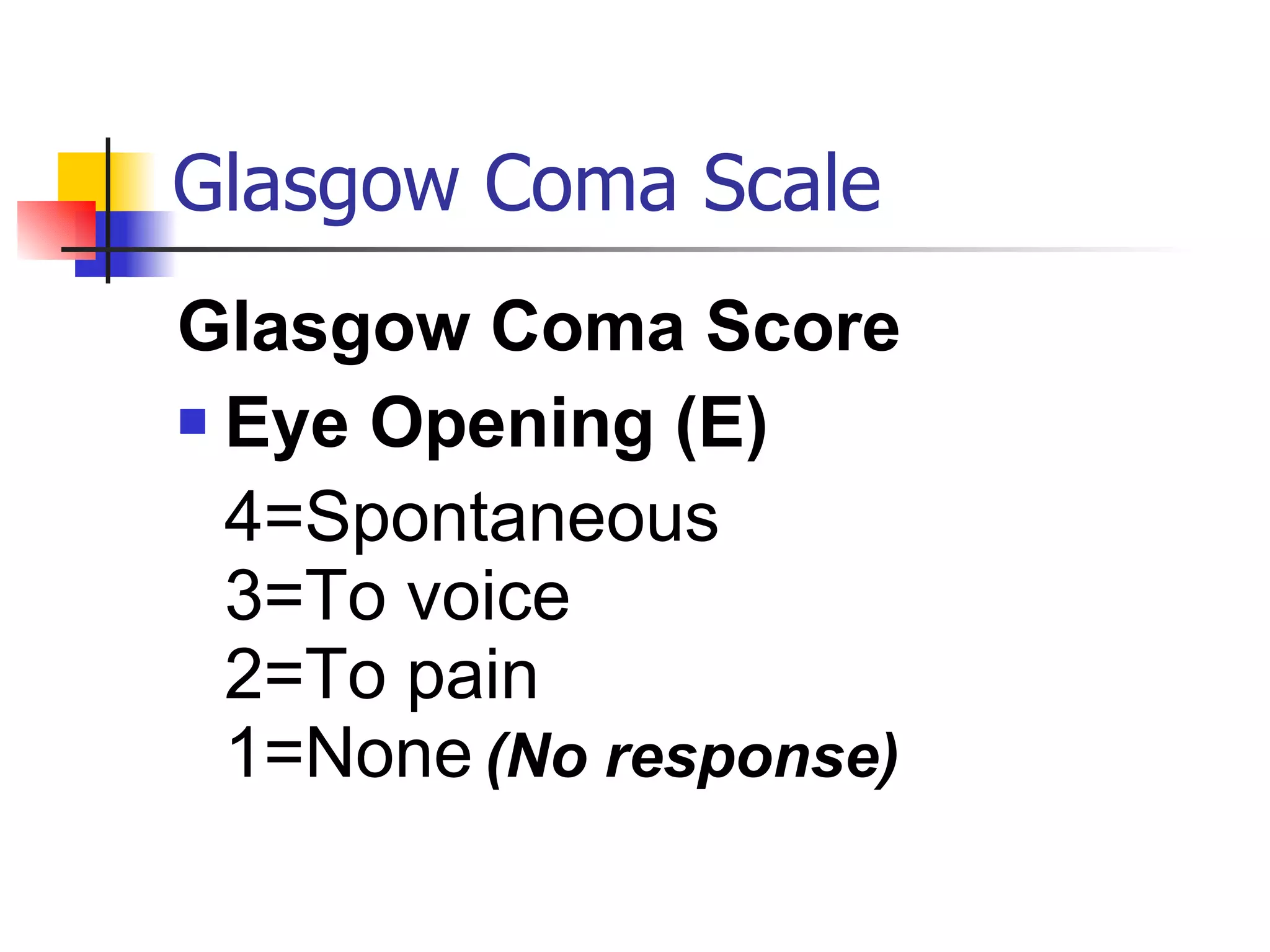
