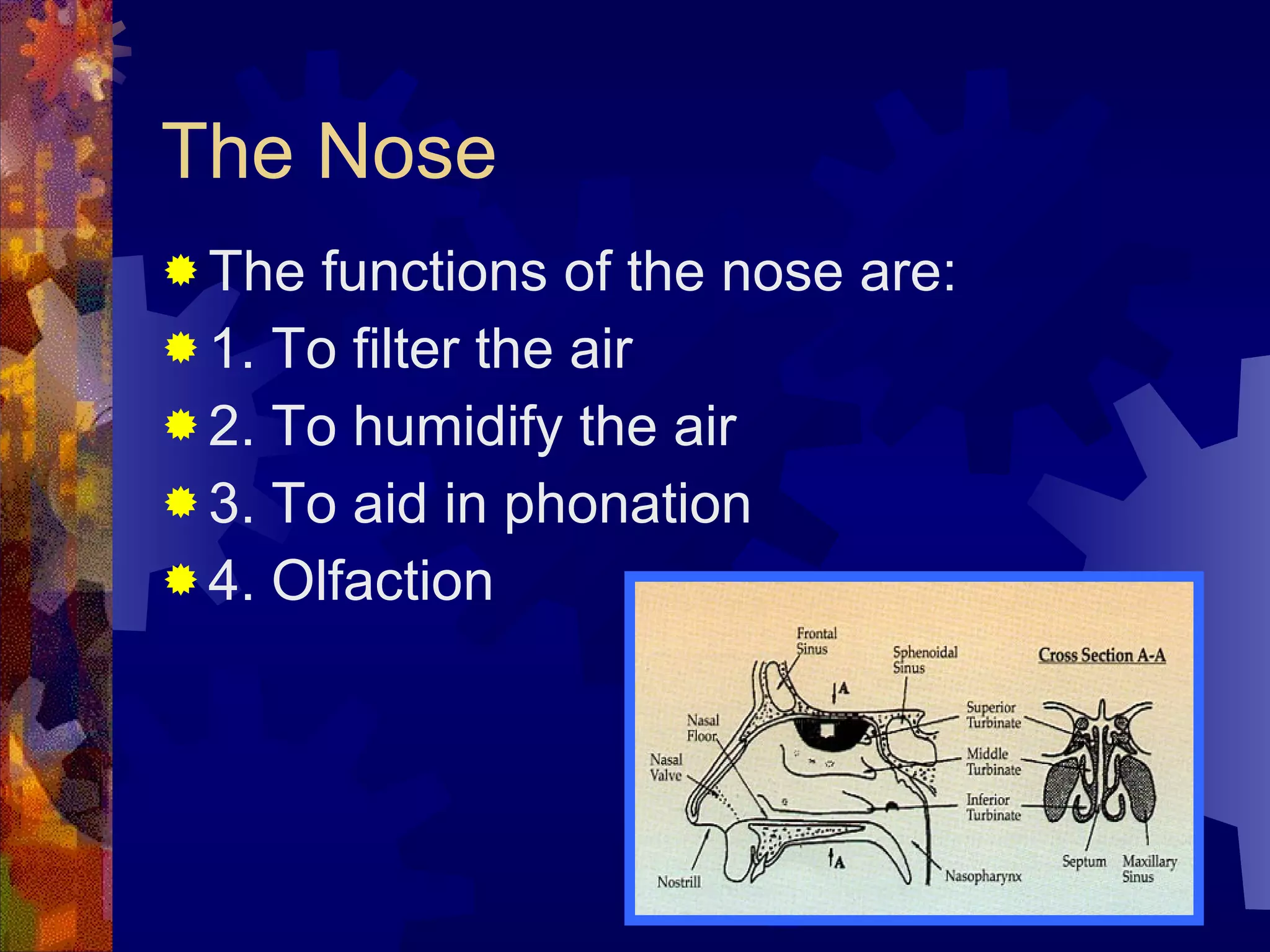
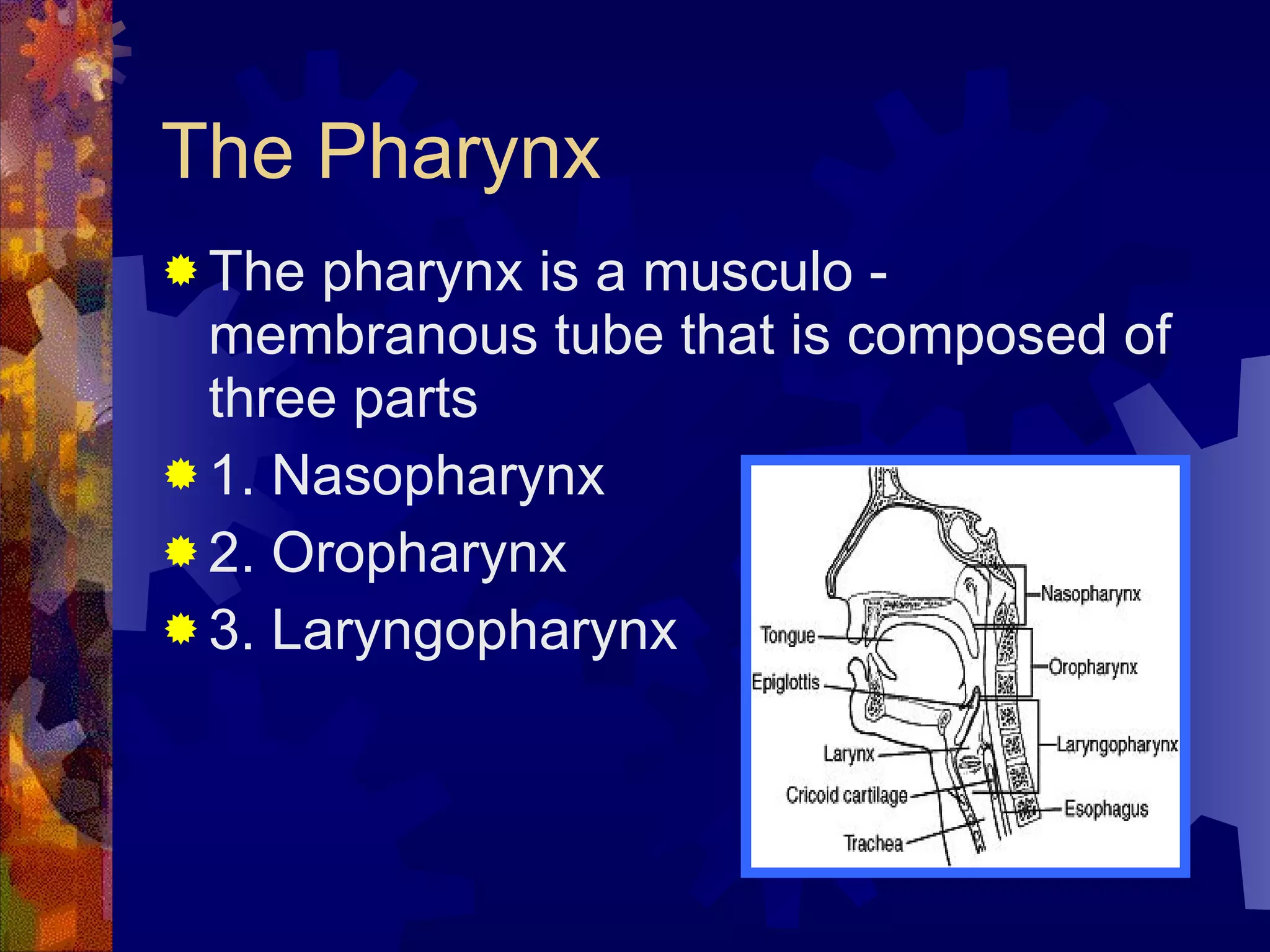
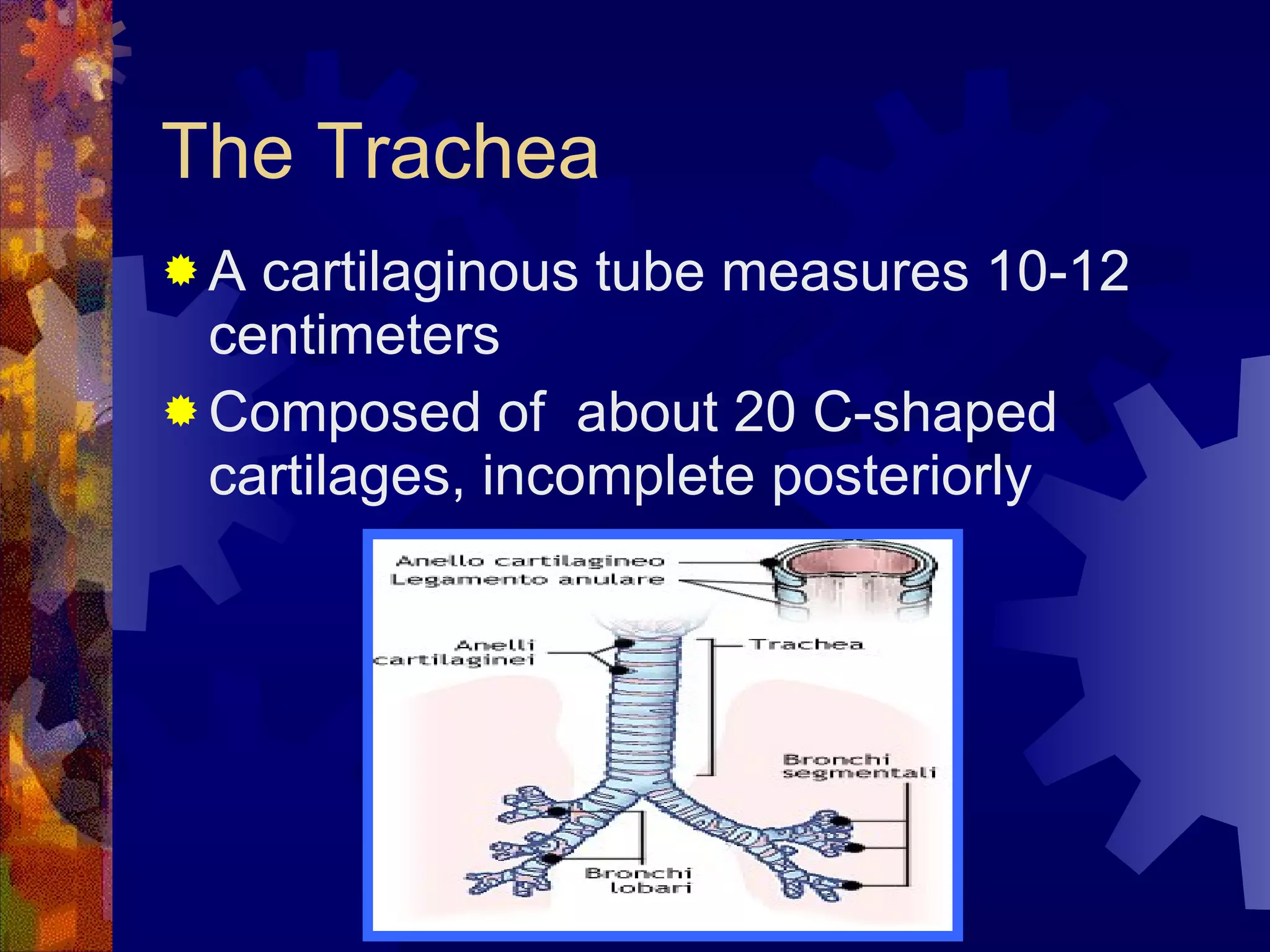
