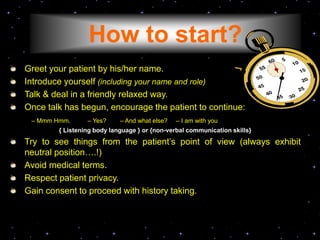
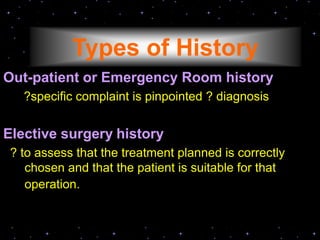
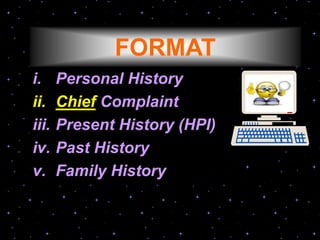
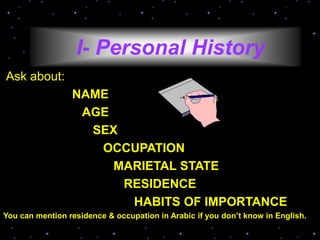
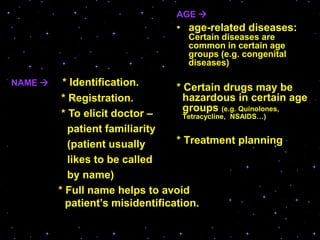
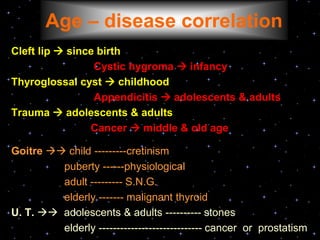
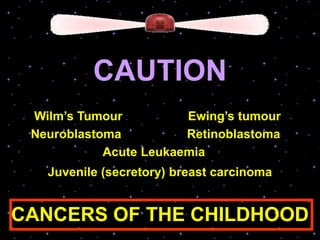
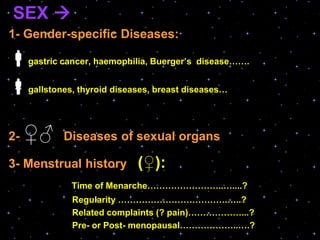
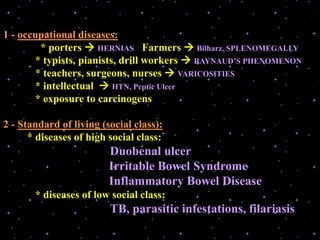
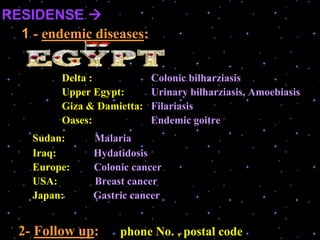
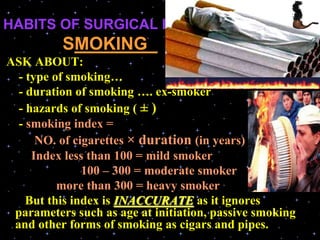
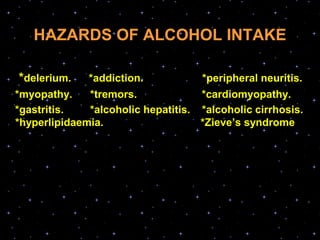
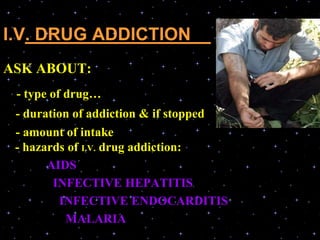
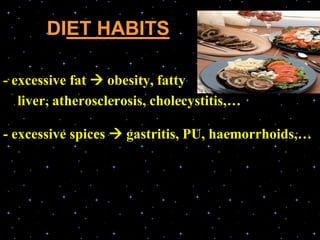
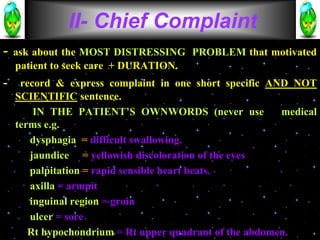
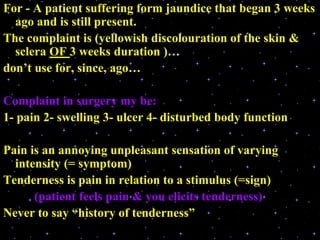
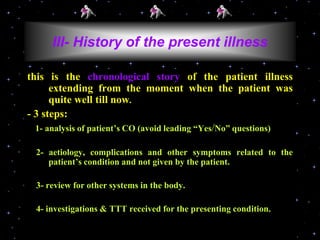
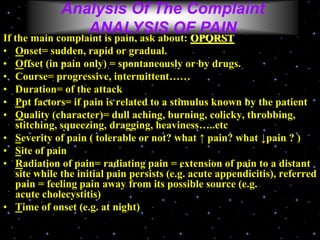
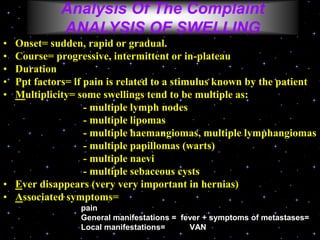
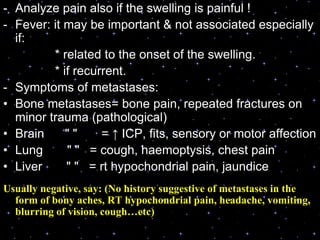
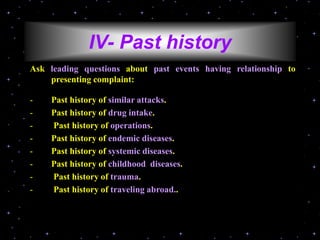
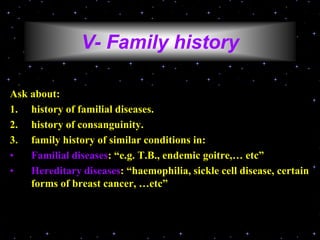
This document provides guidance on taking a thorough surgical history. It emphasizes that history taking is important for accurate diagnosis, communication, documentation, and individualizing patient care. The key components of a surgical history include gathering personal information, chief complaint, present history, past history, family history, and reviewing habits. When analyzing the chief complaint, details about pain, swelling, or other symptoms should be explored thoroughly.