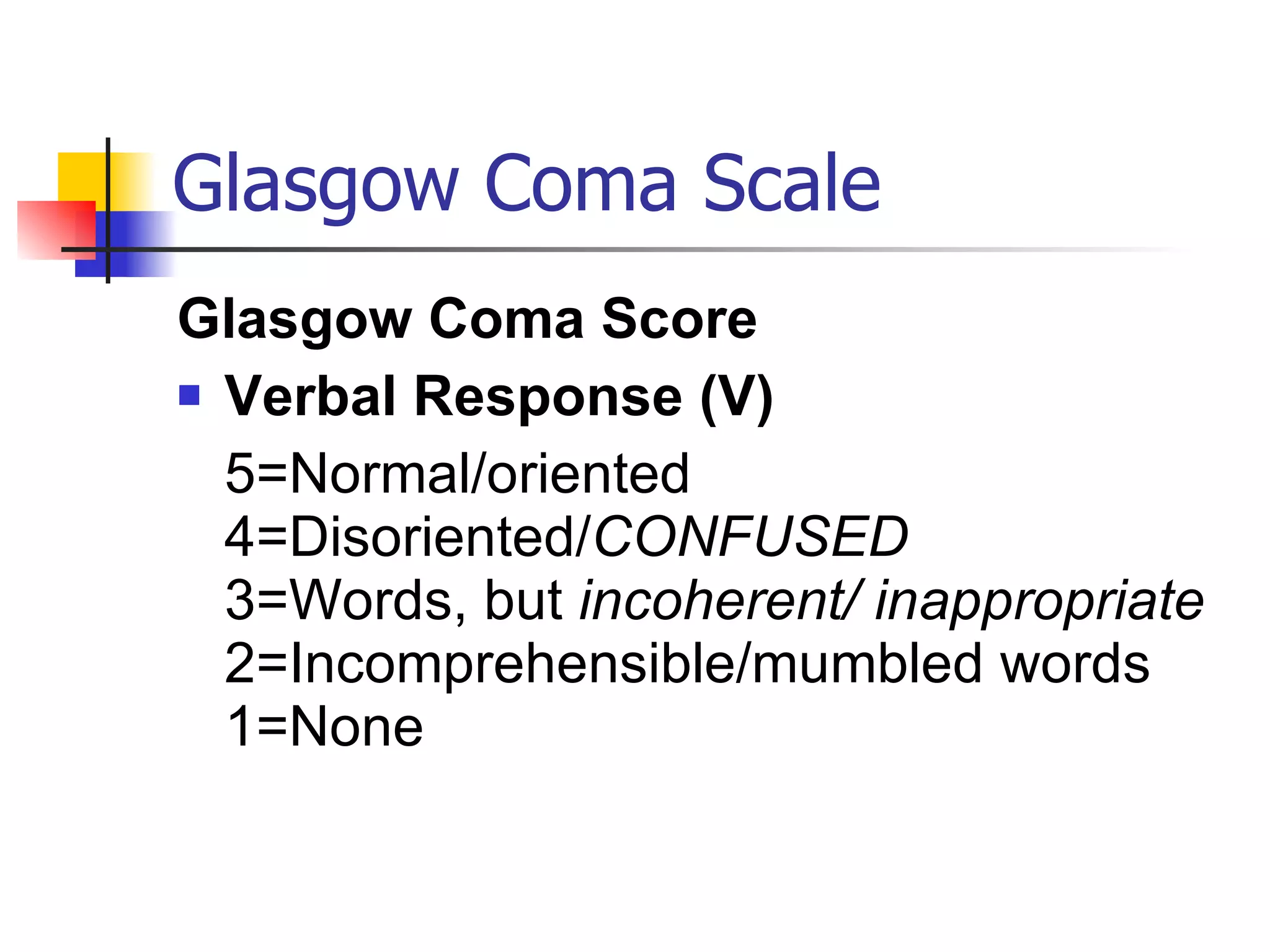