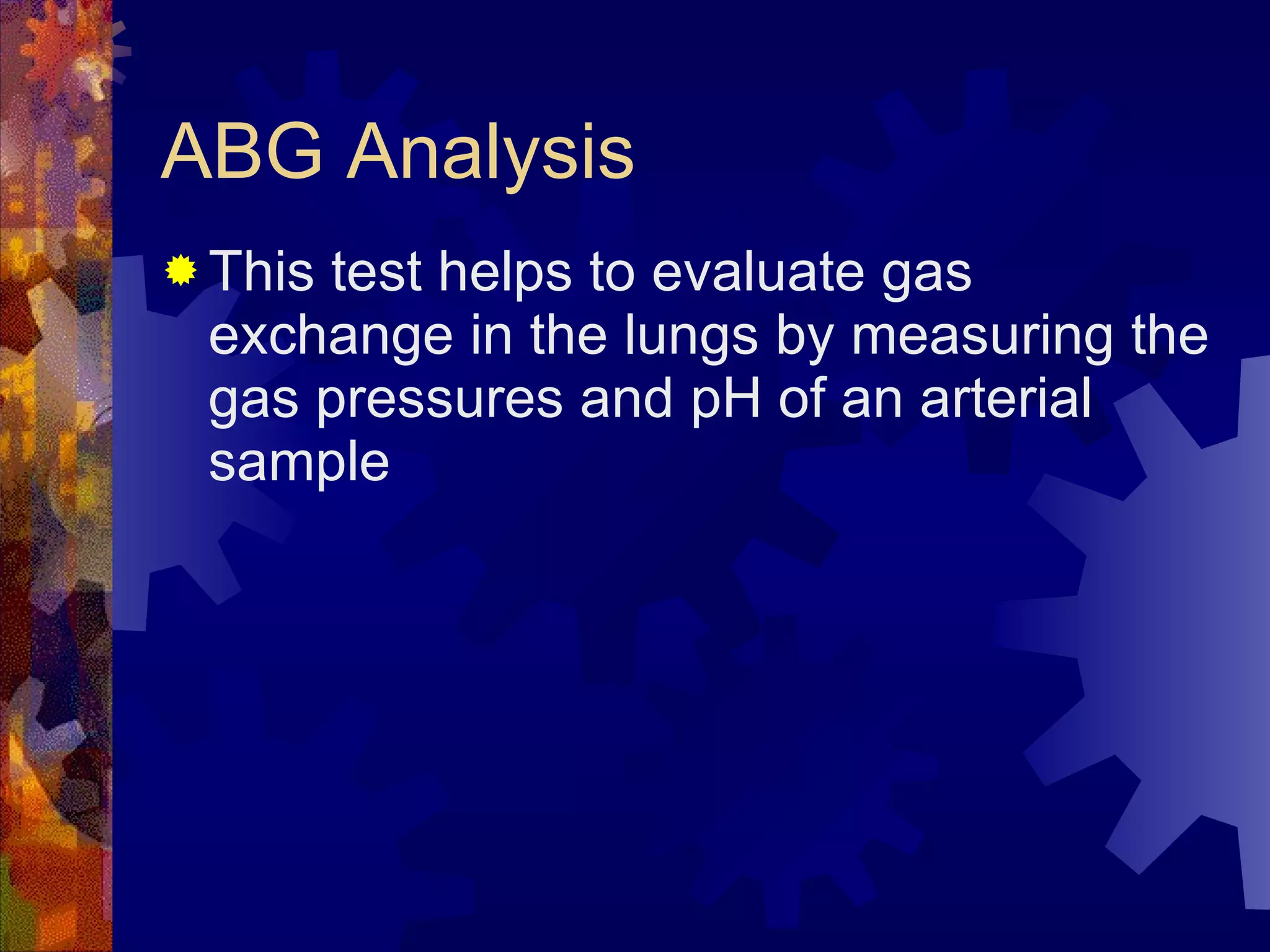
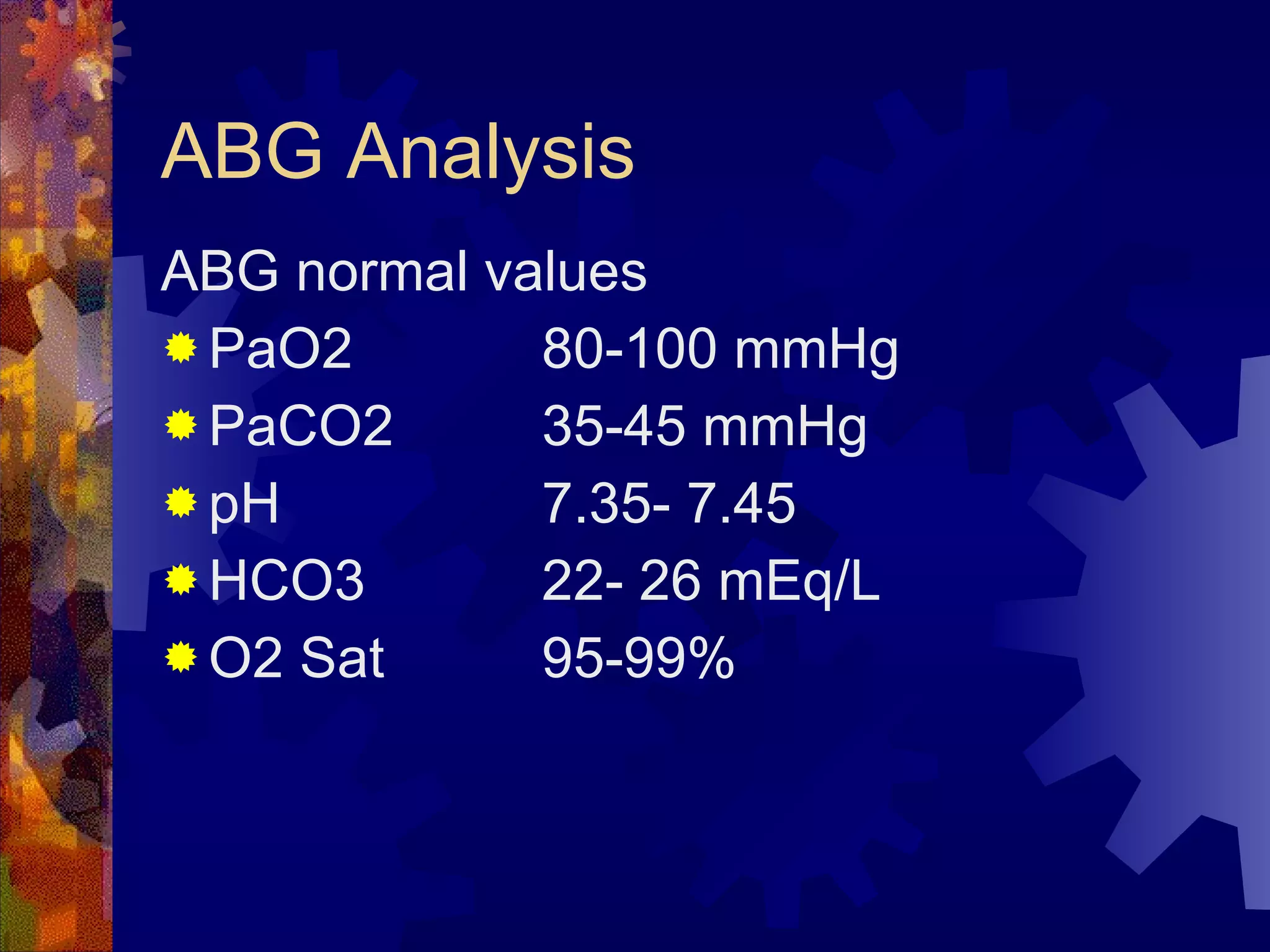
