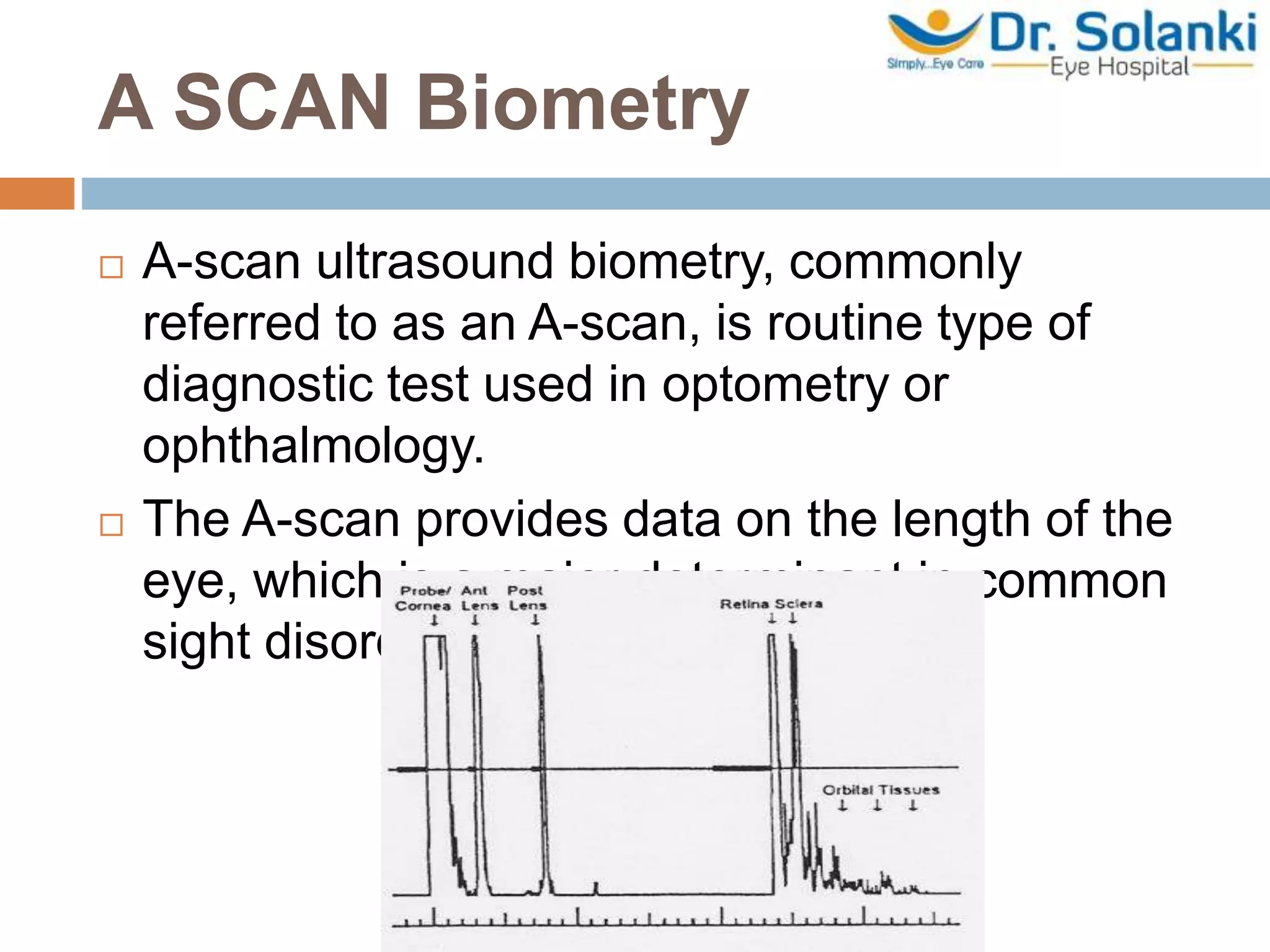
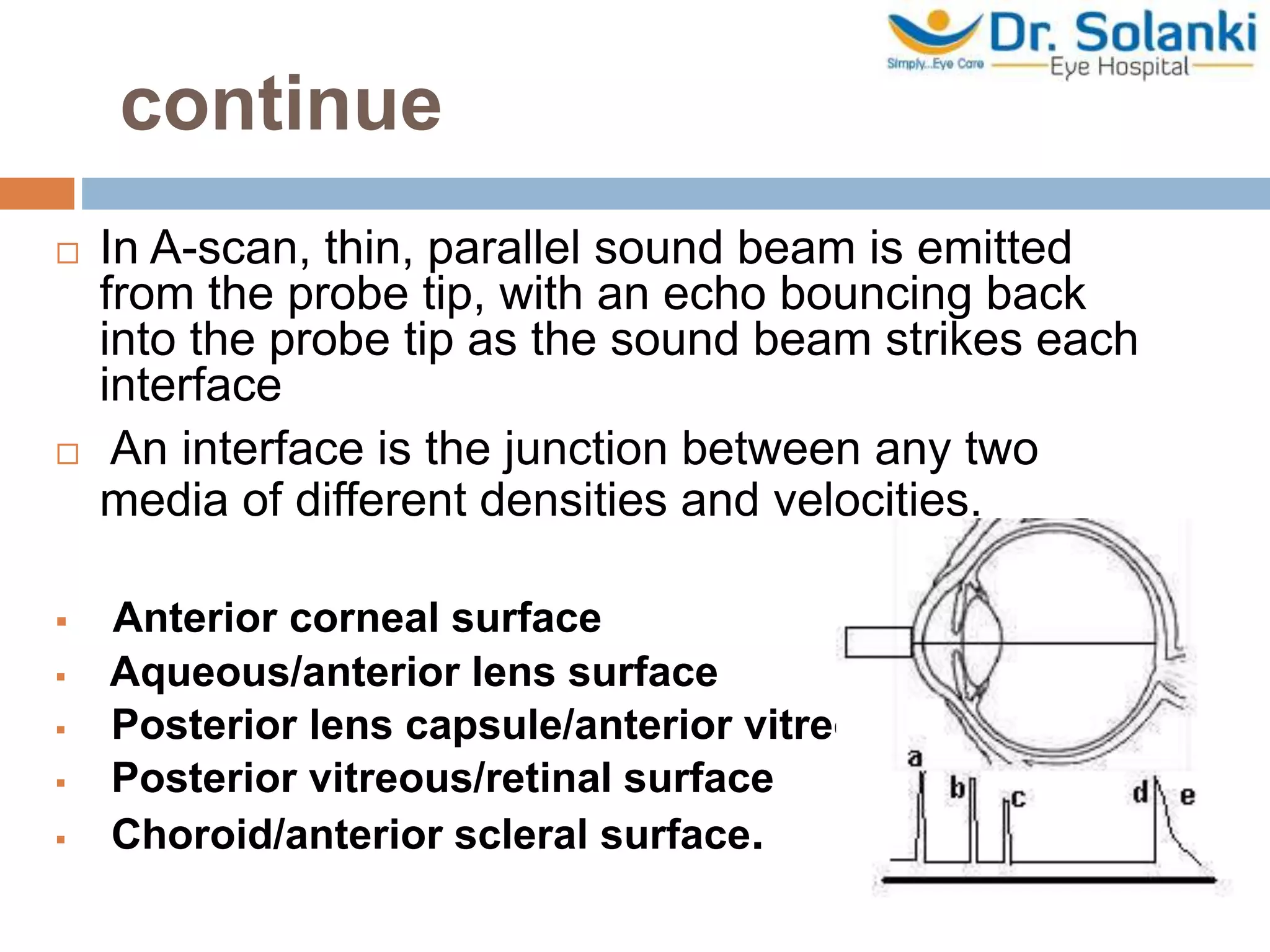
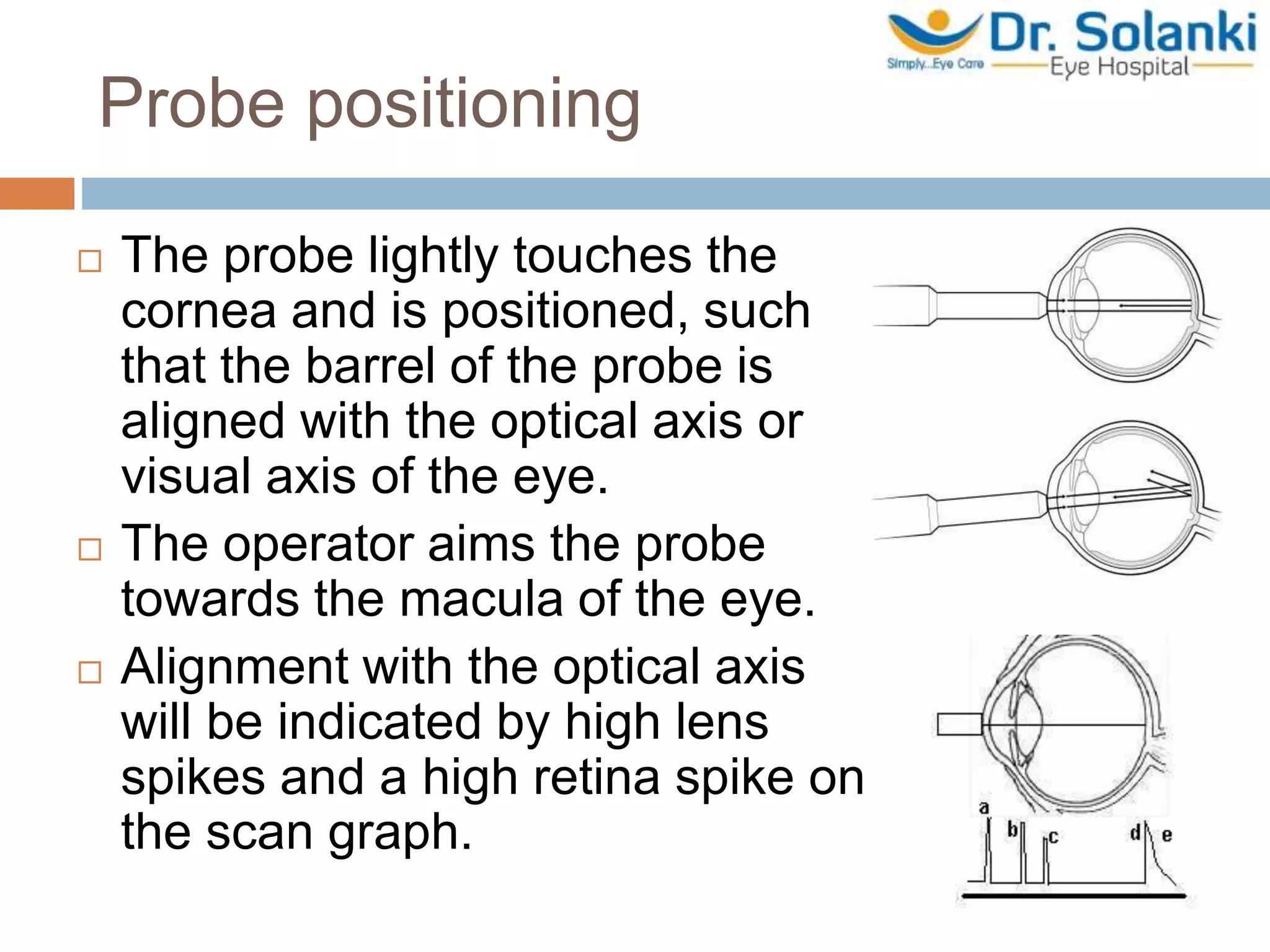
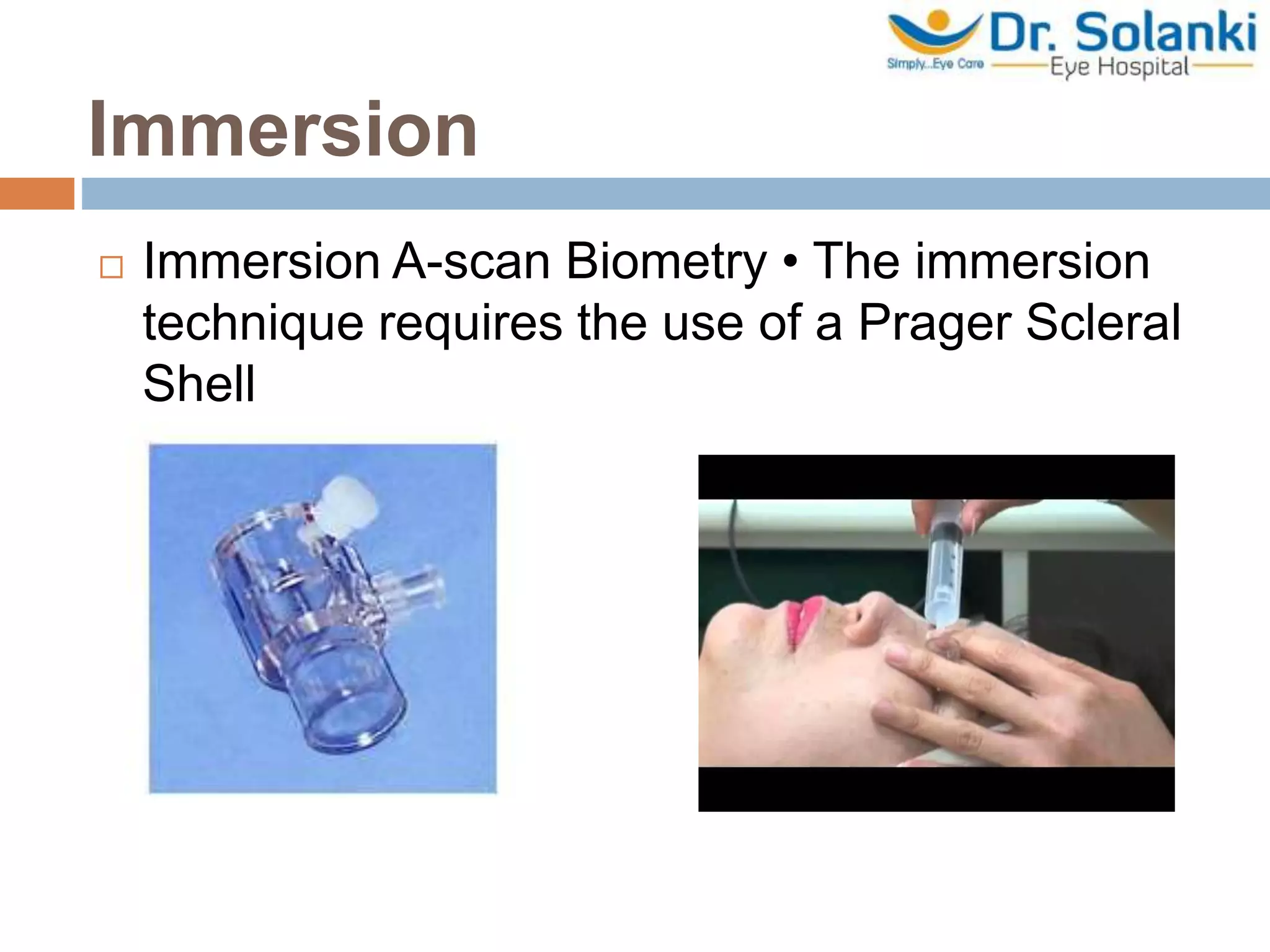