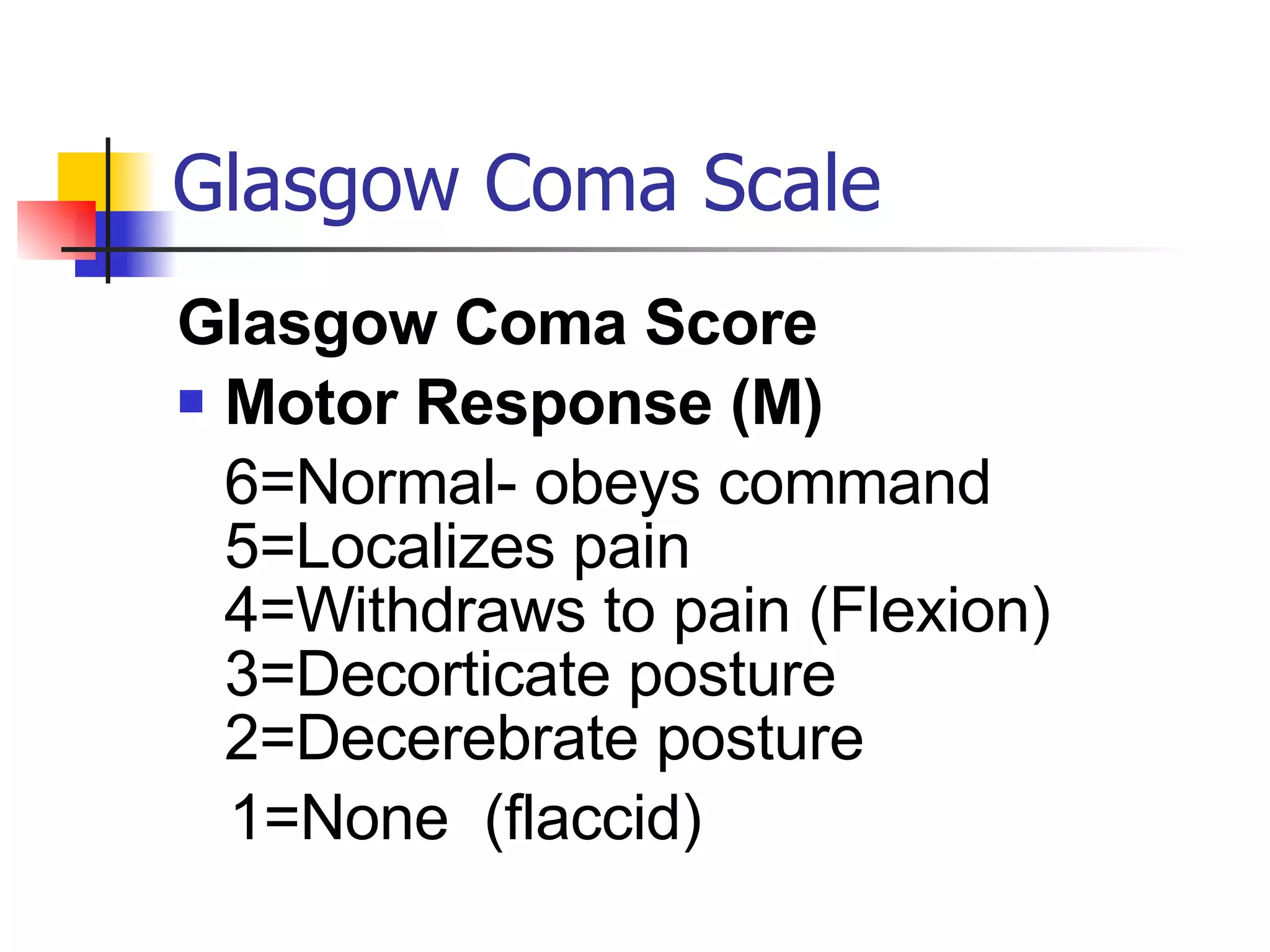
