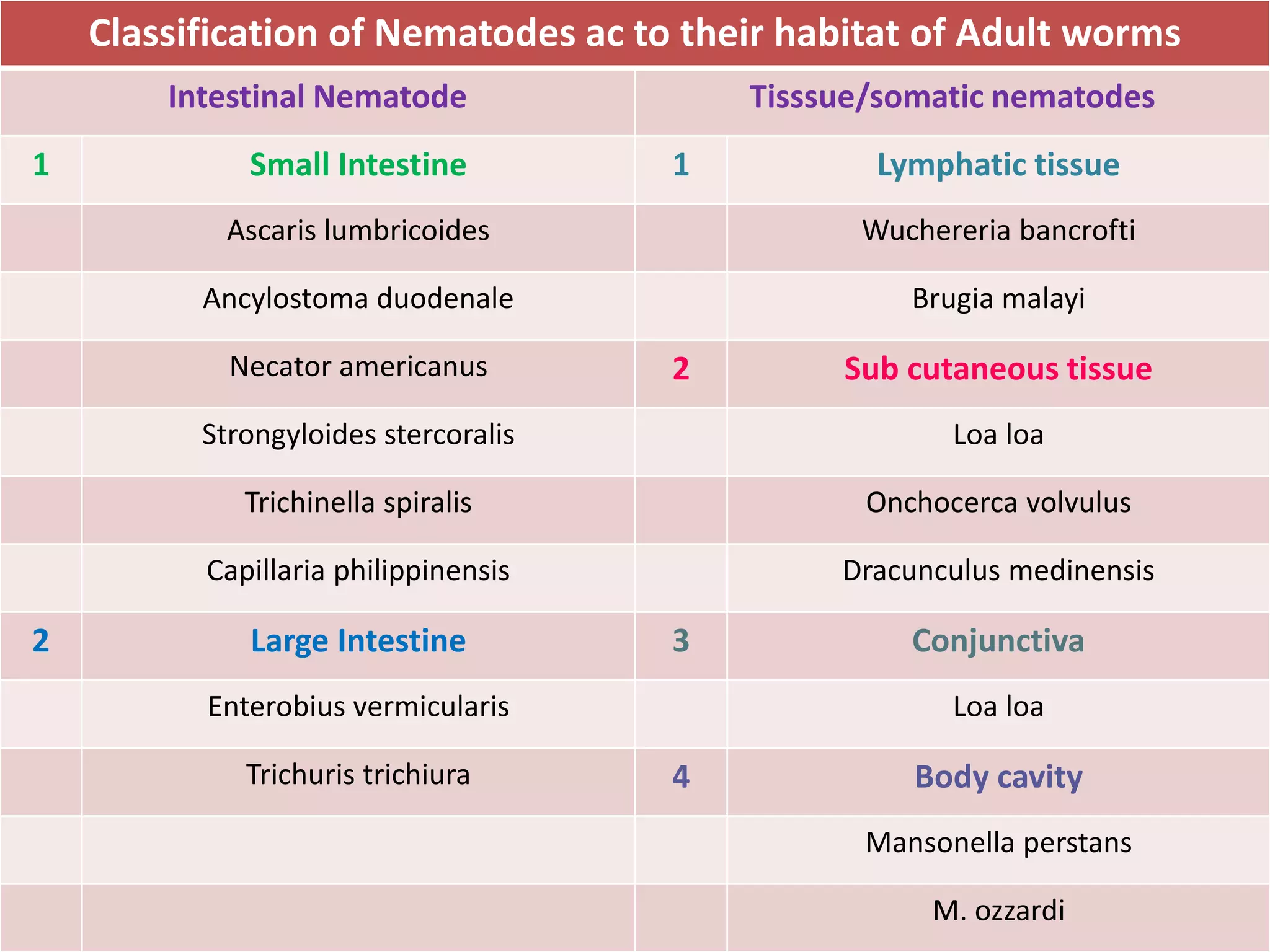
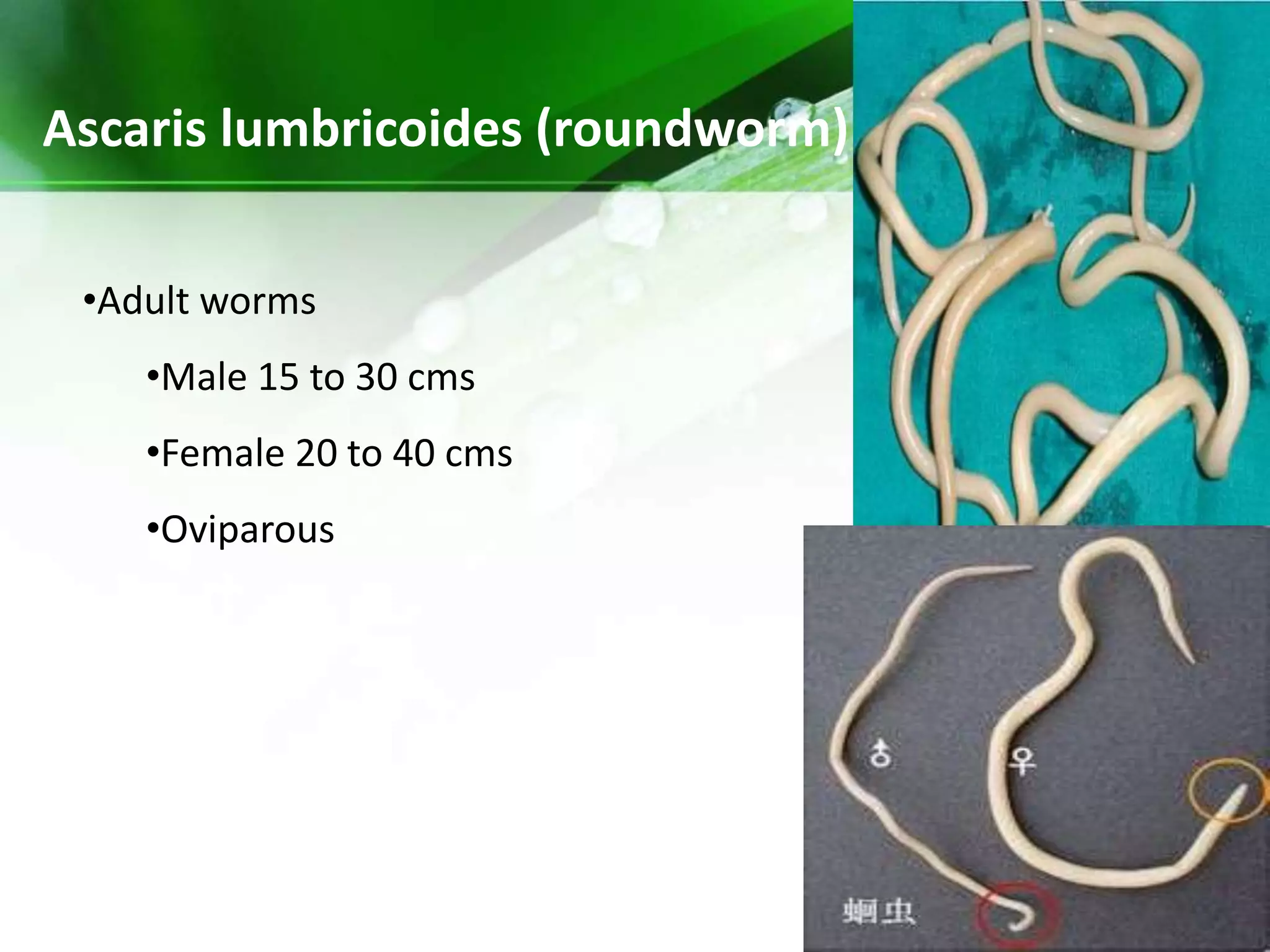
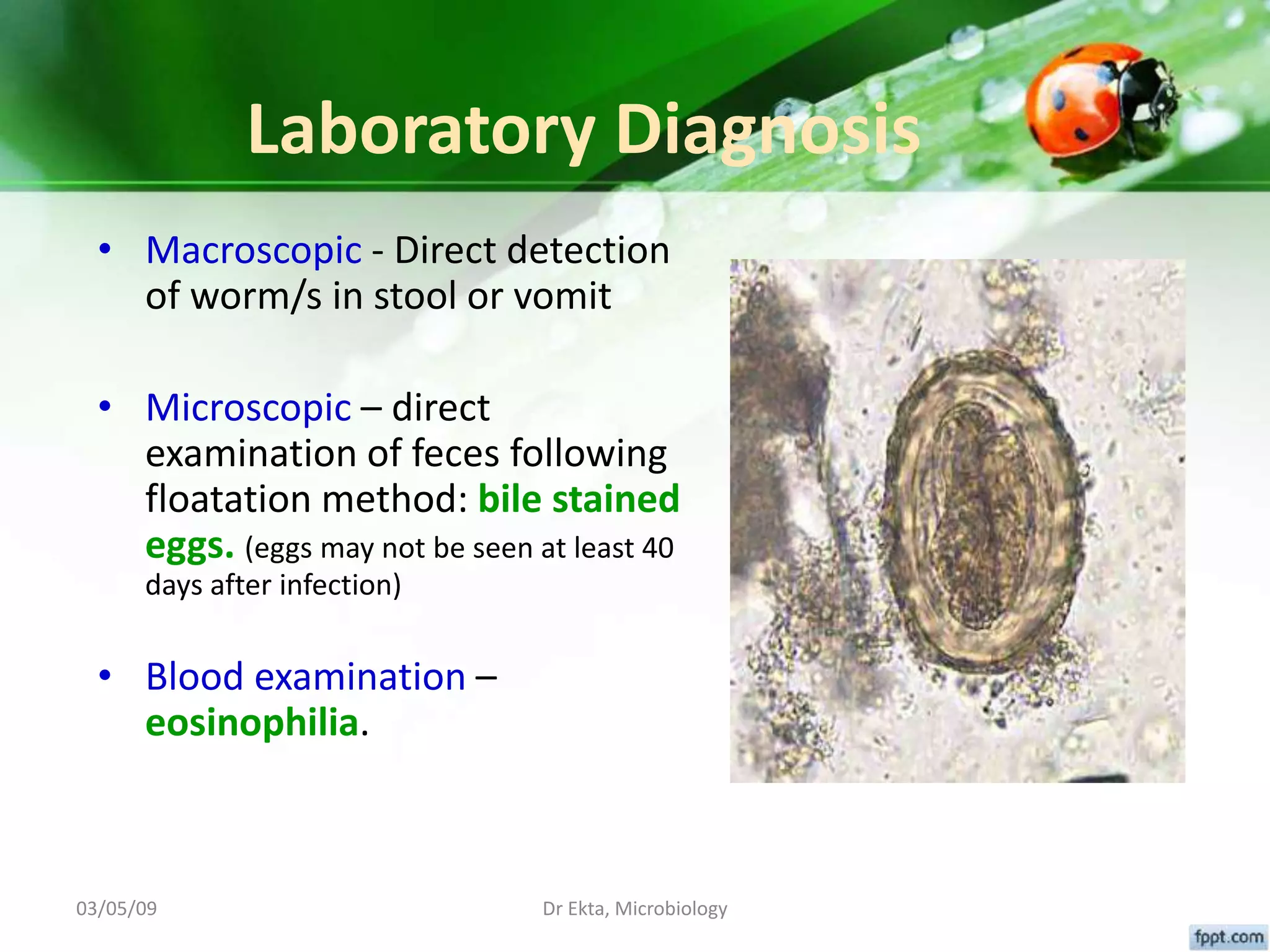
