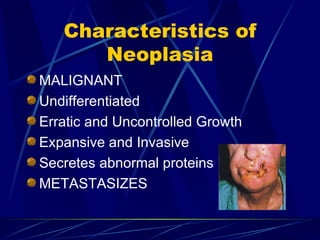
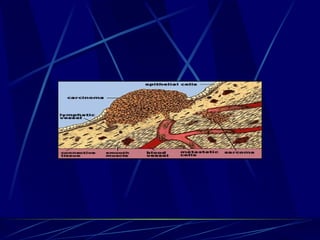
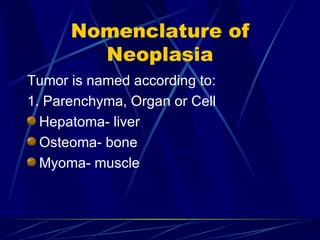
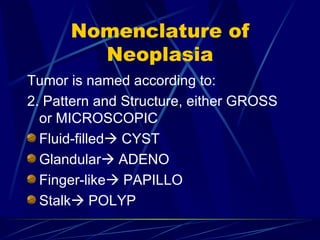
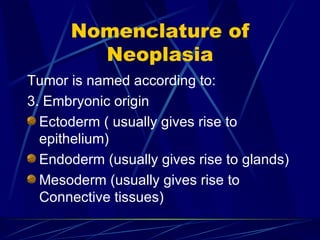
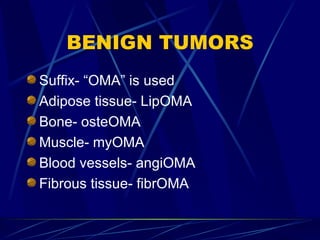
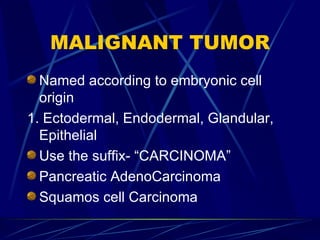
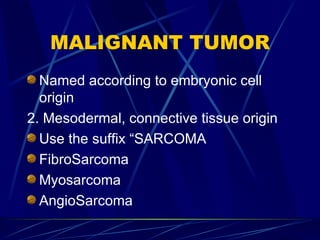
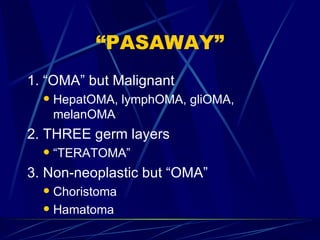
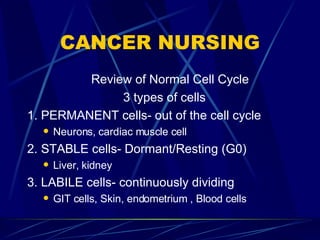
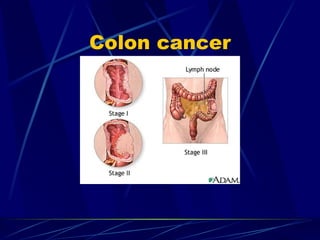
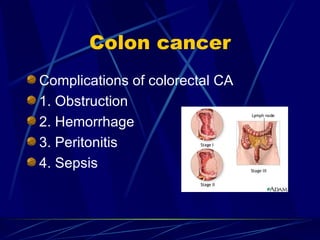
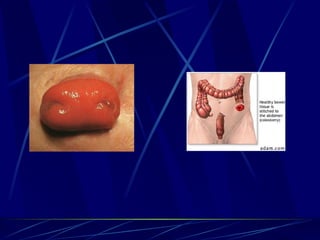
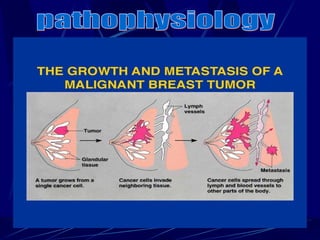
This document provides an overview of oncology nursing and cancer care. It discusses the basics of cancer including characteristics of benign and malignant tumors. It covers cancer diagnosis, staging, treatment including surgery, chemotherapy and radiation therapy. It also summarizes nursing interventions for common cancer complications and procedures such as colostomy care. Specific cancers like breast cancer and colon cancer are reviewed in terms of risk factors, pathophysiology, assessment findings, diagnosis, treatment and nursing management.