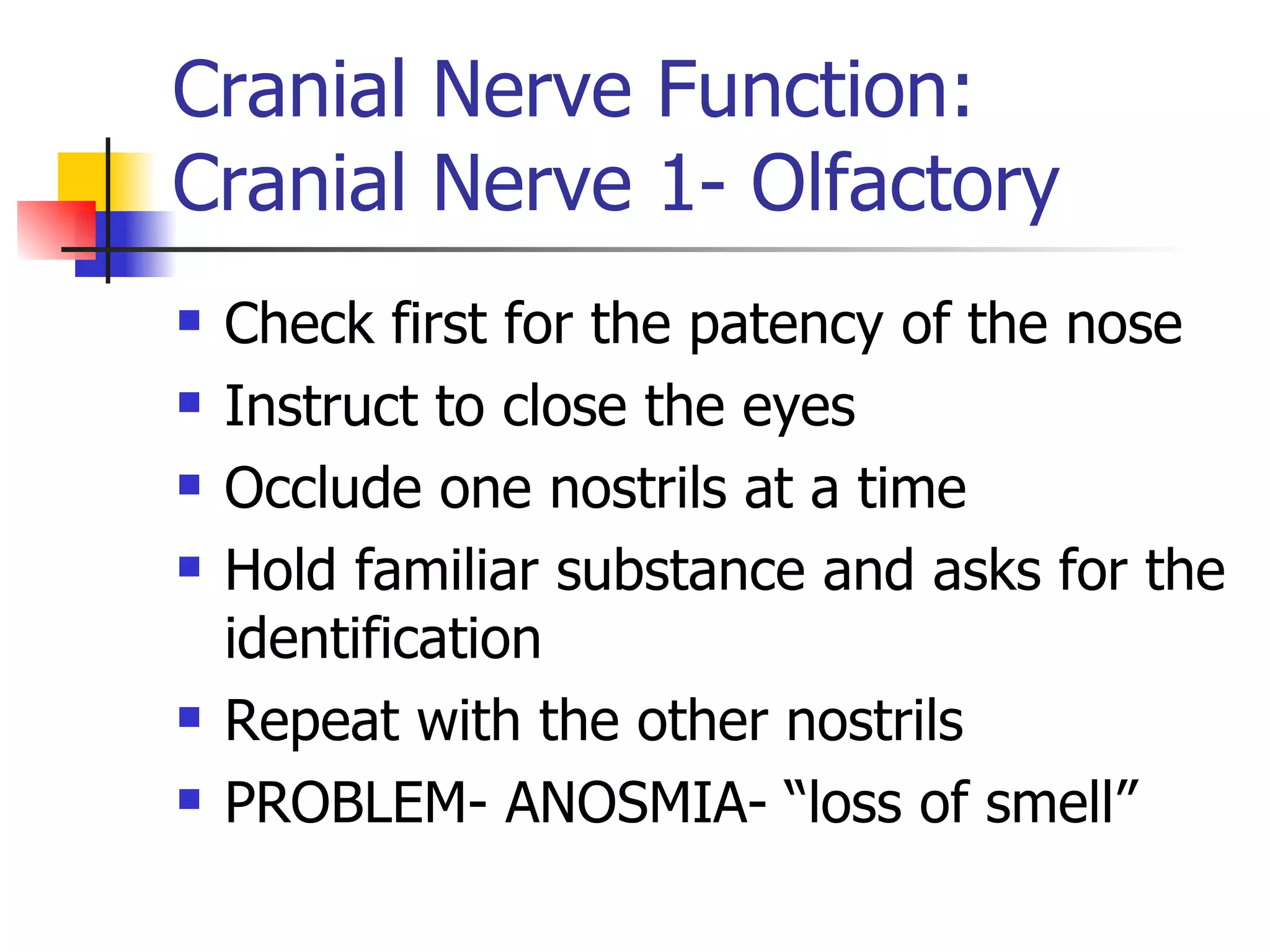
