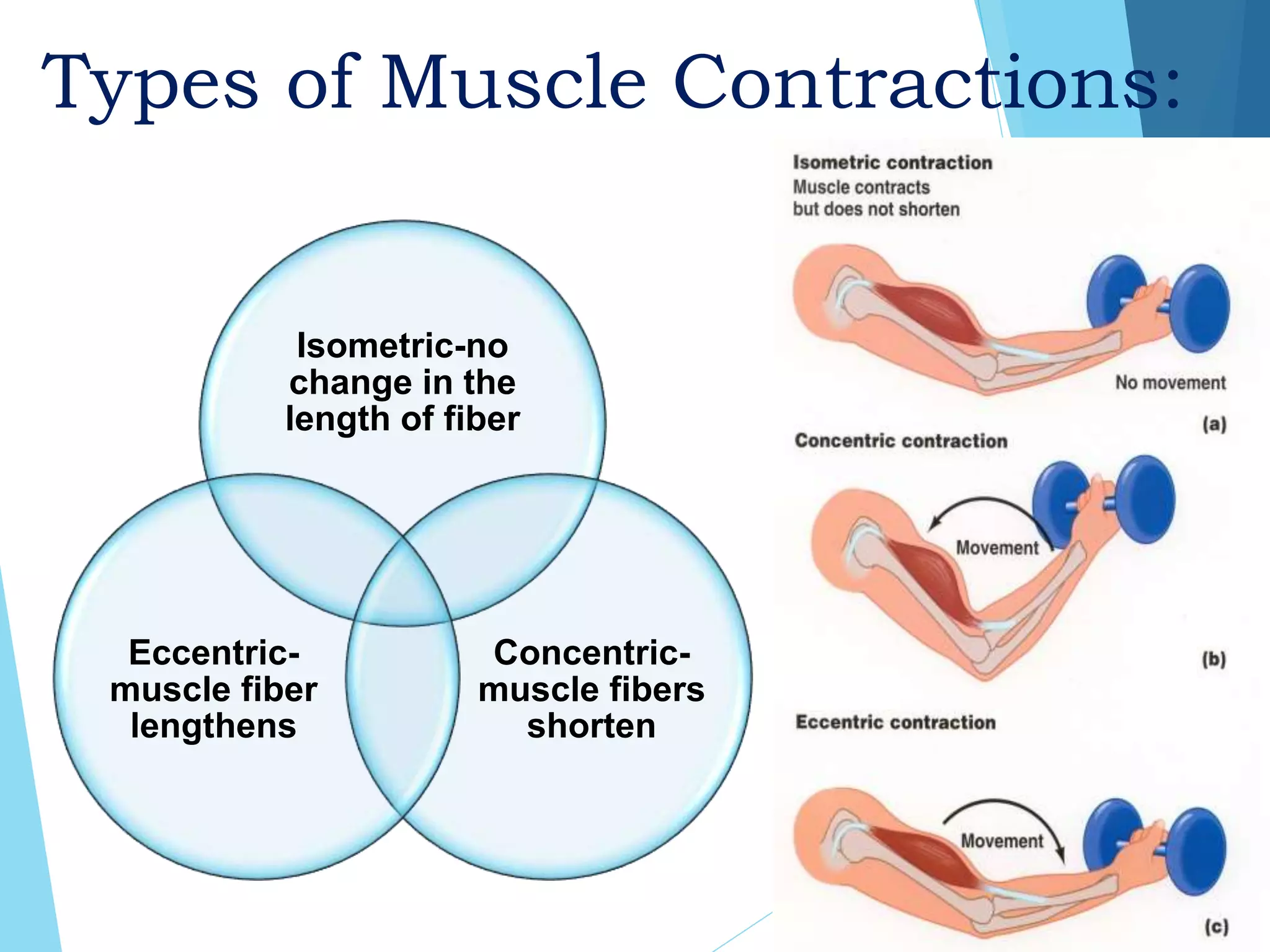
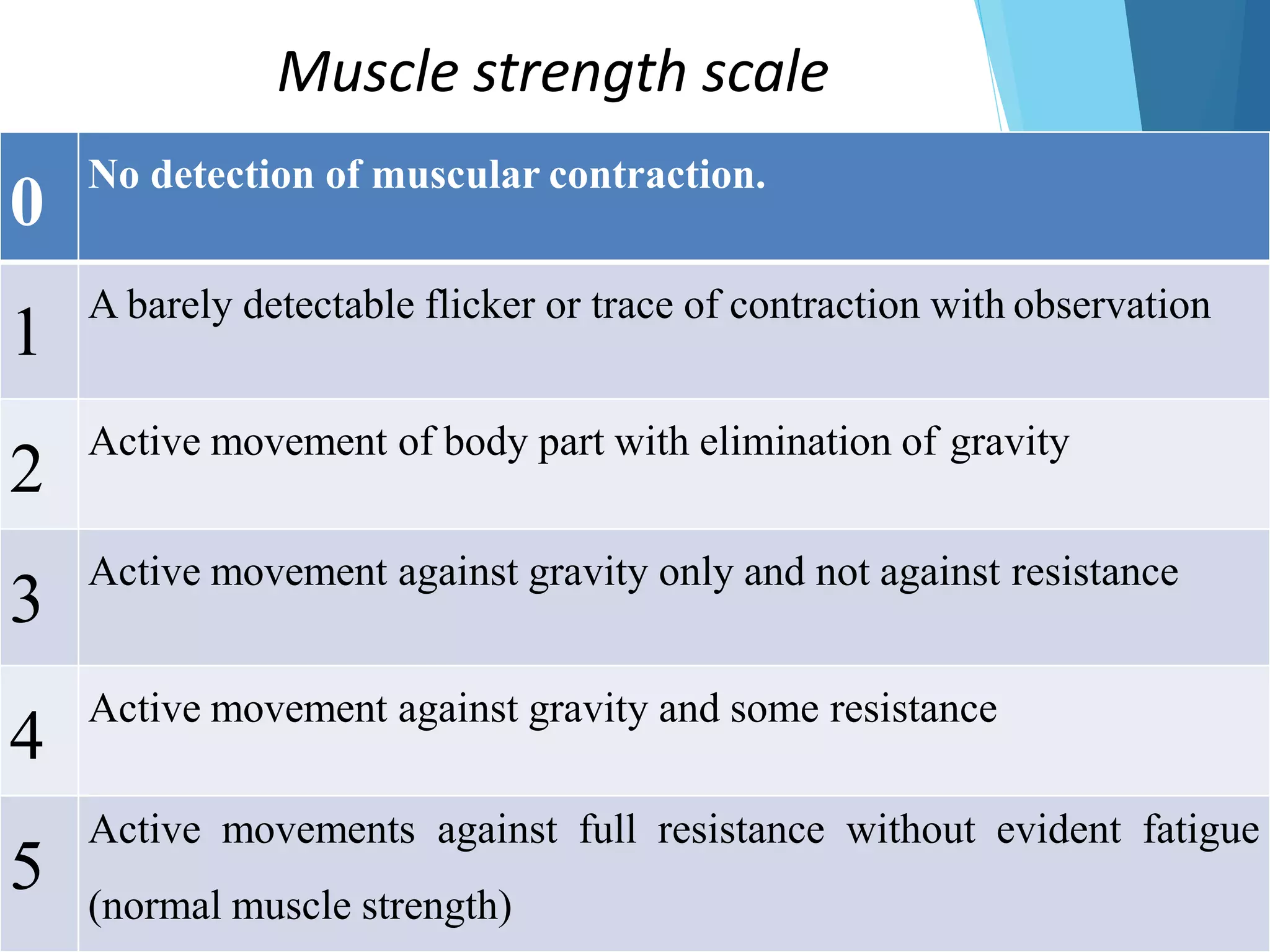
The document provides an overview of musculoskeletal assessment including the components of the musculoskeletal system, functions of muscles and bones, types of muscle contractions and classifications of joints. It describes approaches to subjective and objective assessment including inspection, palpation, range of motion assessment and special tests. Common chief complaints, effects on daily living, past medical history and medications are discussed for subjective data collection. The document also outlines various diagnostic studies for musculoskeletal conditions.