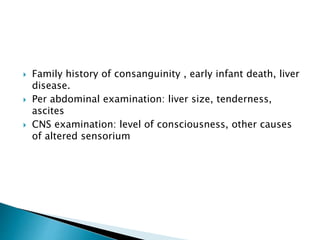
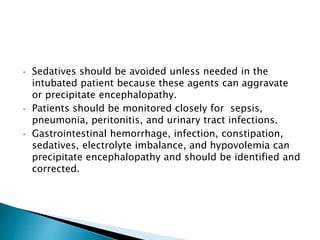
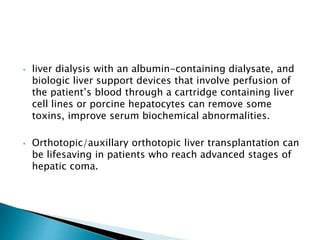
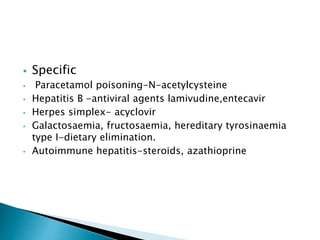
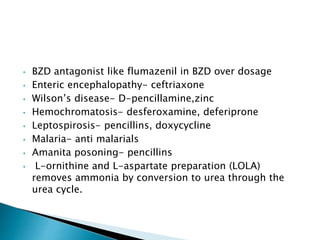
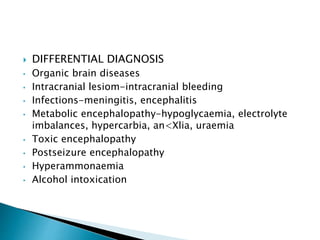
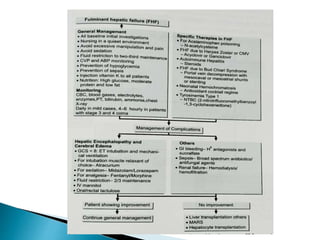
Fulminant hepatic failure is a clinical syndrome resulting from massive liver cell necrosis or impairment. It is characterized by coagulopathy and encephalopathy that develops over less than 8 weeks. The liver loses its synthetic, excretory, and detoxifying functions. Causes include viral hepatitis, drugs like acetaminophen, and metabolic disorders. Presentation includes jaundice, fever, vomiting, and confusion. Treatment focuses on supportive care, treating complications, and sometimes liver transplantation. Prognosis depends on factors like age, etiology, and development of complications.