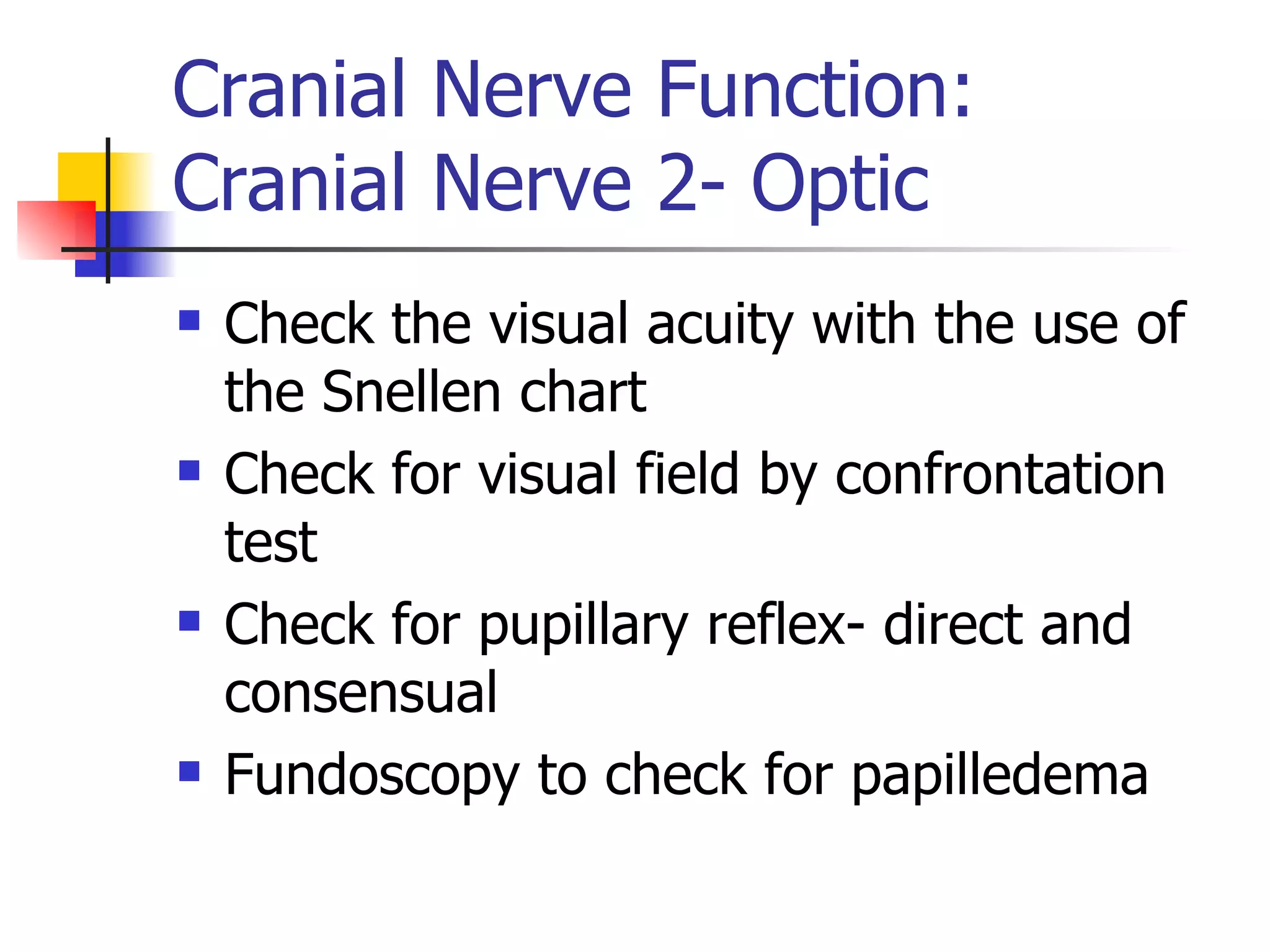