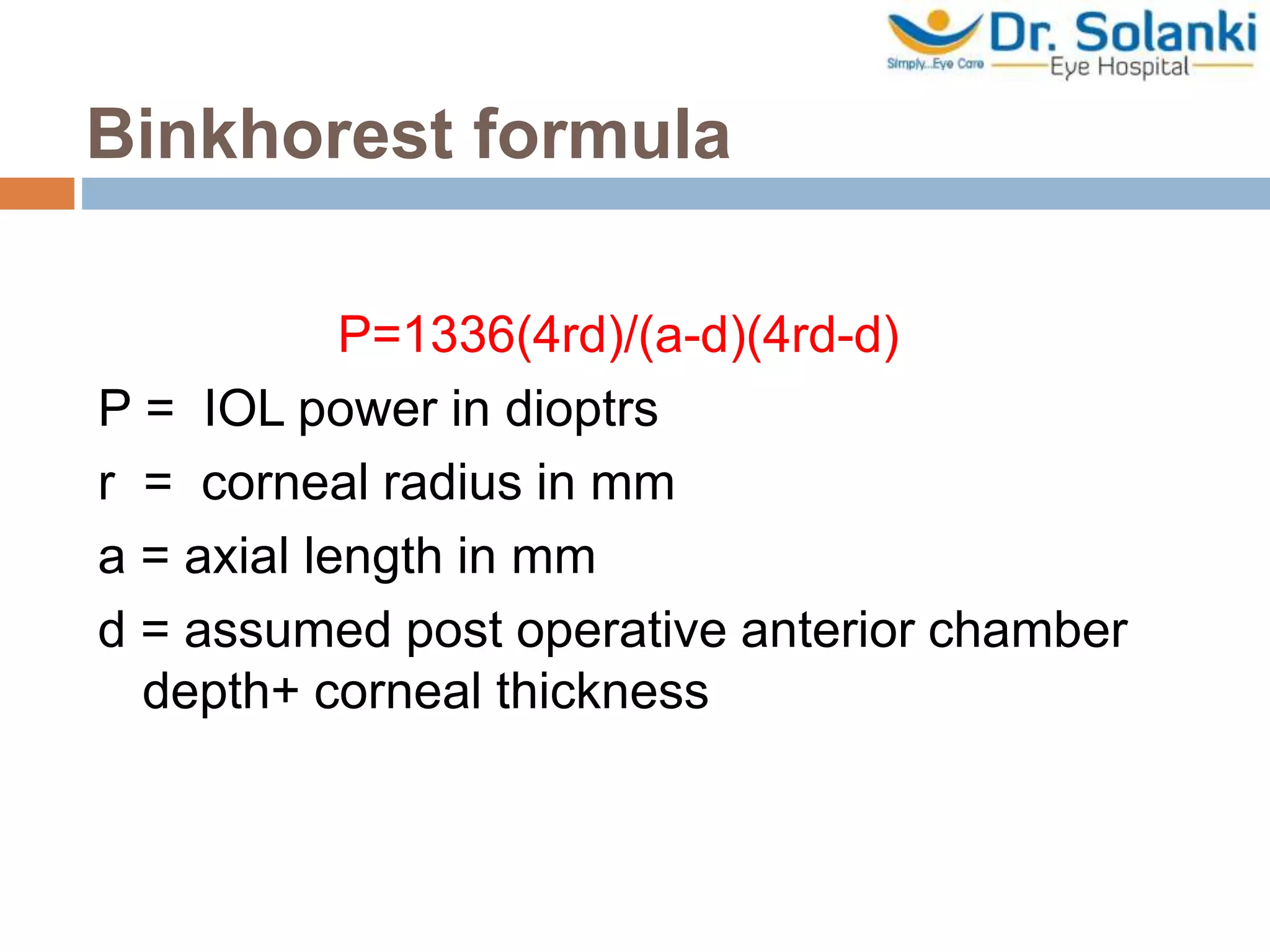
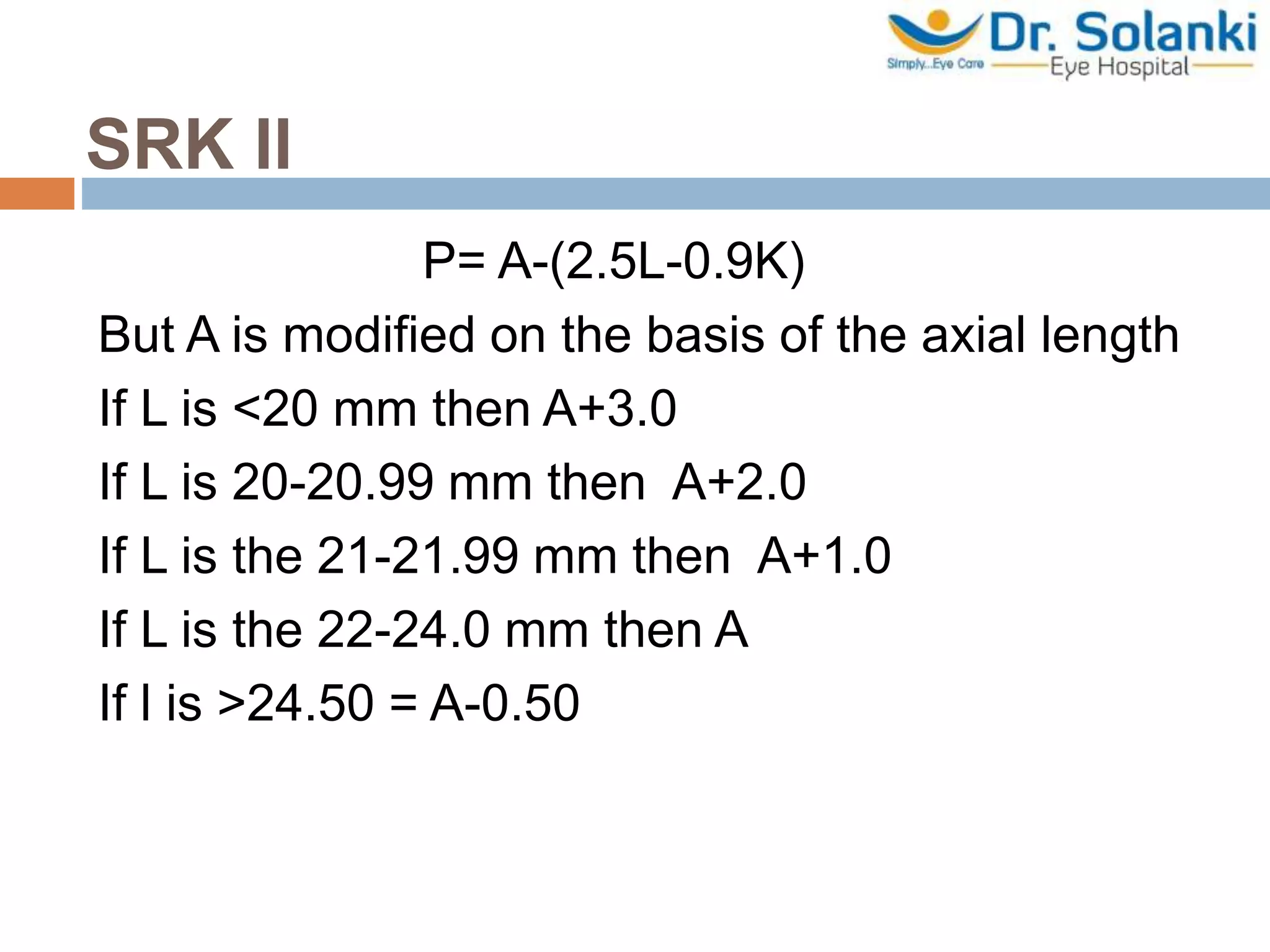
A-scan biometry is an ultrasound test used to measure the length of the eye, which is important for determining treatments for sight disorders. It works by emitting a sound beam into the eye and measuring the echoes that bounce back from different structures. The measurements of axial length, corneal curvature, and estimated lens position are used to calculate the ideal intraocular lens power needed after cataract surgery. Accuracy is important as even small errors in measurement can significantly impact the calculated lens power. Different formulas exist to relate the biometry measurements to the appropriate lens power, with newer regression formulas found to be most accurate.