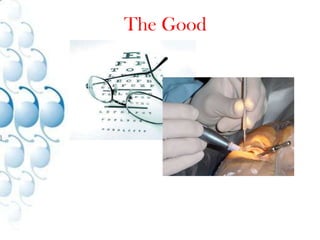
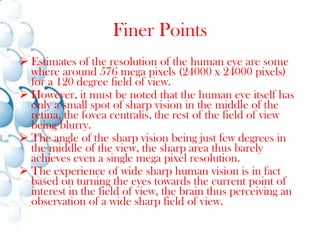
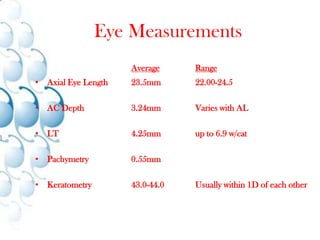
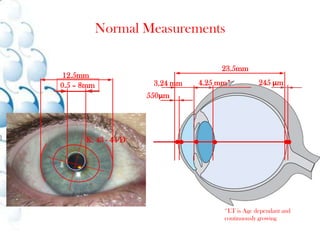
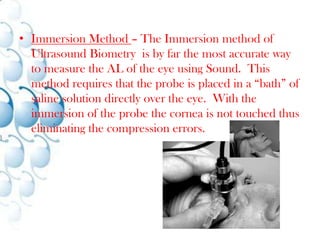
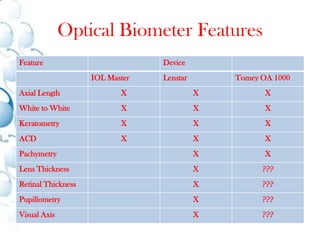
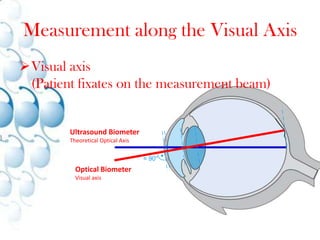
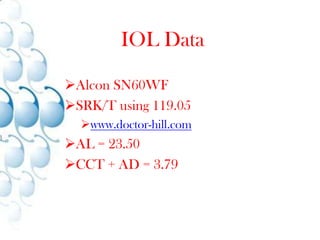
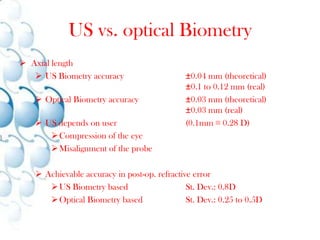
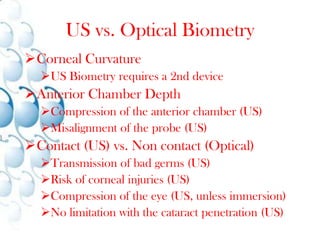
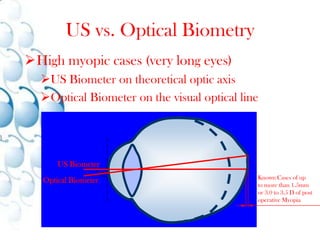
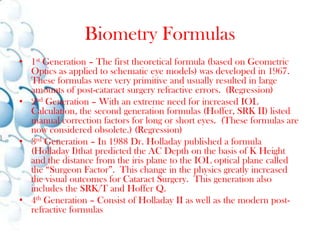
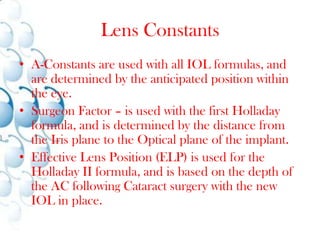
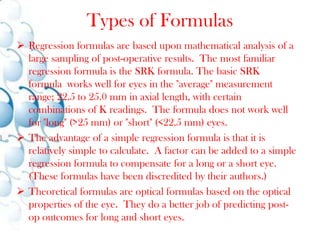
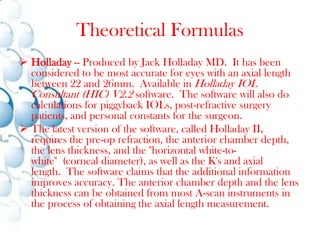
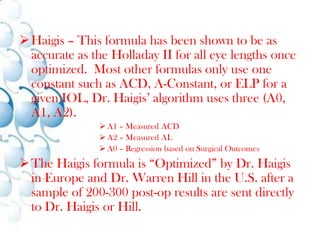
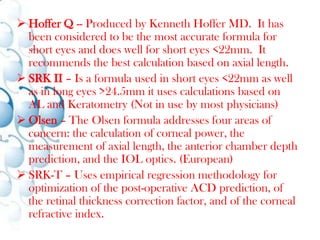
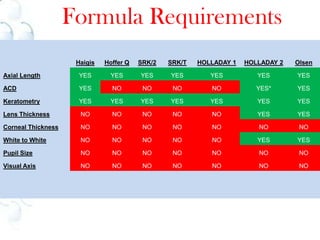
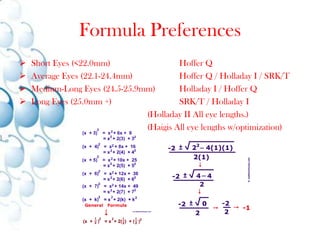
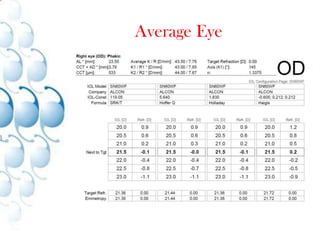
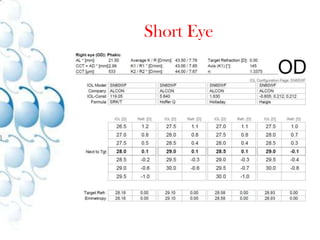
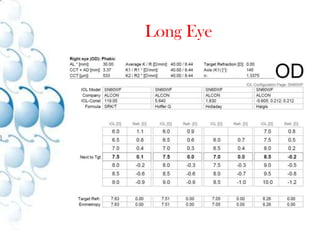
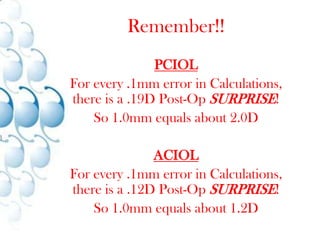
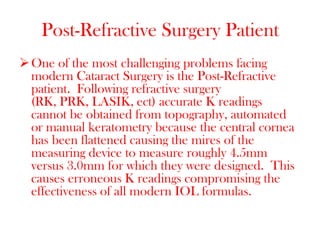
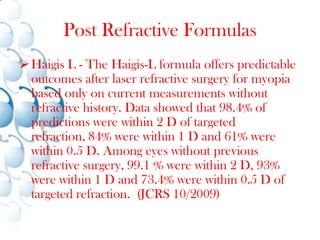
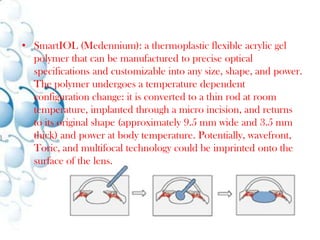
This document discusses optical biometry measurements and their use in determining appropriate intraocular lens (IOL) calculations and selections. It provides an overview of biometry techniques such as ultrasound and optical methods, compares their accuracy advantages, and outlines considerations for different eye anatomies and conditions. Formulas for calculating IOL power are examined, including preferences for different eye lengths. Challenges in post-refractive surgery patients are also addressed.