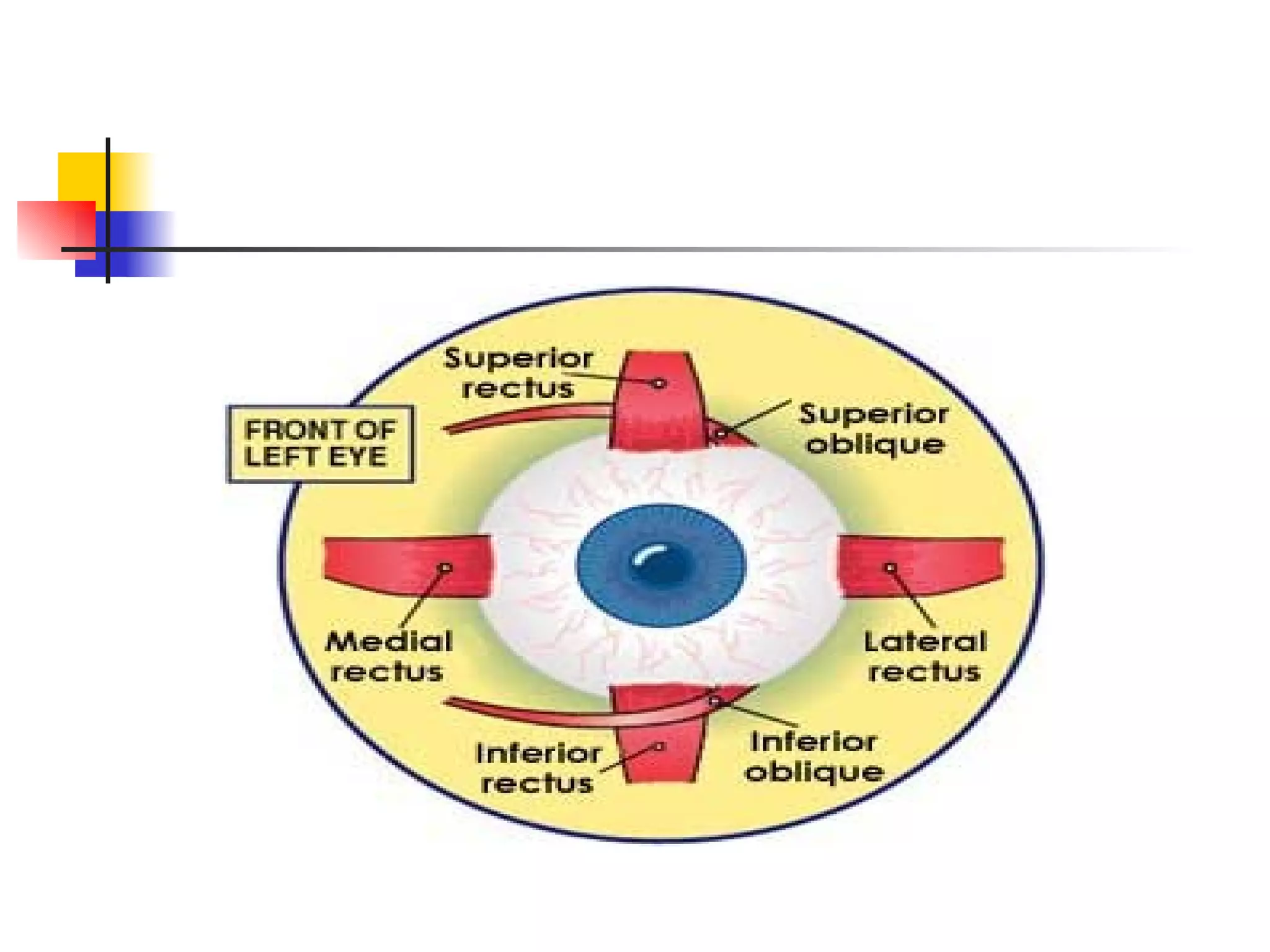
