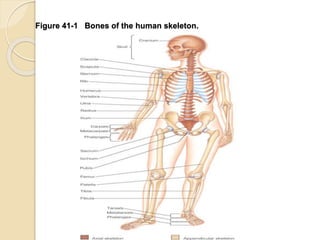
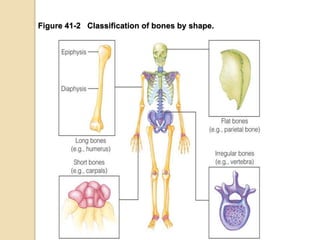
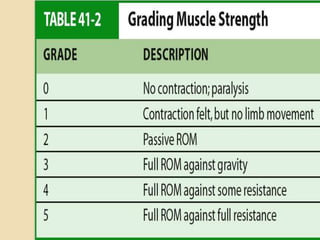
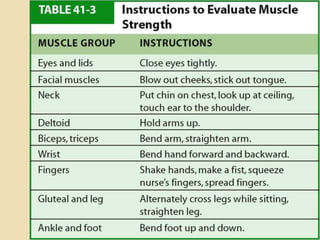
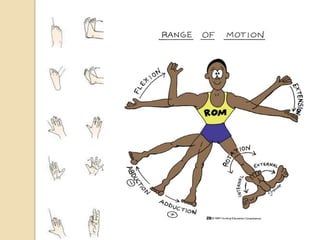
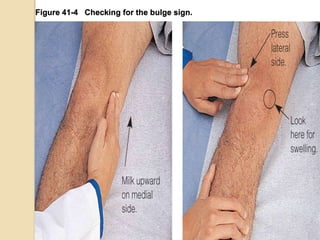
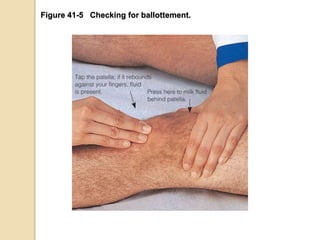
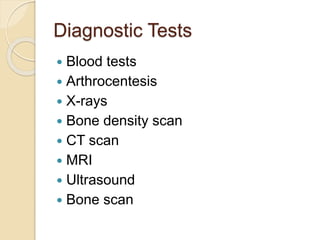
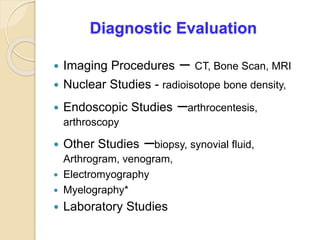
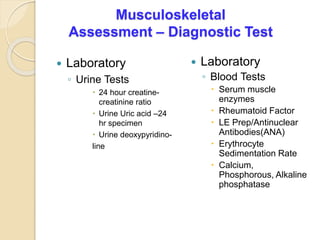
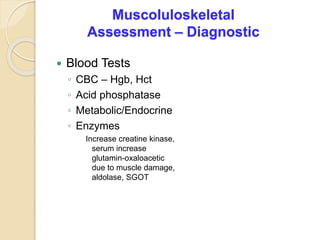
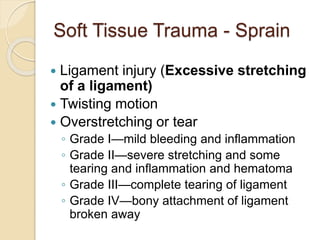
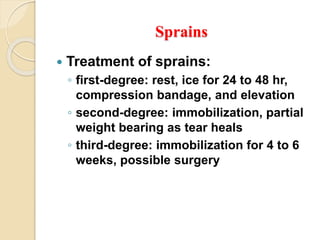
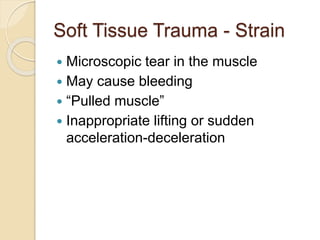
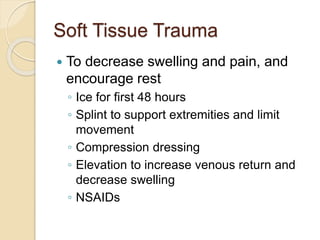
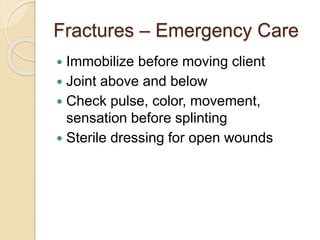
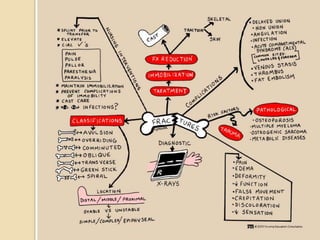
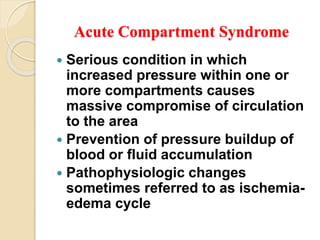
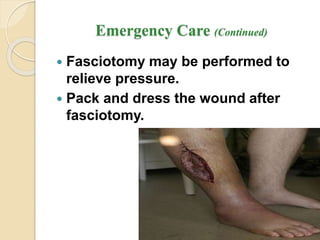
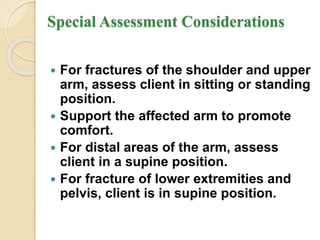
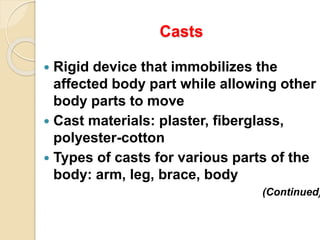