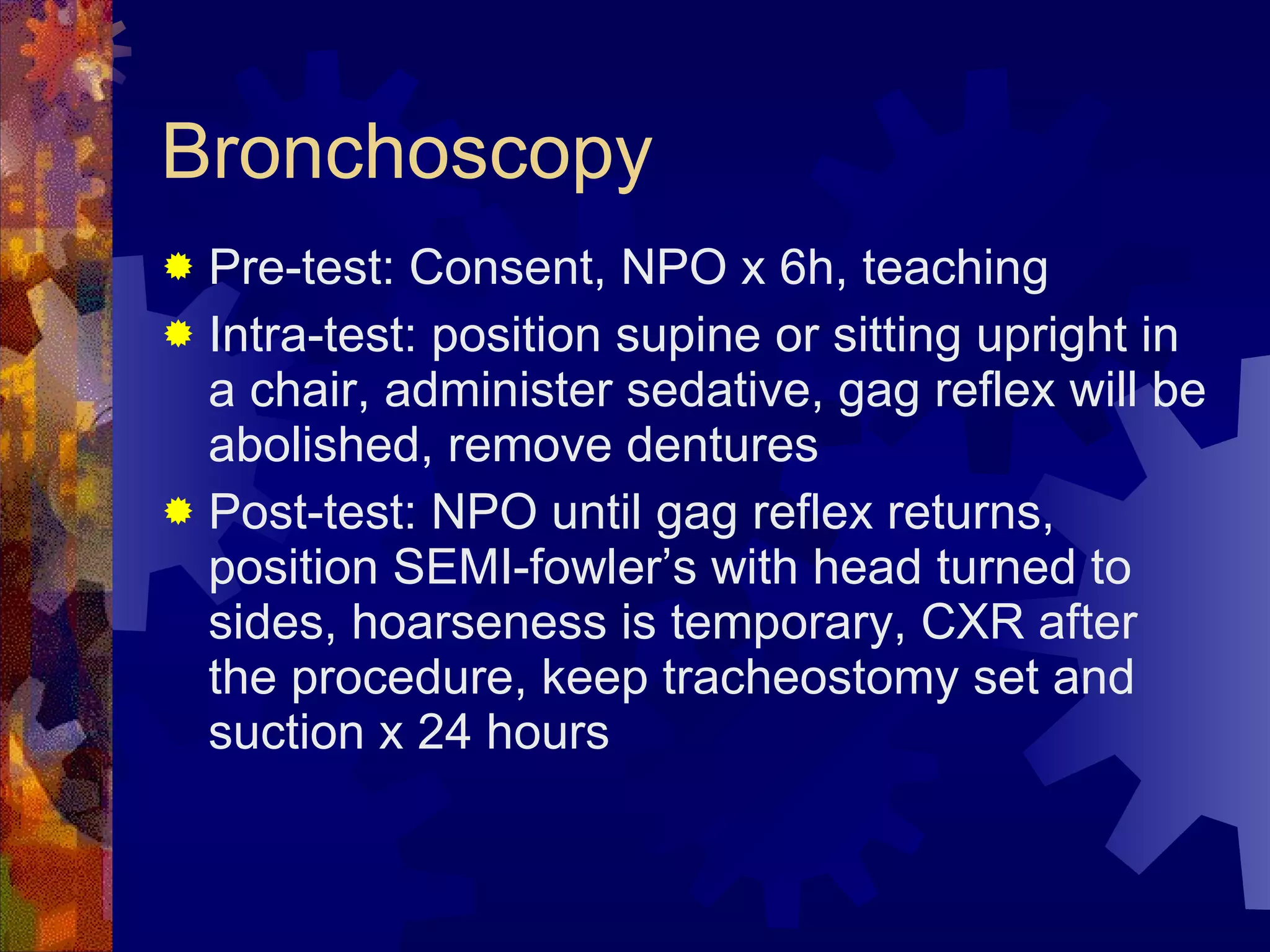
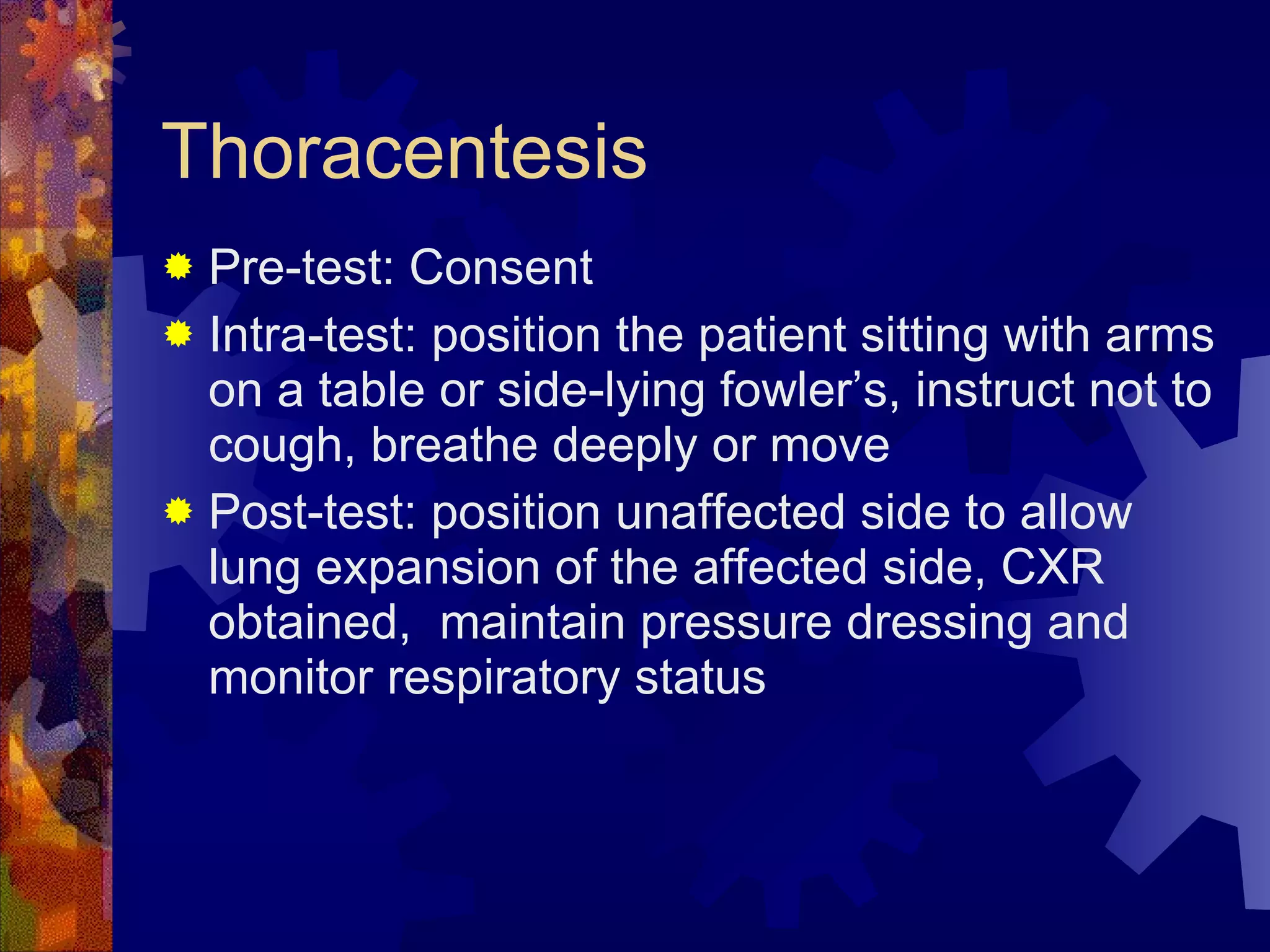
The document provides an overview of the respiratory system including anatomy, physiology, common conditions, diseases, and nursing management. It discusses the upper and lower respiratory tract, respiratory assessment, laboratory tests, common problems like dyspnea, cough and sputum production, and conditions such as tonsillitis, sinusitis, and laryngeal cancer. Nursing interventions focus on airway management, communication techniques, nutrition, and monitoring for post-operative complications.