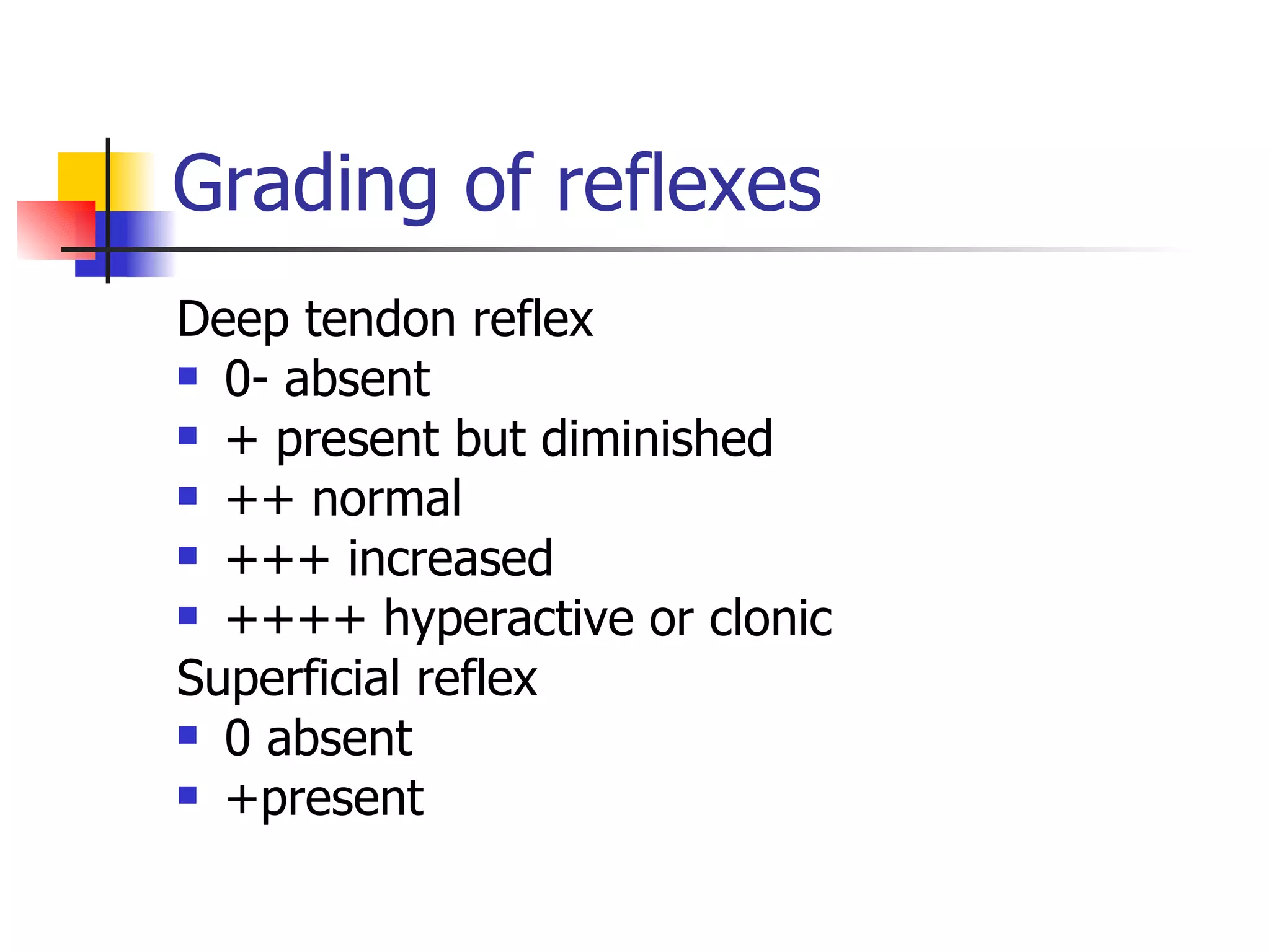
