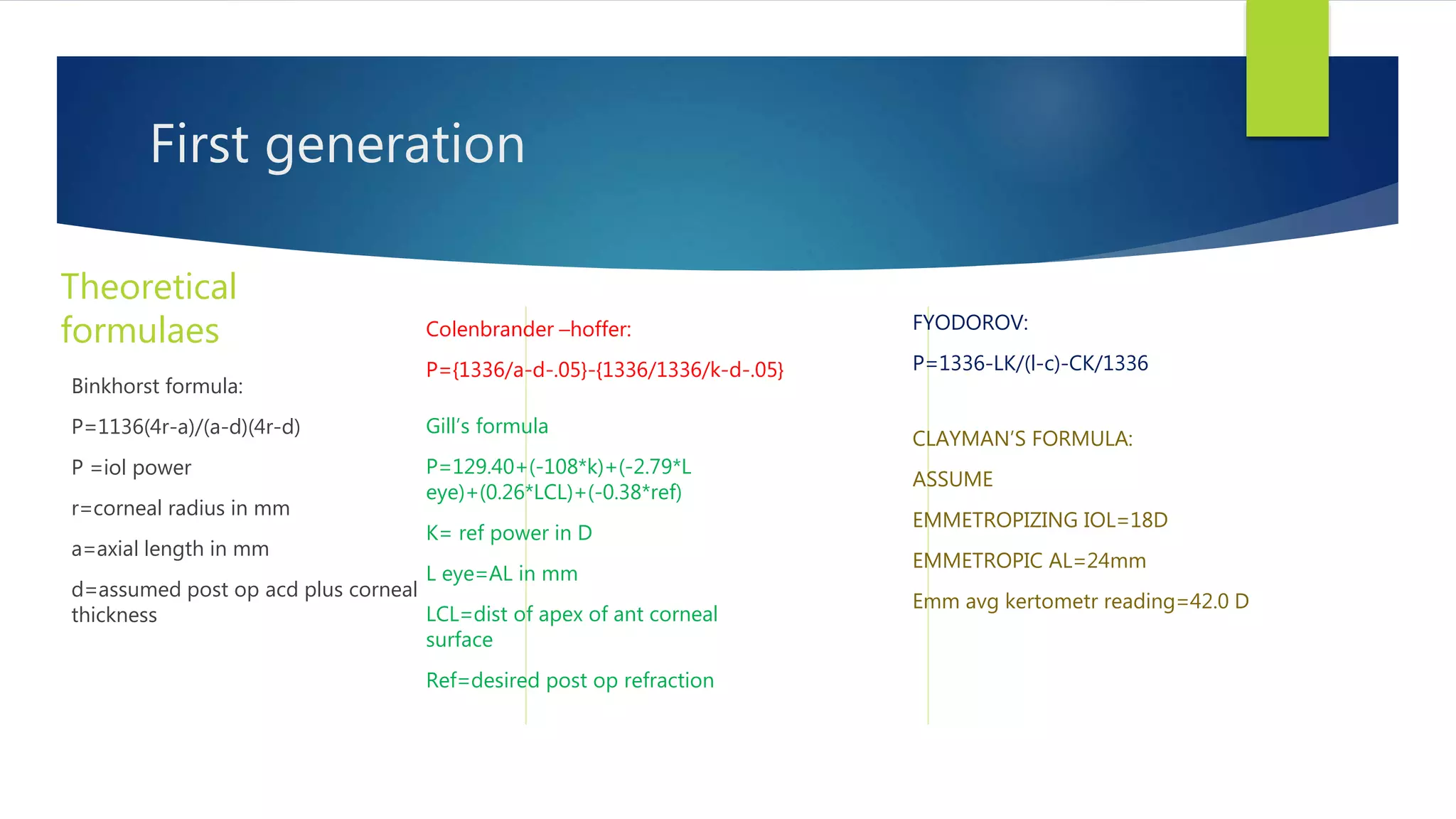
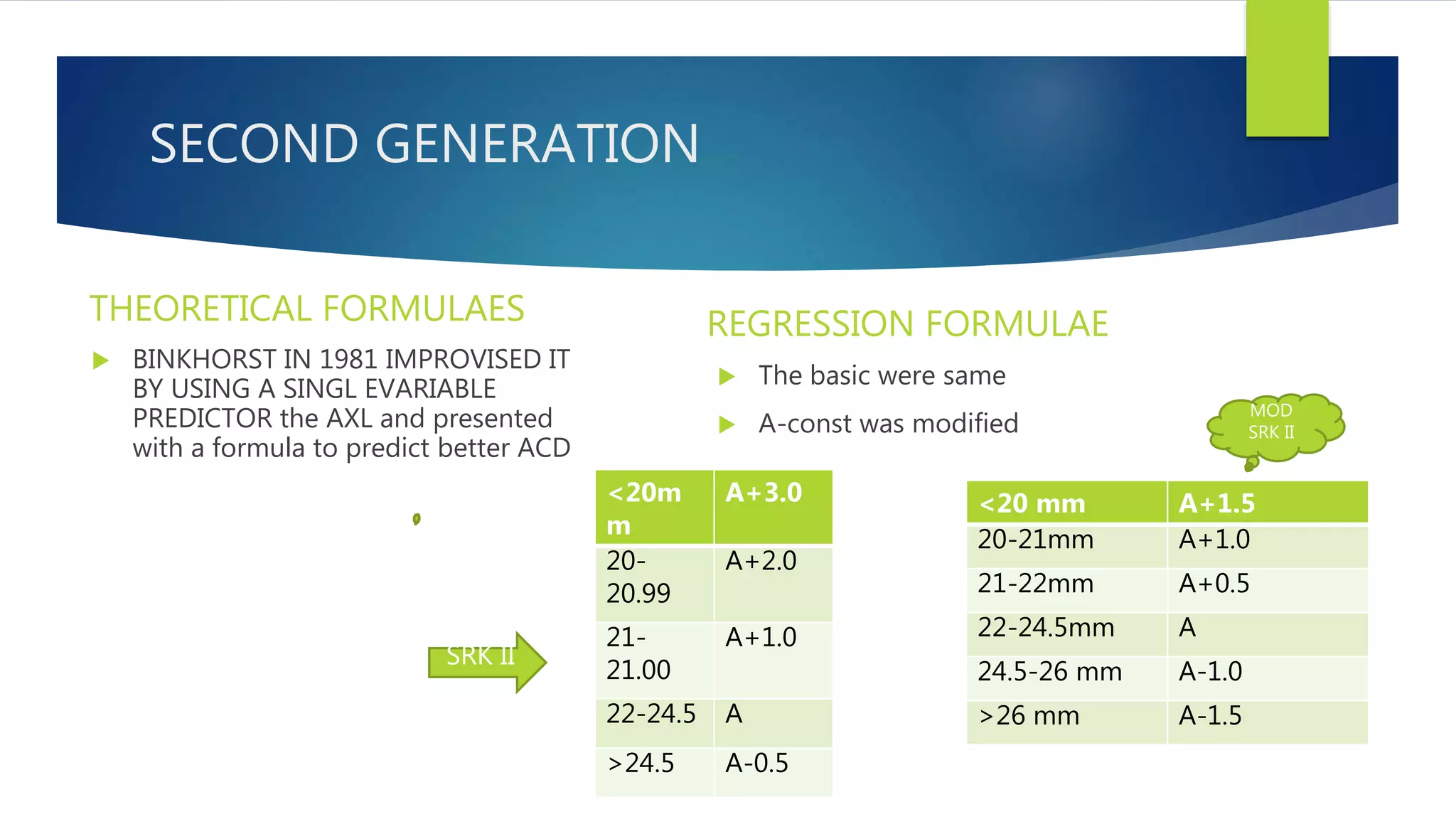
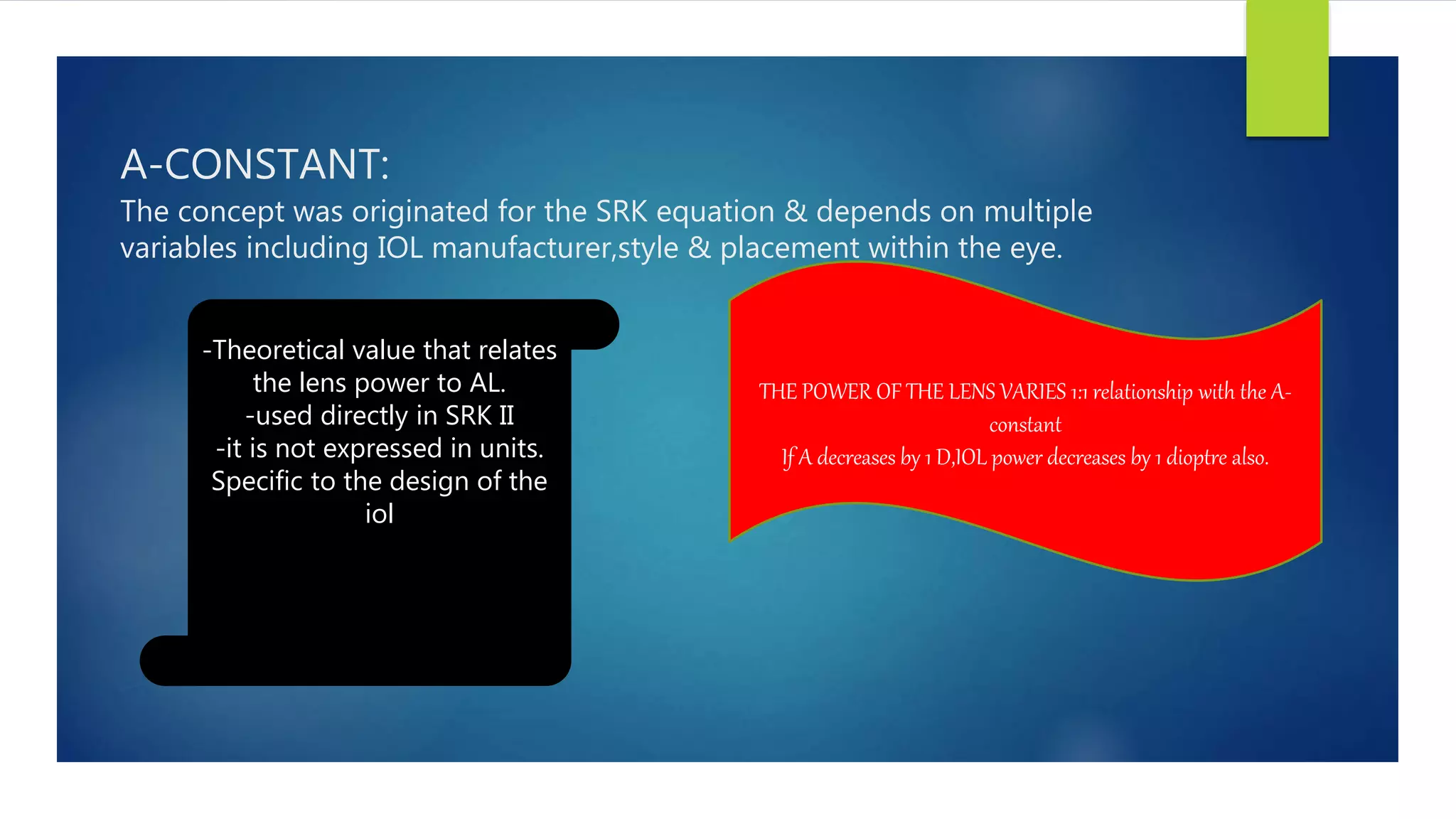
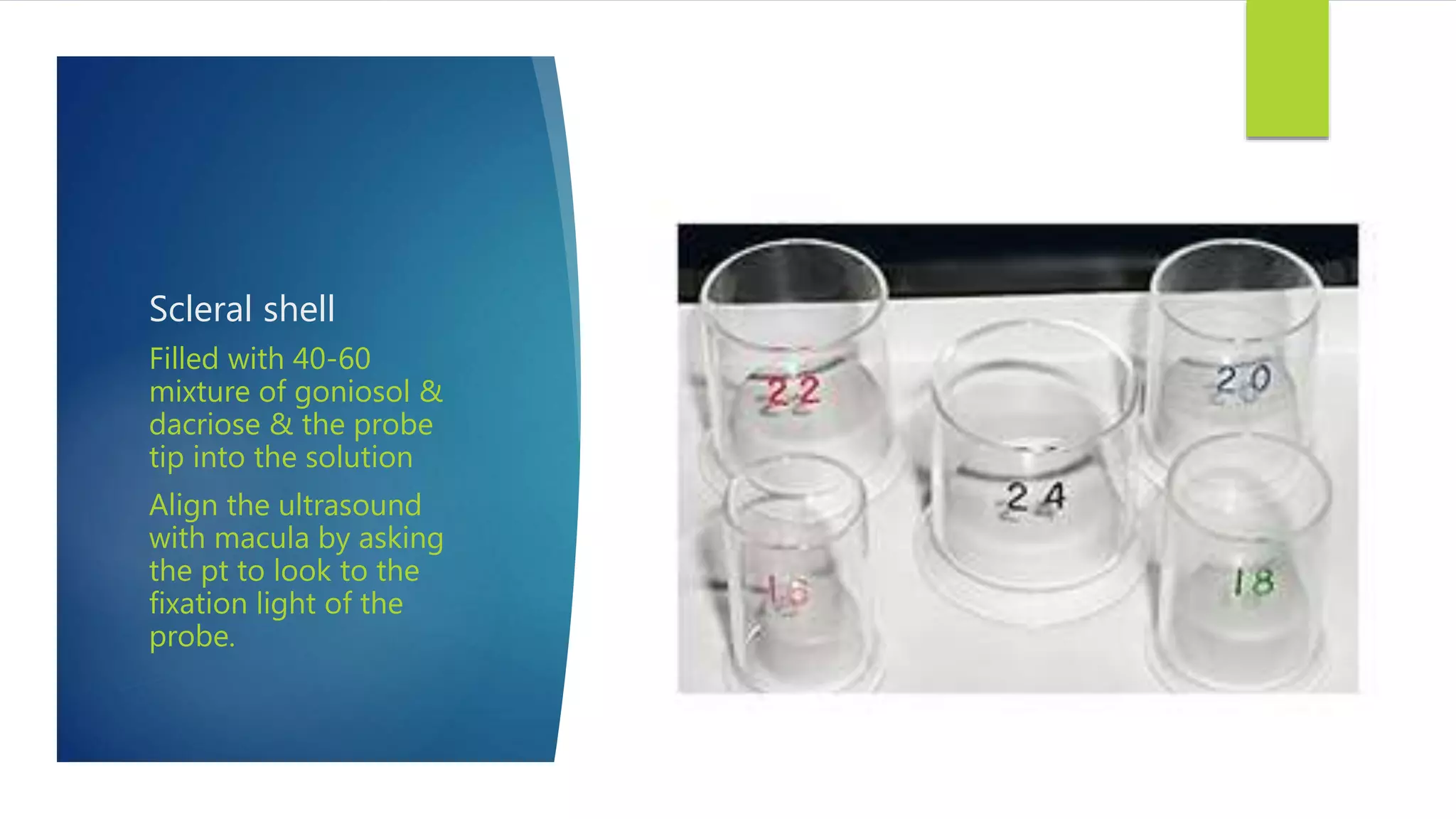
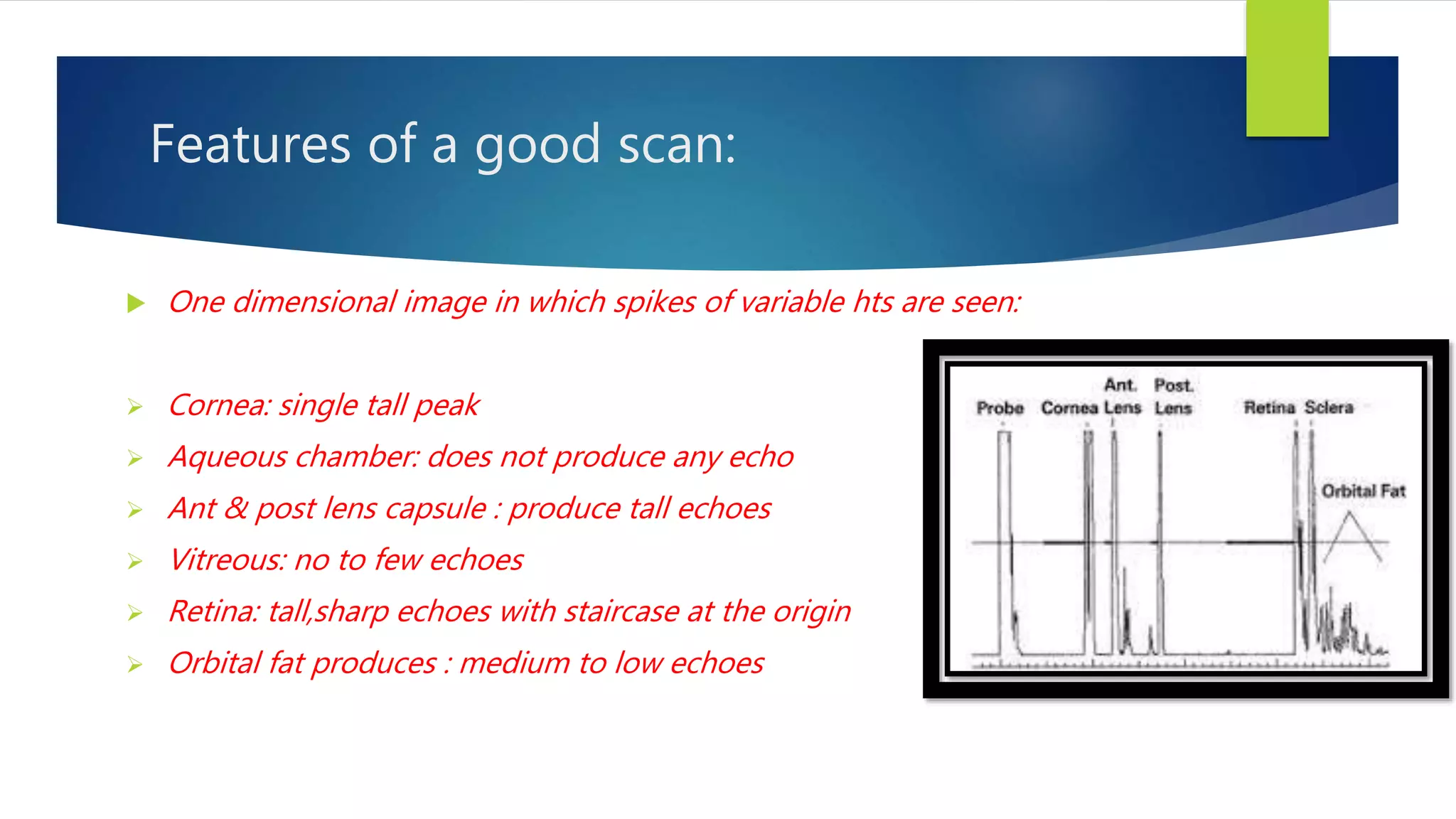
This document discusses biometry and intraocular lens (IOL) power calculation. It begins by defining biometry as the analysis of biological data using mathematical and statistical methods. It then describes various biometry techniques including A-scan ultrasound to measure axial length, keratometry to measure corneal curvature, and different formulas used to calculate IOL power. Over generations, the formulas have evolved from theoretical to regression-based approaches using parameters like axial length, keratometry readings, and A-constants specific to IOL designs. Proper technique and quality checks are important for accurate biometry and IOL power calculation to achieve the desired refractive outcome.












![History :
Helmholtz—javal & schiotz---Bausch & laumb{reichert}
{1854} {1881} {1932}
}}}]}}](https://image.slidesharecdn.com/biometry1-160913183150/75/Biometry-17-2048.jpg)