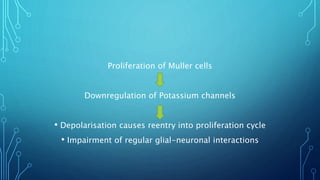
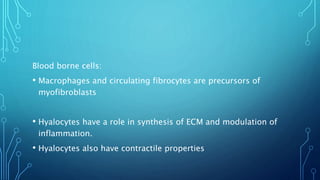
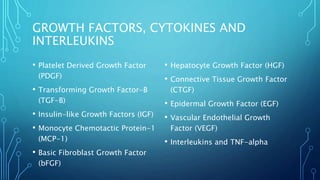
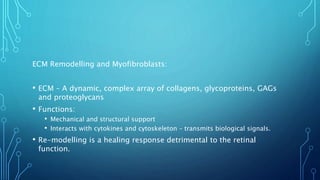
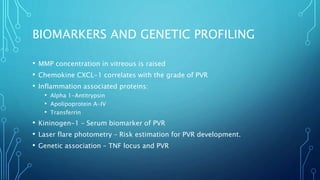
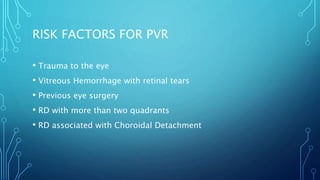
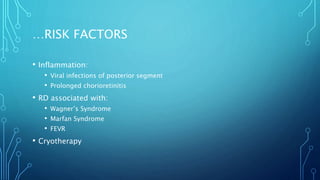
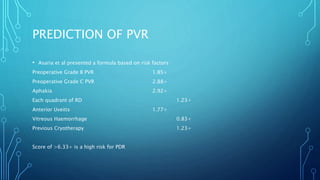
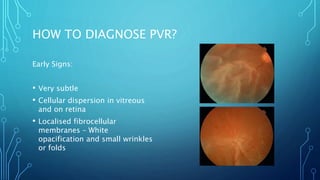
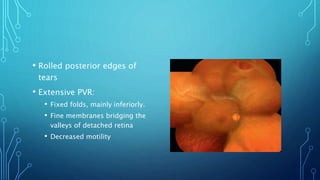
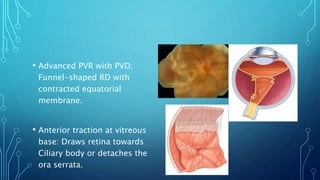
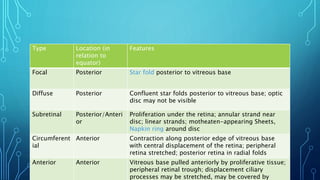
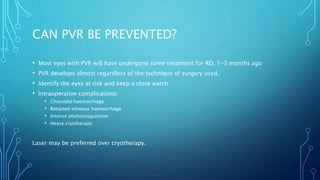
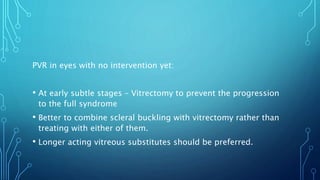
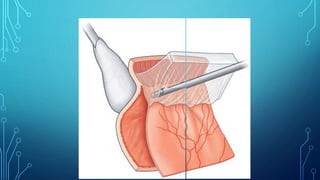
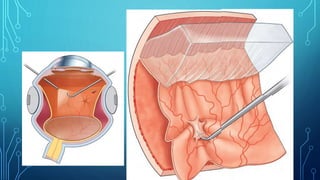
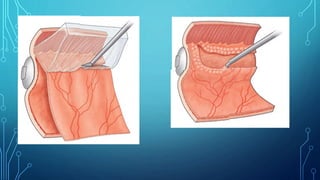
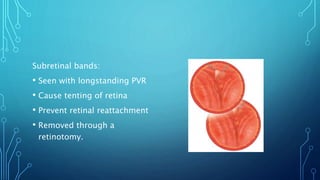
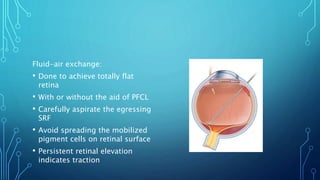
This document provides an overview of proliferative vitreoretinopathy (PVR). It defines PVR as a fibrotic wound healing response involving proliferation of cells that can cause retinal traction and detachment. The pathophysiology involves epithelial-mesenchymal transition of retinal pigment epithelium cells and proliferation of glial cells, which secrete extracellular matrix proteins. Growth factors and cytokines promote proliferation and contraction of fibrocellular membranes. Risk factors include retinal detachment, inflammation, and previous vitreoretinal surgery. Early diagnosis and timely surgery aiming to relieve traction and reattach the retina are important for treatment.