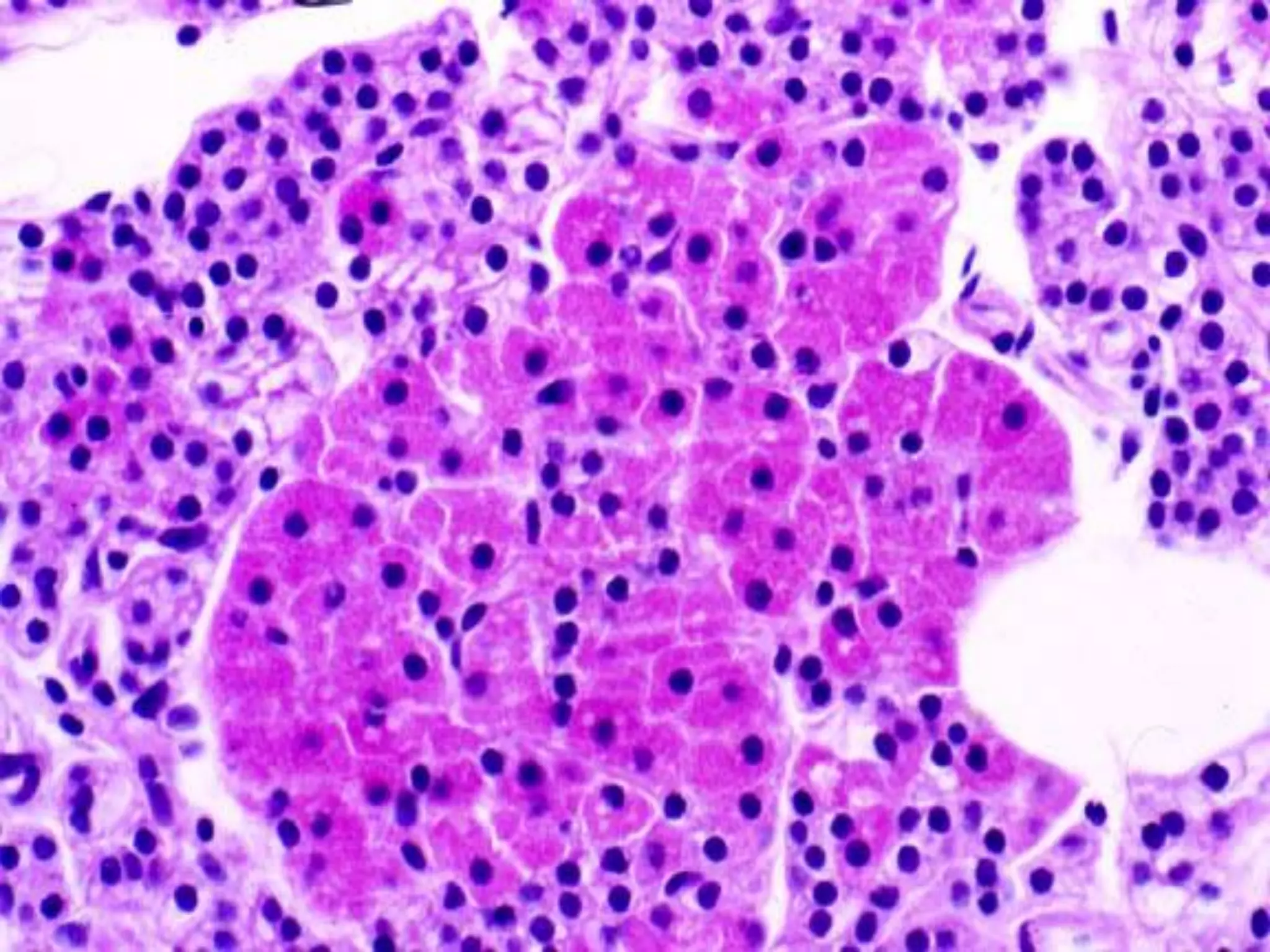
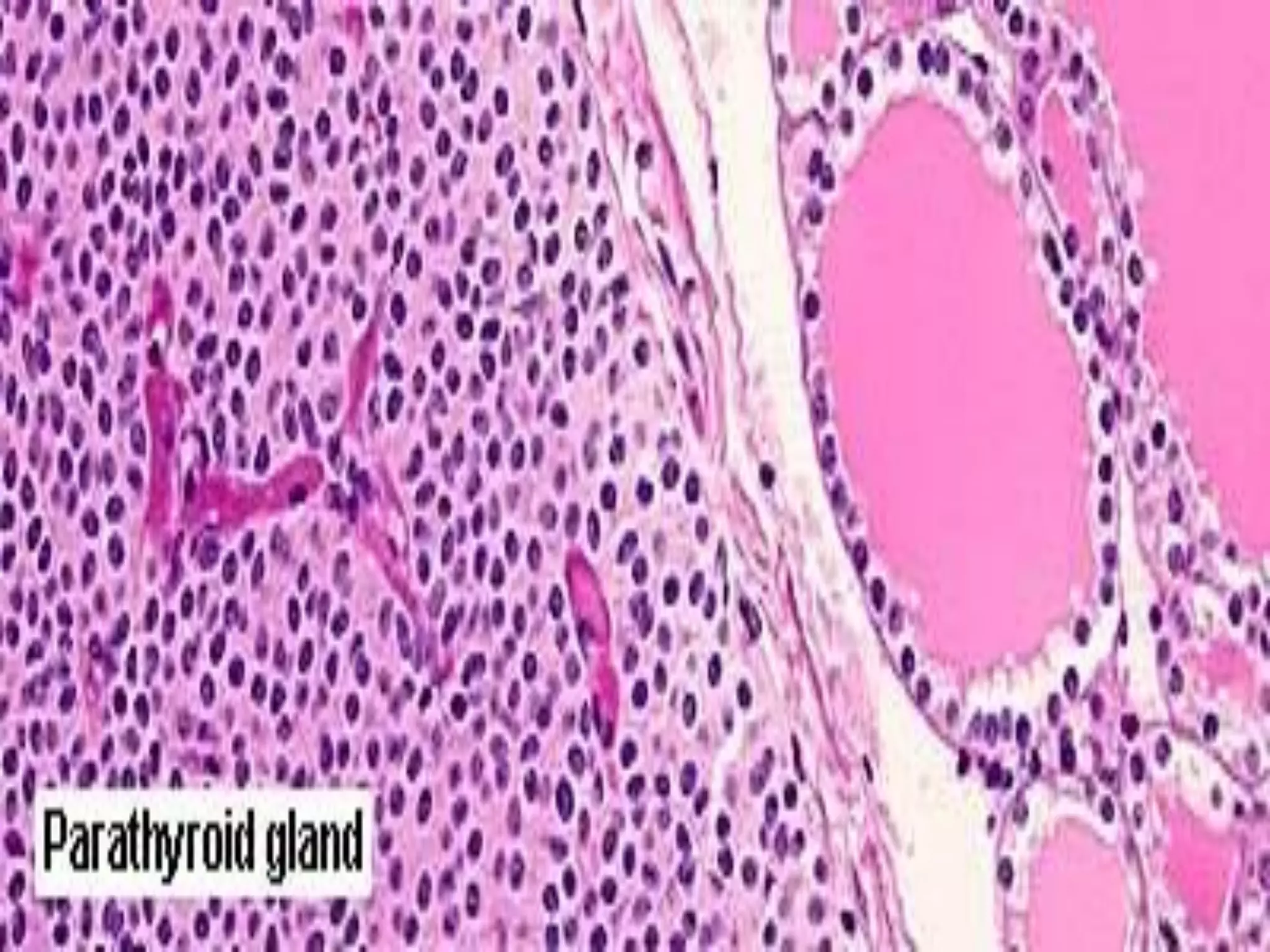
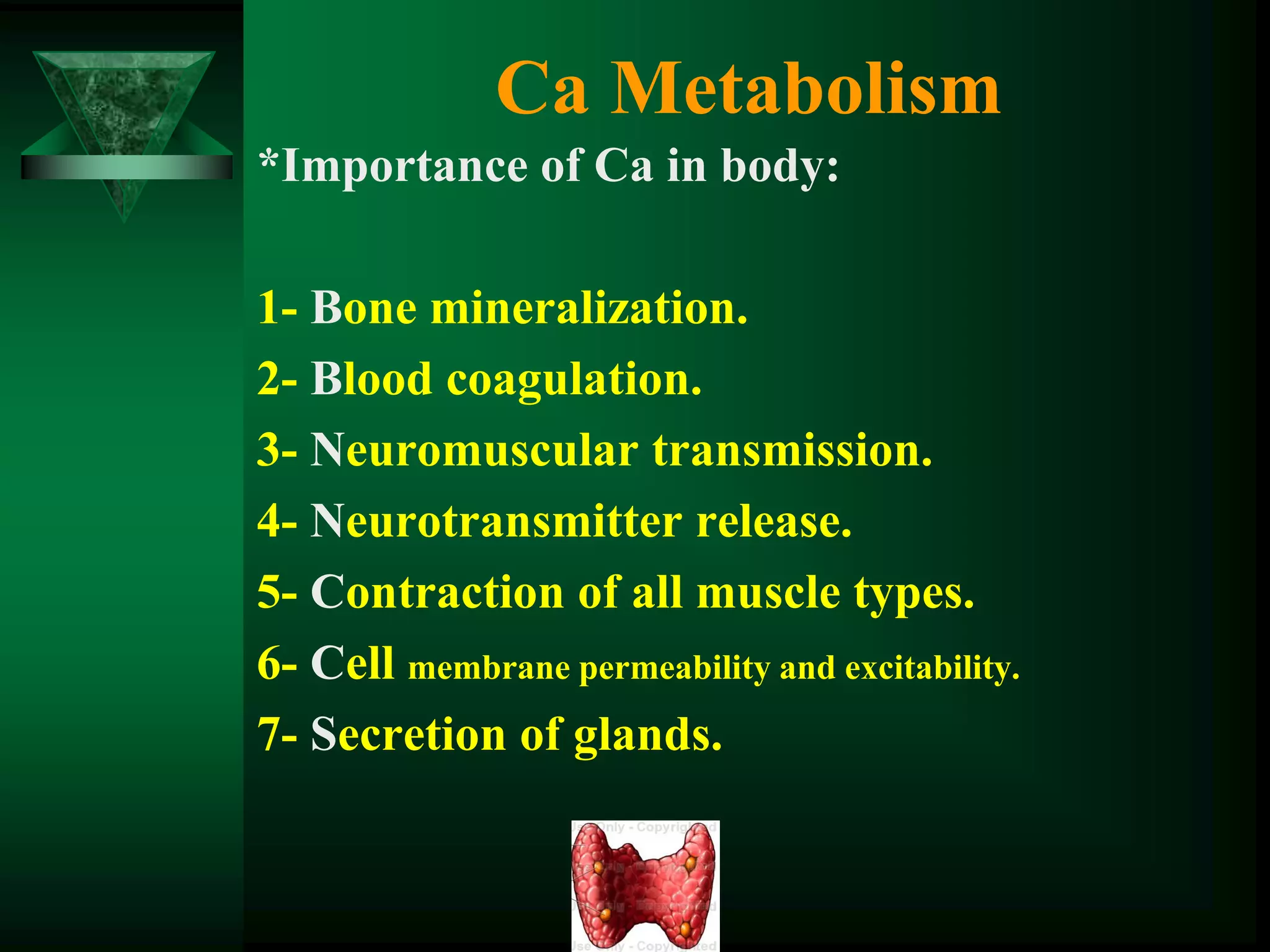
Hyperparathyroidism is caused by overproduction of parathyroid hormone (PTH) resulting in abnormal calcium homeostasis. Primary hyperparathyroidism is caused by uncontrolled PTH production from a parathyroid adenoma in 85% of cases. Symptoms include bone and kidney problems, abdominal pain, weakness and mood changes. It is diagnosed based on high PTH and calcium levels. Treatment involves surgical removal of the affected parathyroid gland(s). Secondary and tertiary hyperparathyroidism are caused by prolonged hypocalcemia from kidney disease or malnutrition, and are treated medically or with parathyroidectomy if medications fail.