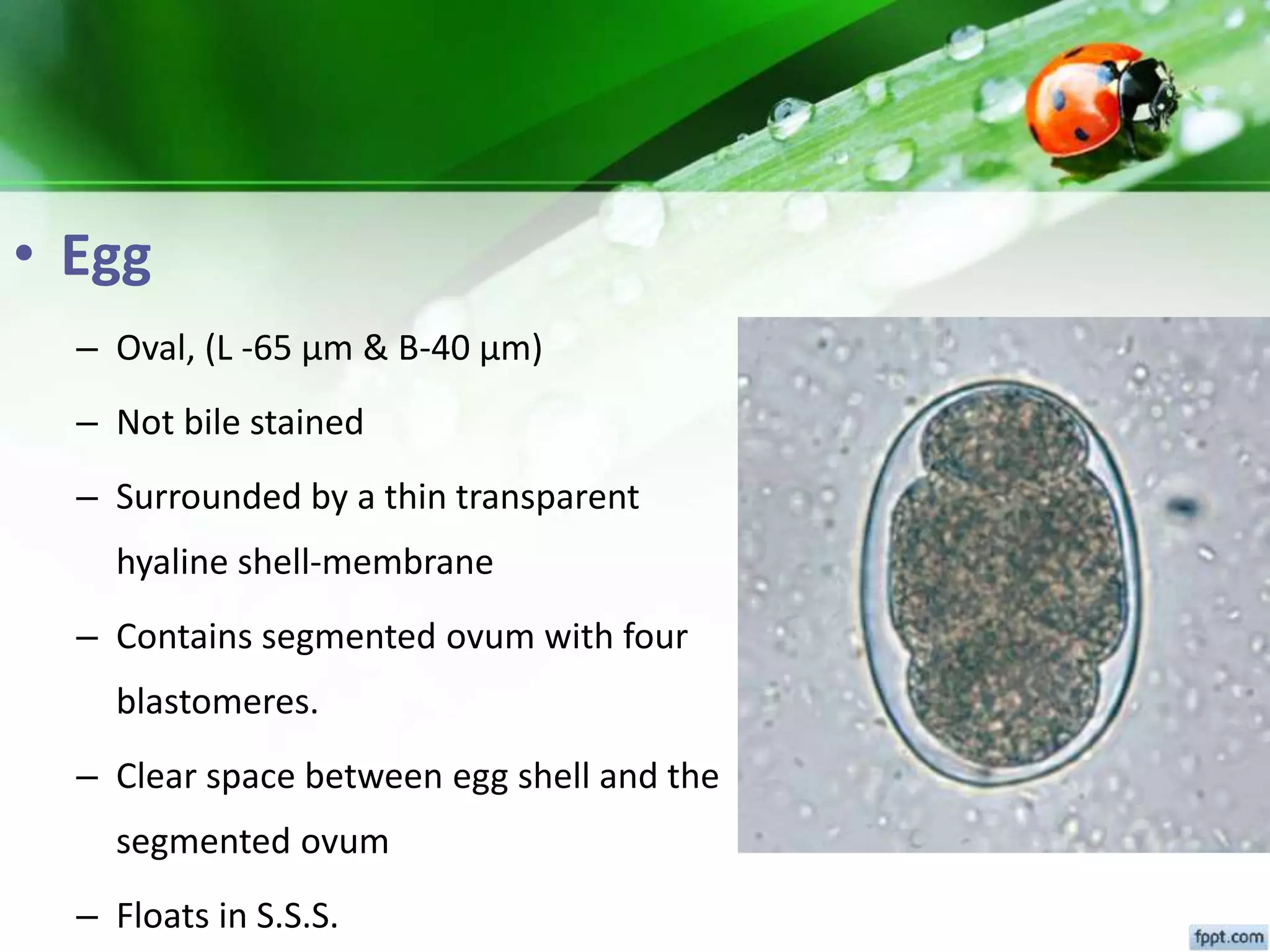
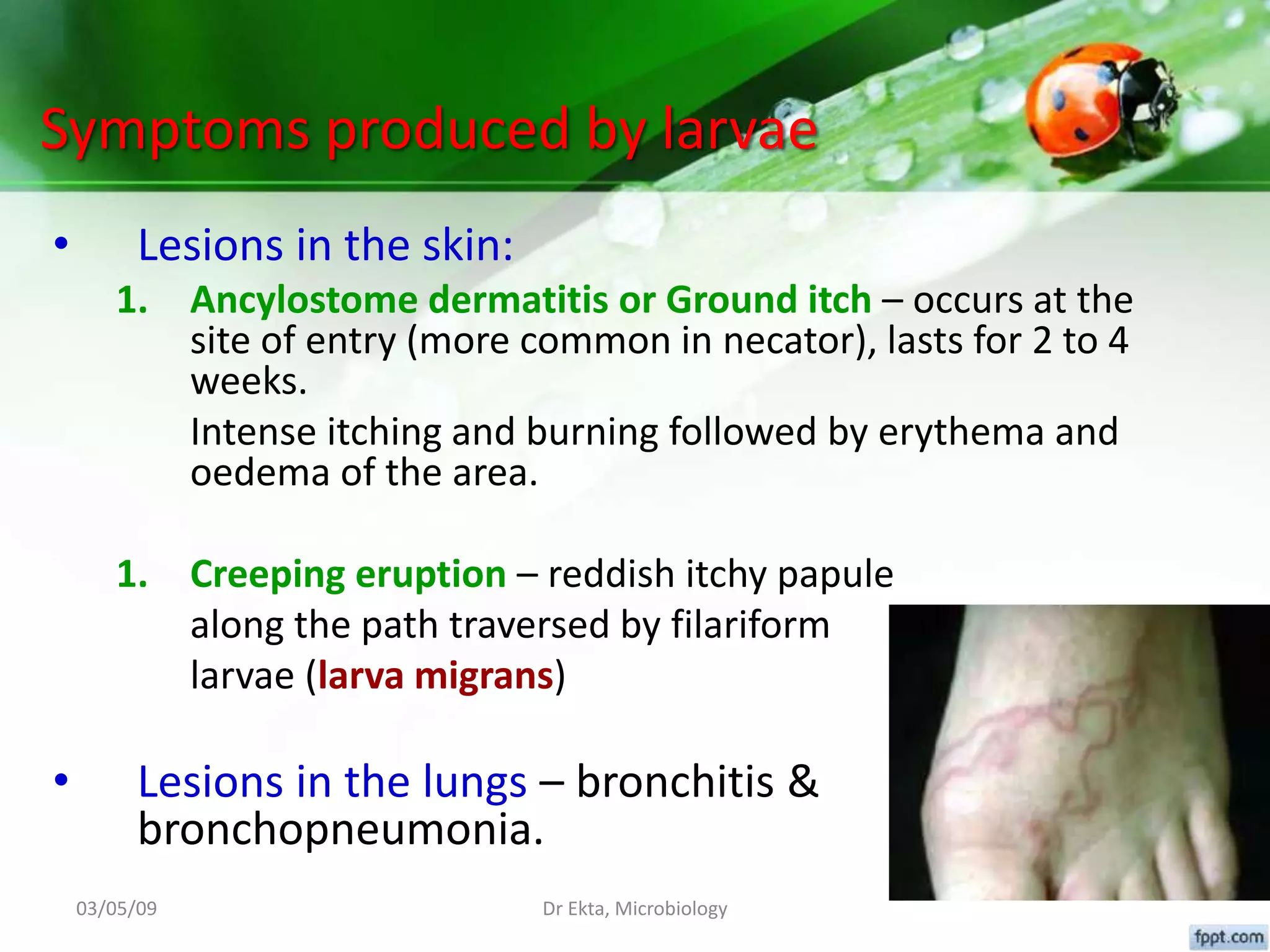
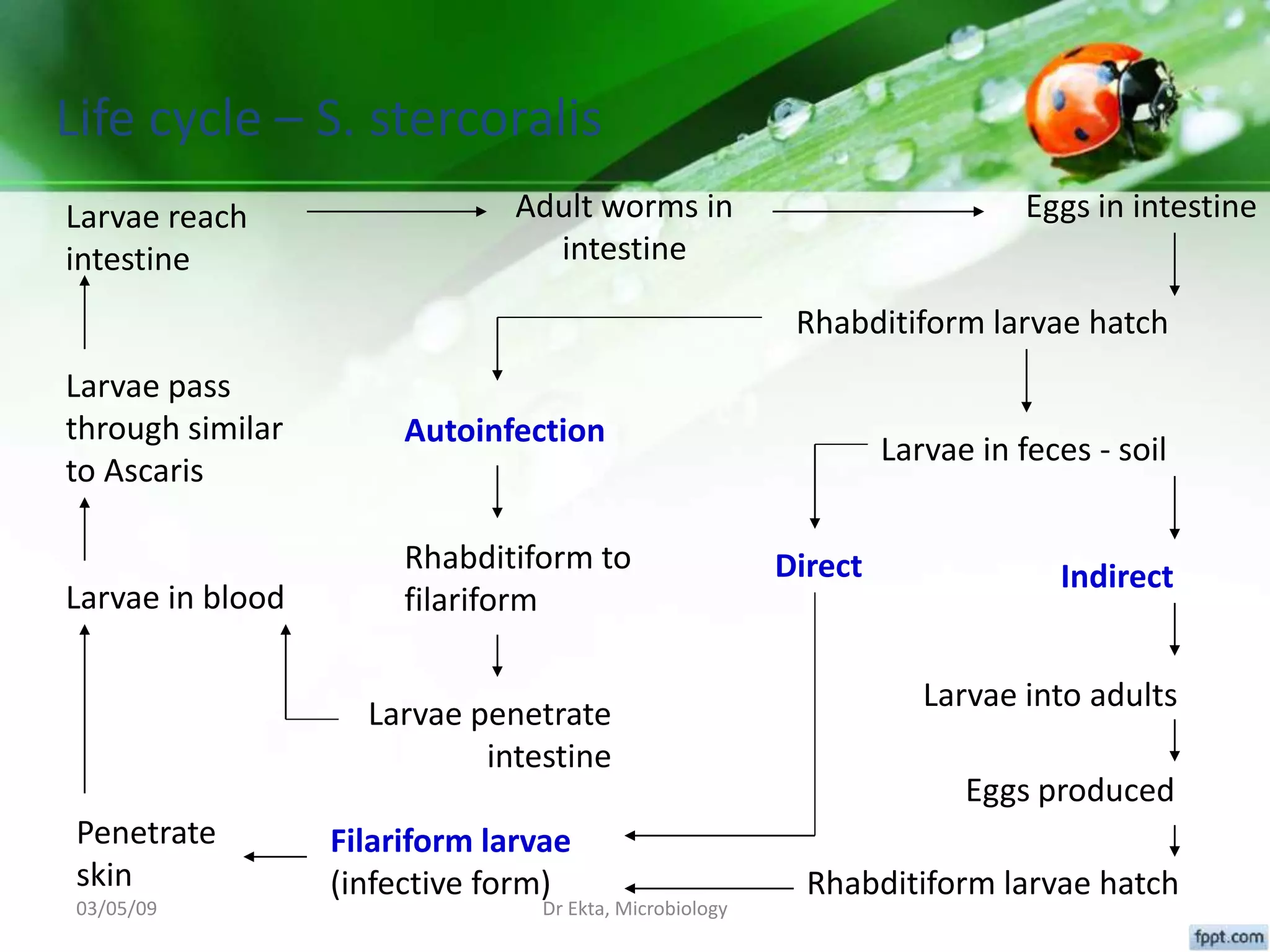