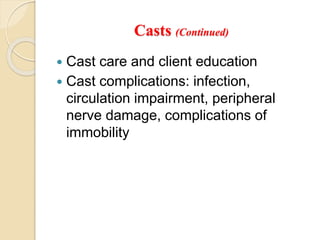
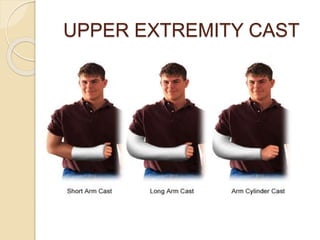
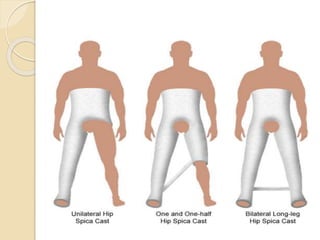
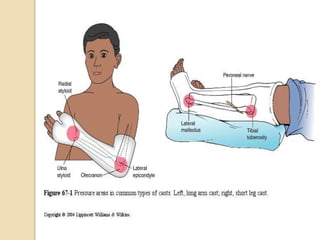
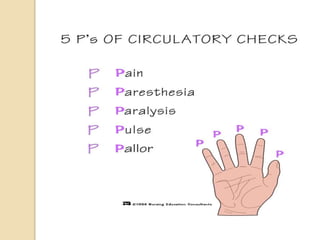
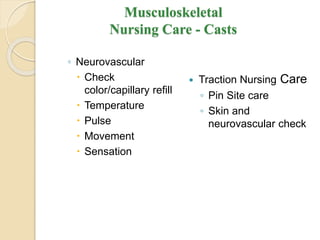
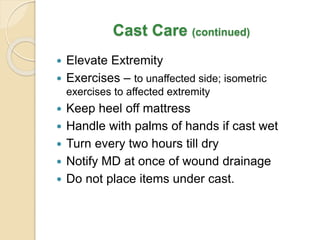
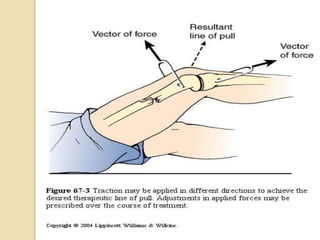
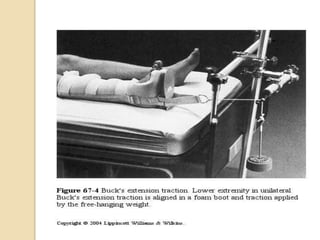
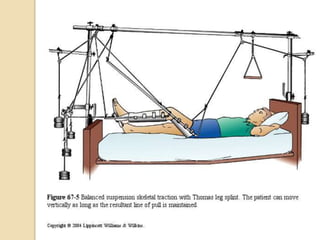
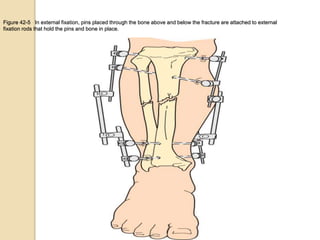
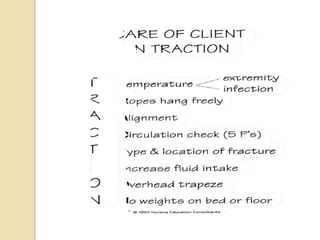
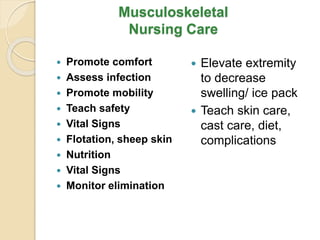
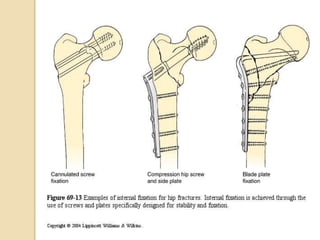
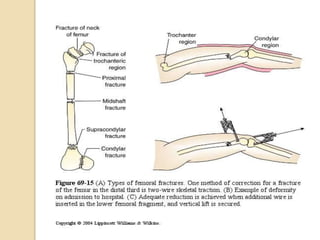
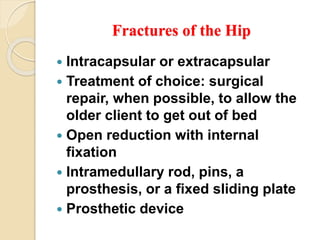
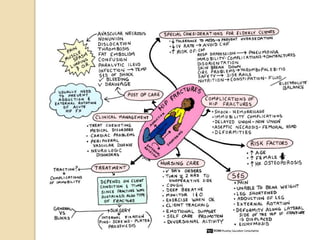
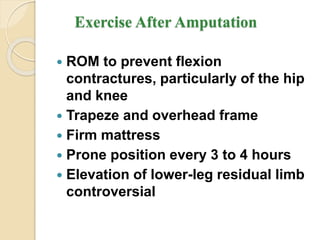
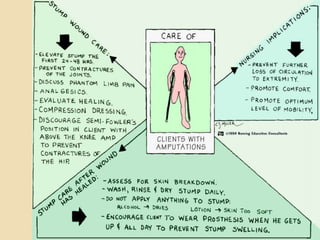
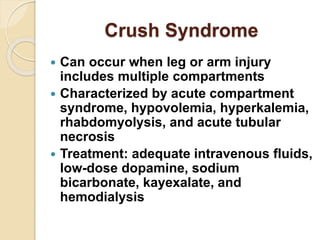
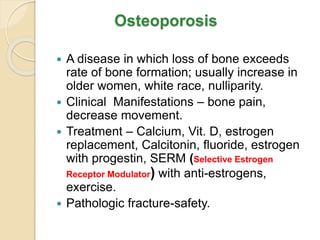
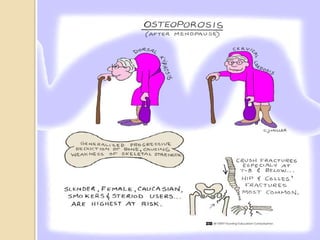
