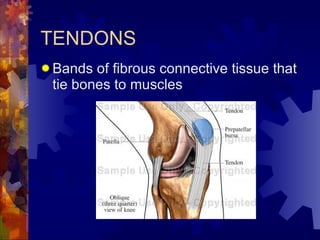
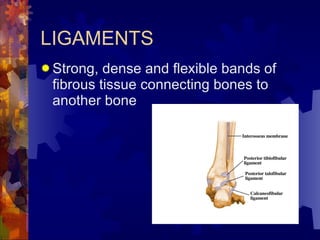
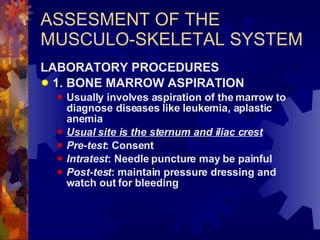
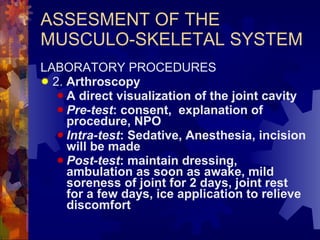
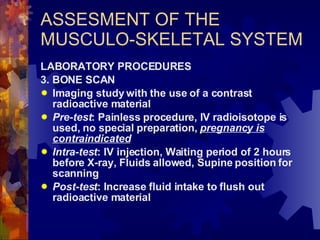
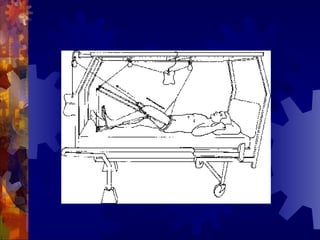
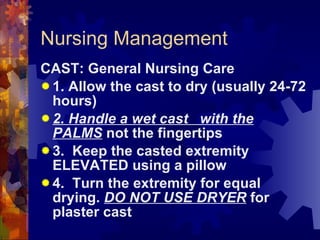
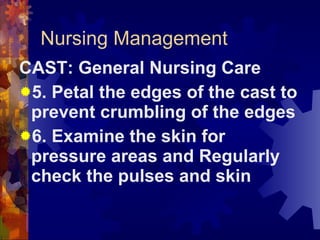
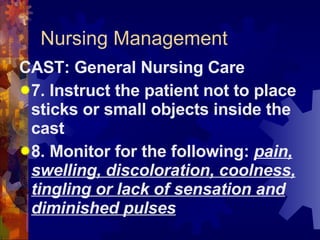
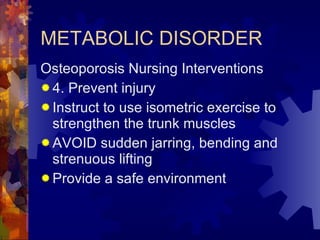
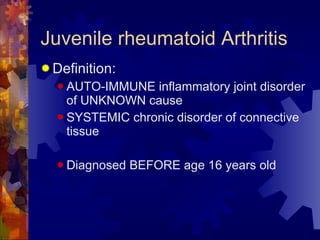
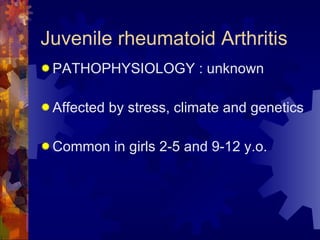
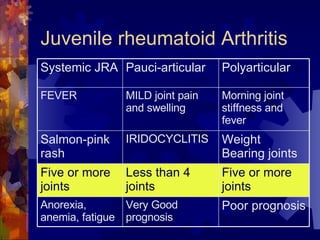
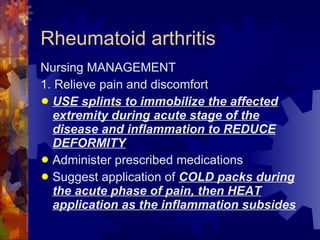
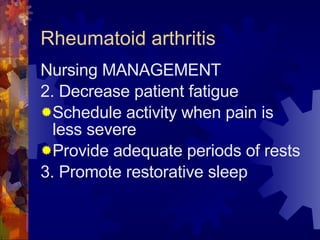
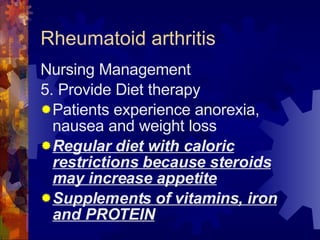
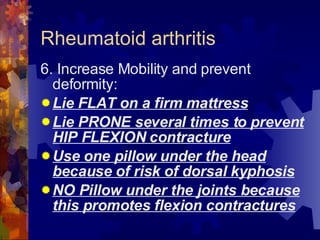
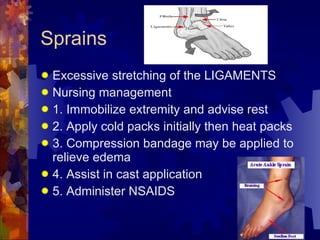
The document discusses the musculoskeletal system, including its main components like muscles, bones, tendons, and joints. It describes the three main types of muscles and functions of bones and joints. Assessment of the musculoskeletal system includes inspection, palpation, range of motion testing, and evaluation of gait and posture. Common musculoskeletal problems like pain, impaired mobility, and self-care deficits are discussed along with relevant nursing management.