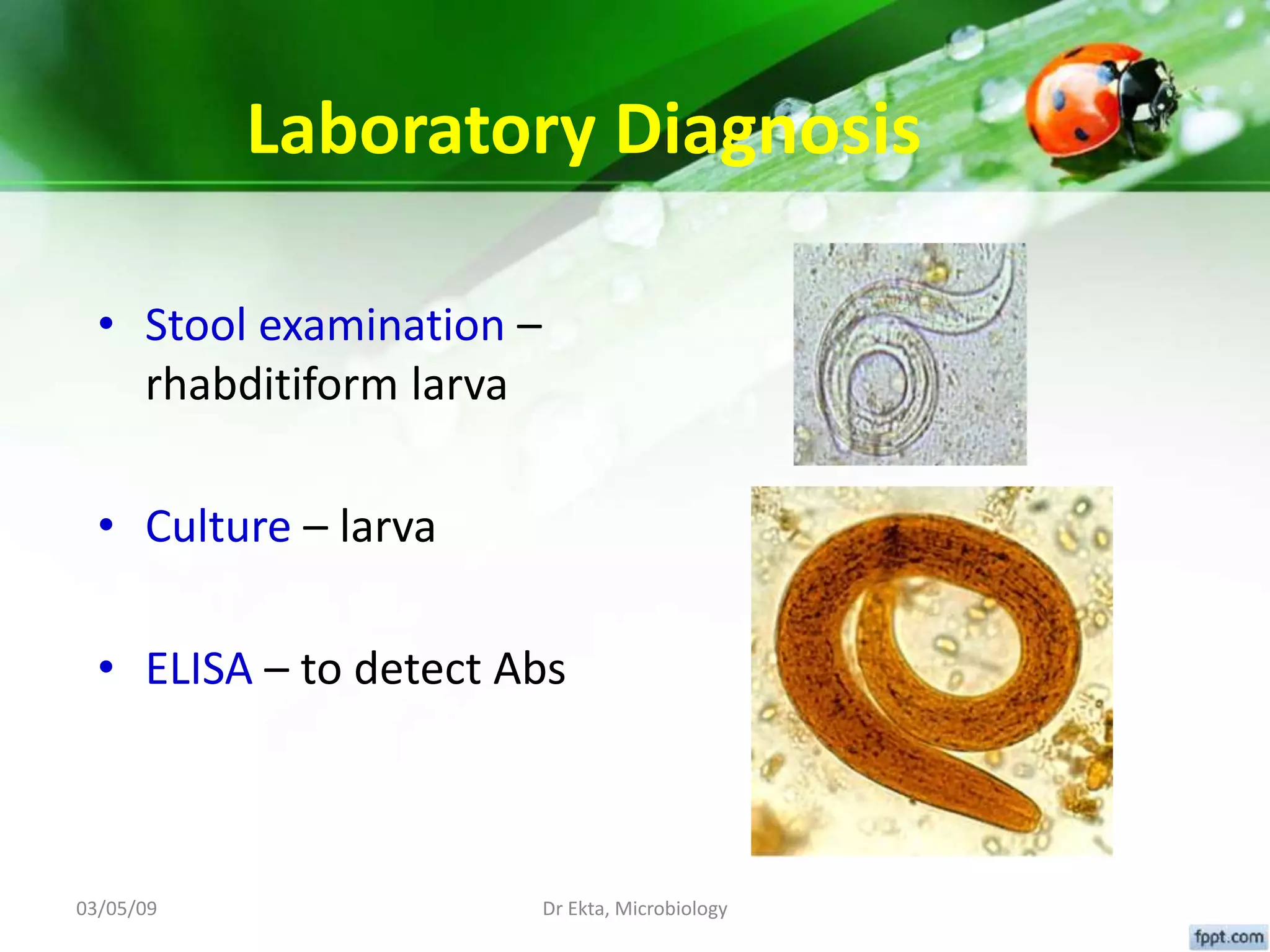
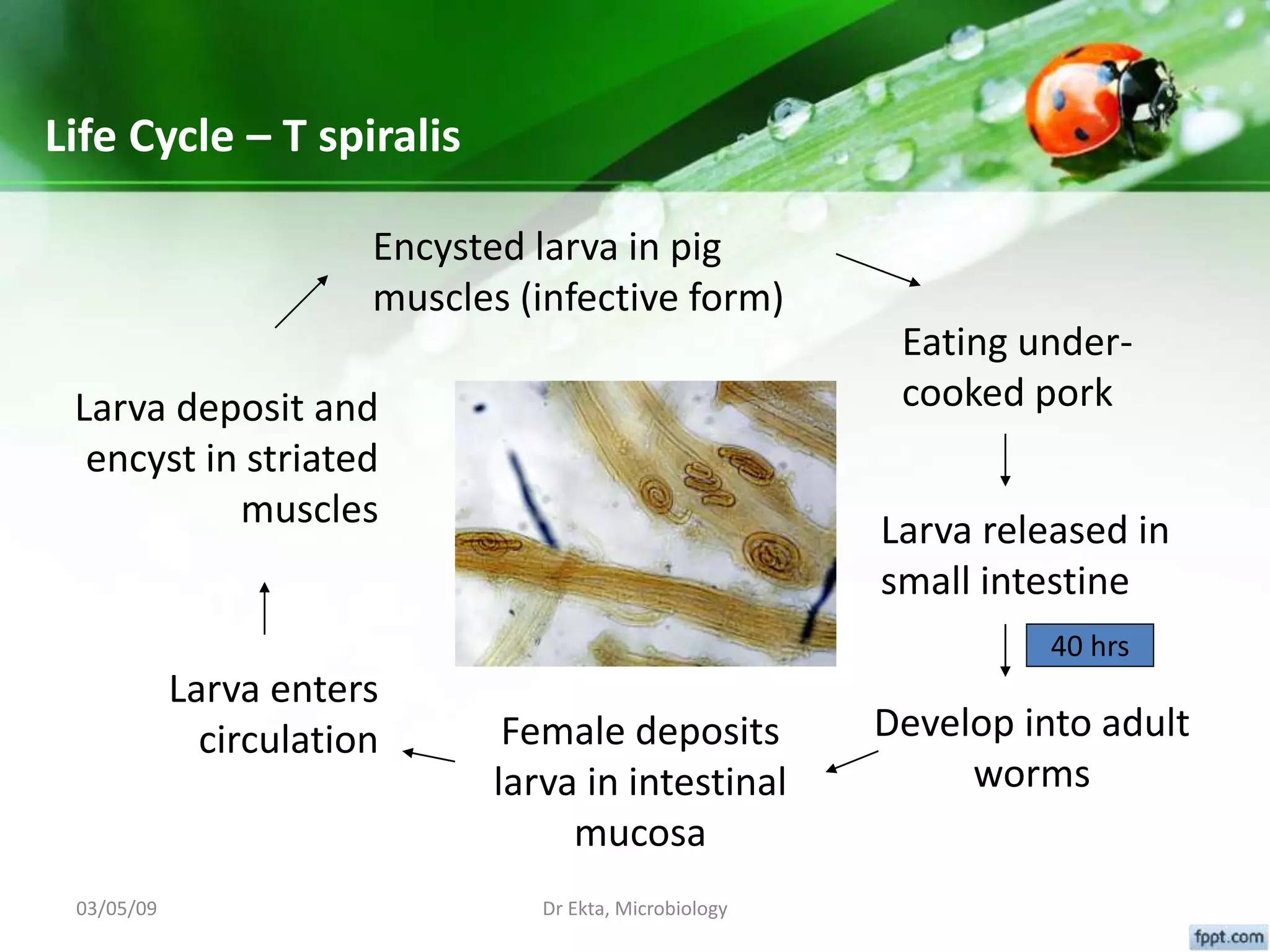
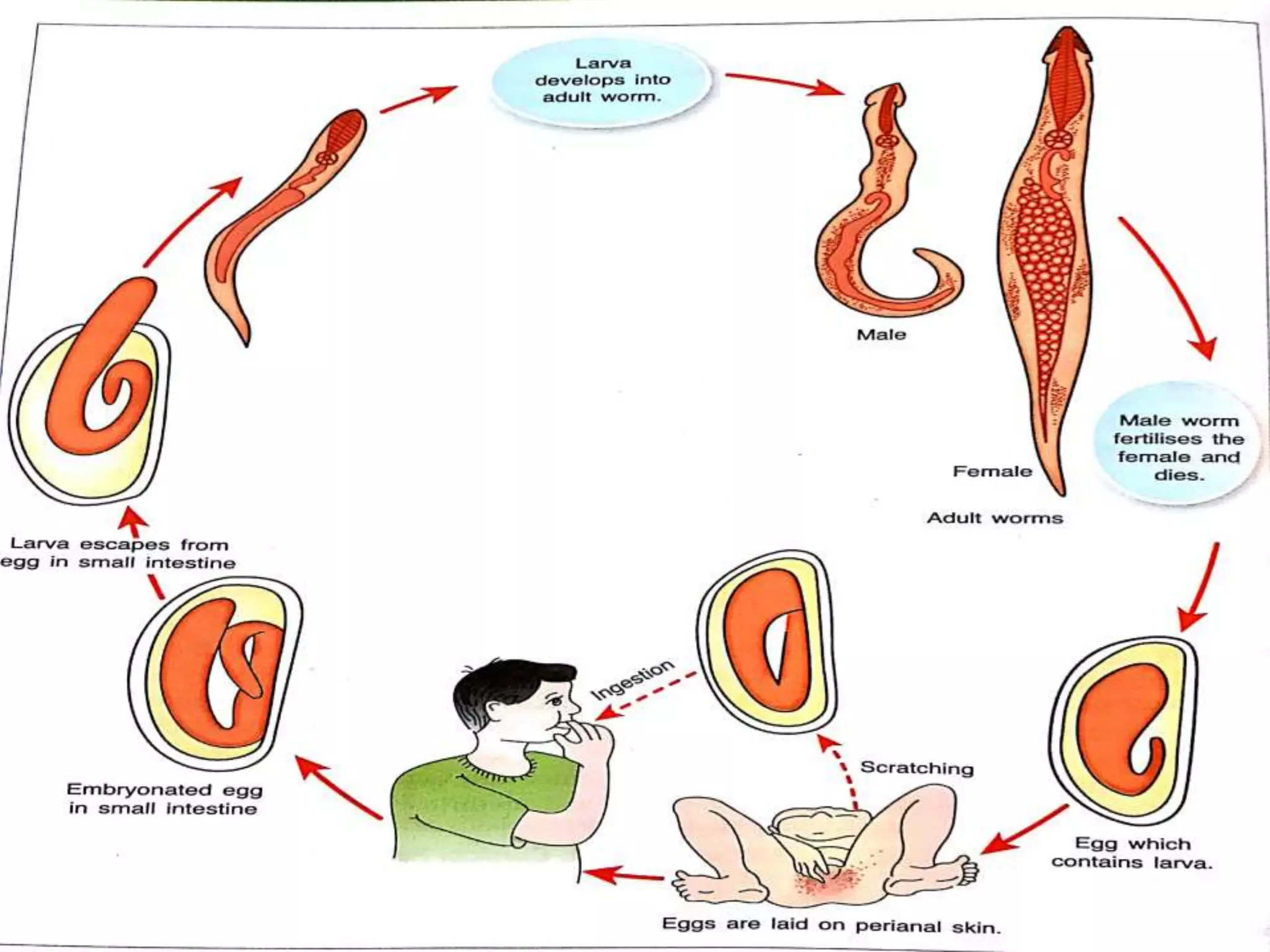
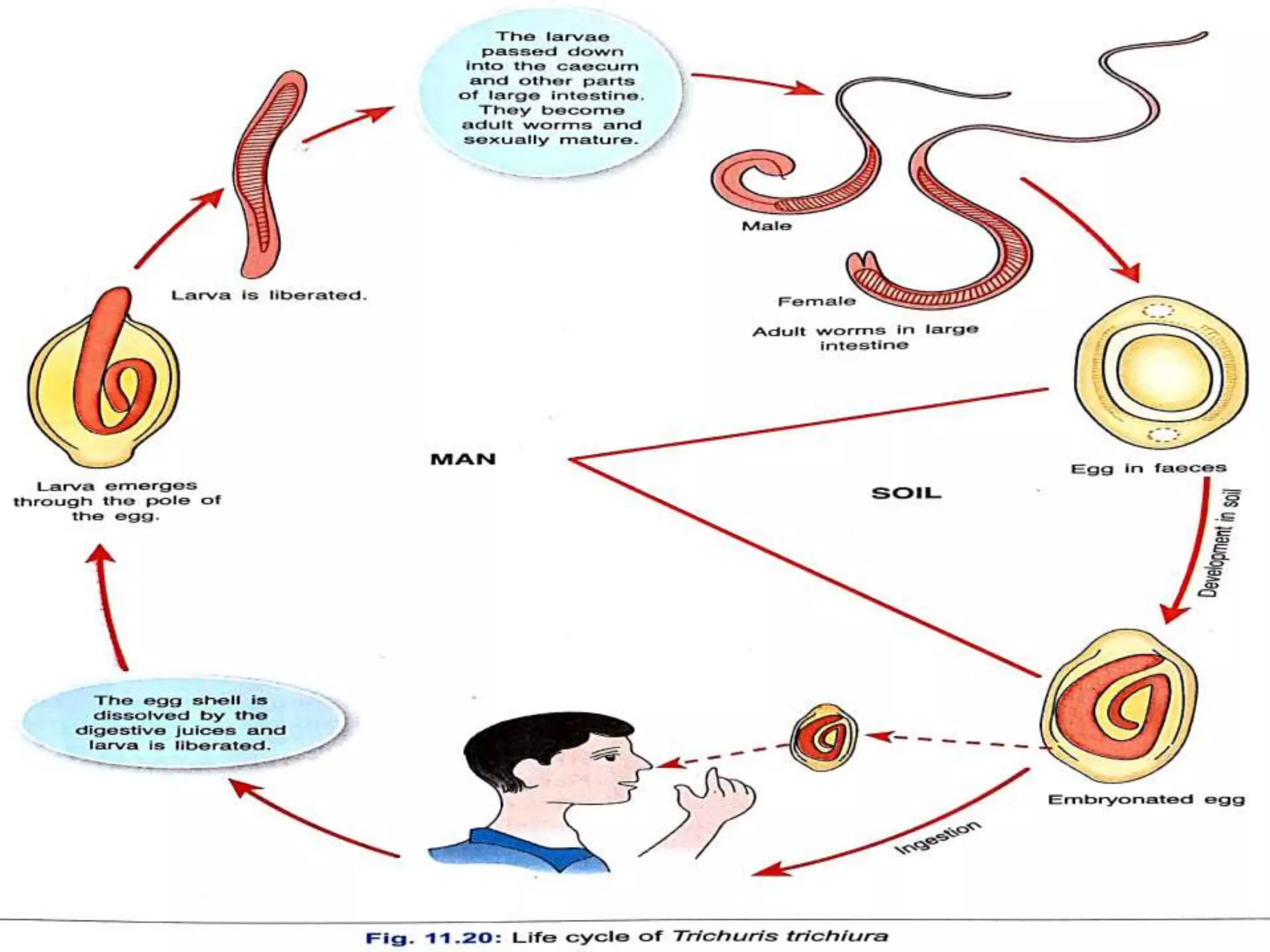
This document provides information on nematodes (roundworms). It discusses key characteristics of nematodes such as their elongated shape and presence of a cuticle. It also describes the classification and life cycles of several medically important nematodes that infect humans, including Ascaris lumbricoides (roundworm), Ancylostoma duodenale (hookworm), Strongyloides stercoralis, Trichinella spiralis (trichina worm), Enterobius vermicularis (pinworm), and Trichuris trichiura (whipworm). For each nematode, it covers features such as the adult worm morphology, eggs, life cycle, pathogenicity, clinical signs, and methods for laboratory