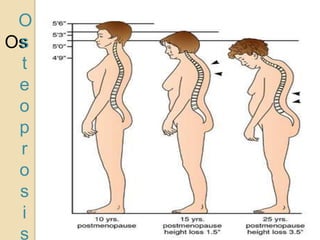
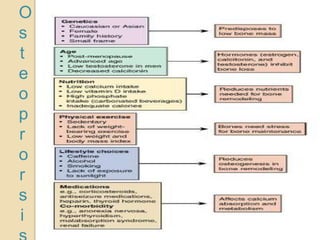
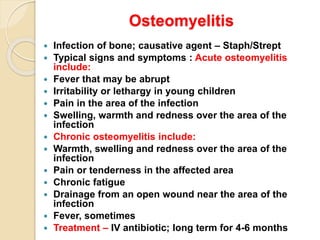
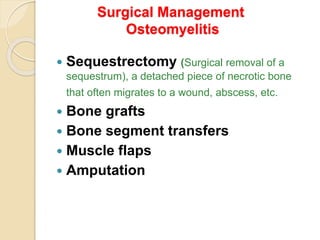
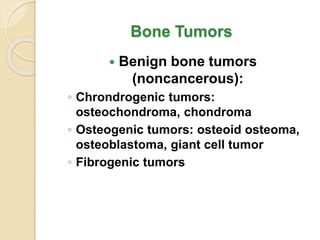
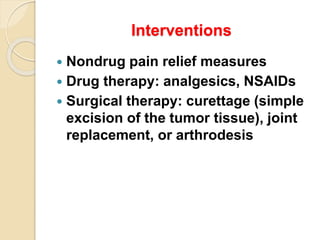
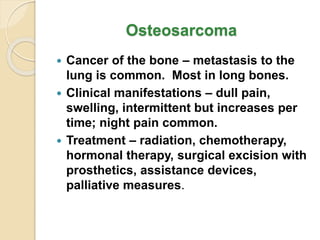
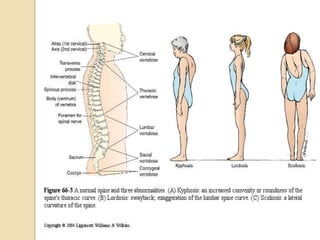
The document covers the musculoskeletal system assessment and disorders, detailing the structure and function of the skeletal system, bone types, and diagnostic evaluations for musculoskeletal issues. It discusses assessment strategies, treatment protocols for soft tissue trauma and fractures, and highlights the importance of proper nursing interventions and patient education. Additionally, it addresses complications such as acute compartment syndrome and phantom limb pain, emphasizing both medical and rehabilitative management.