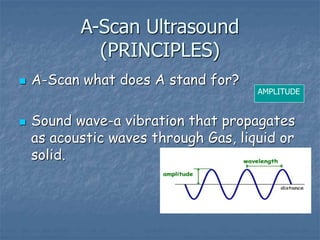
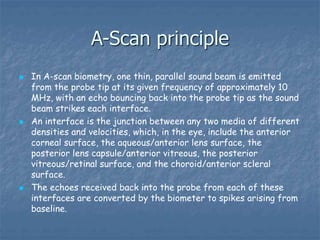
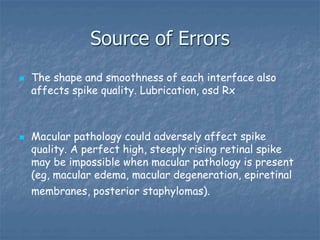
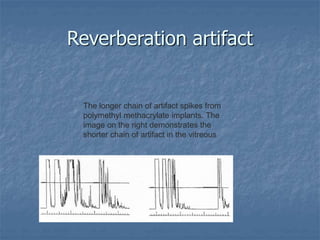
This document discusses ocular biometry, which is a clinical procedure used to measure intraocular distances and parameters for intraocular lens (IOL) power calculation and other purposes. It describes the principles of A-scan ultrasound biometry, including how sound waves are used to measure distances between ocular interfaces. Sources of error in biometry are discussed, as well as techniques to minimize errors. Important steps in performing a quality biometry exam are outlined. Finally, commonly used IOL calculation formulas are introduced.


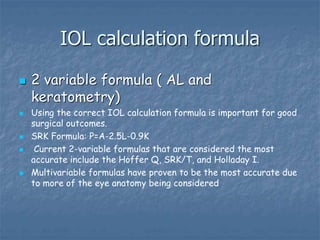
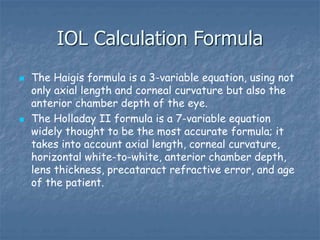
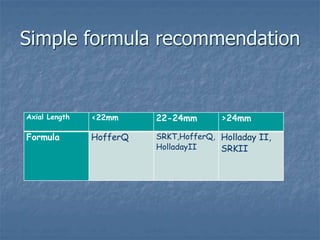
![IOL Calculation Formula
Predicting lens position is one of the most common
causes of a postoperative surprise; by taking more of
the eye anatomy into account, this can be more
accurately predicted. For average-length eyes with
average Ks, these formulas give almost identical
calculations. [3] However, when the eye is small,
formula selection is more critical. In eyes that are
less than 22 mm in length, the Hoffer Q and the
Holladay II IOL Consultant formulas are the most
accurate. For long eyes, the SRK/T and the Holladay
II IOL Consultant formulas are the most accurate.](https://image.slidesharecdn.com/biometryyonas-221104210107-198d4895/85/Biometry-Yonas-res-ppt-49-320.jpg)