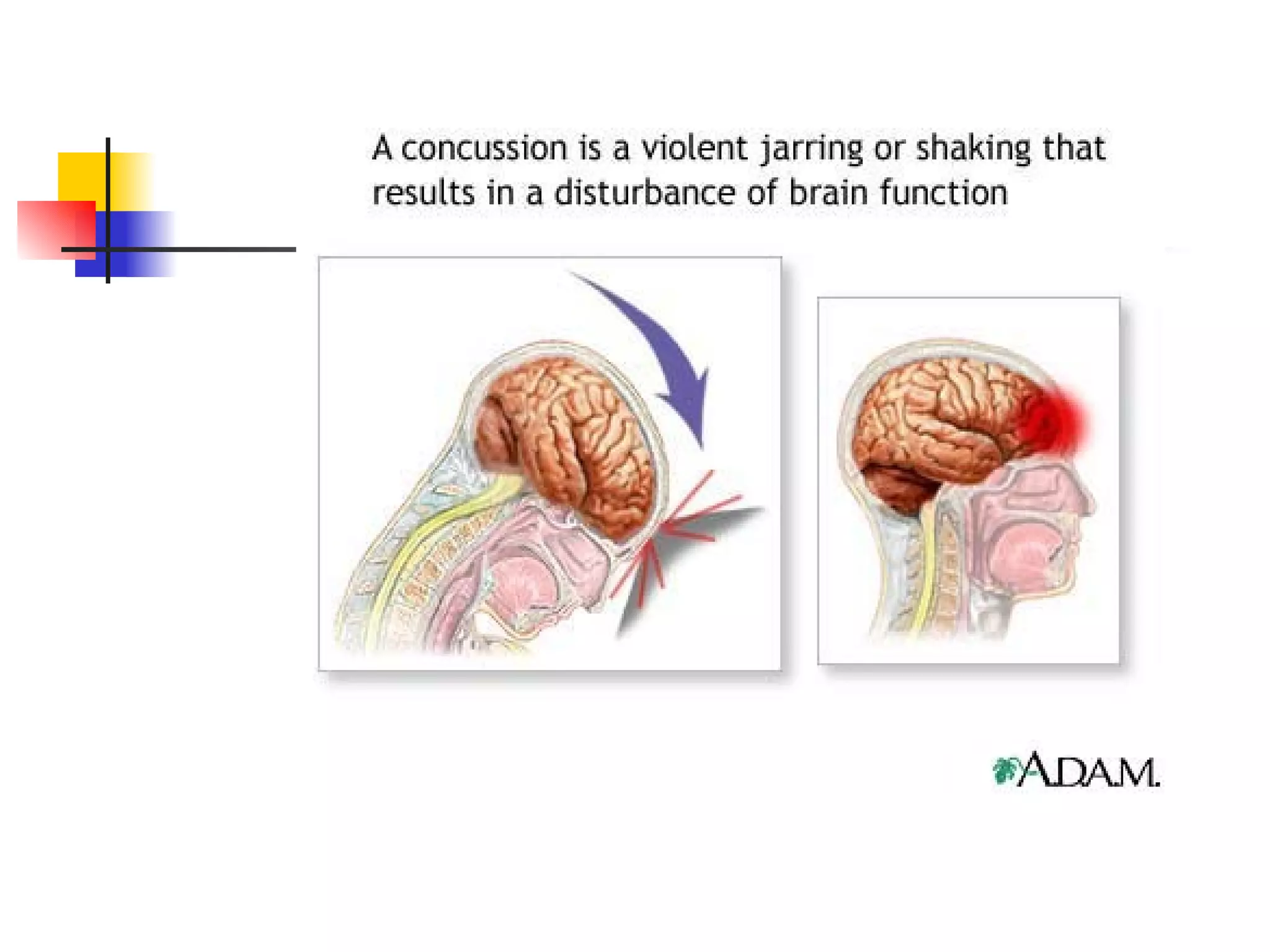
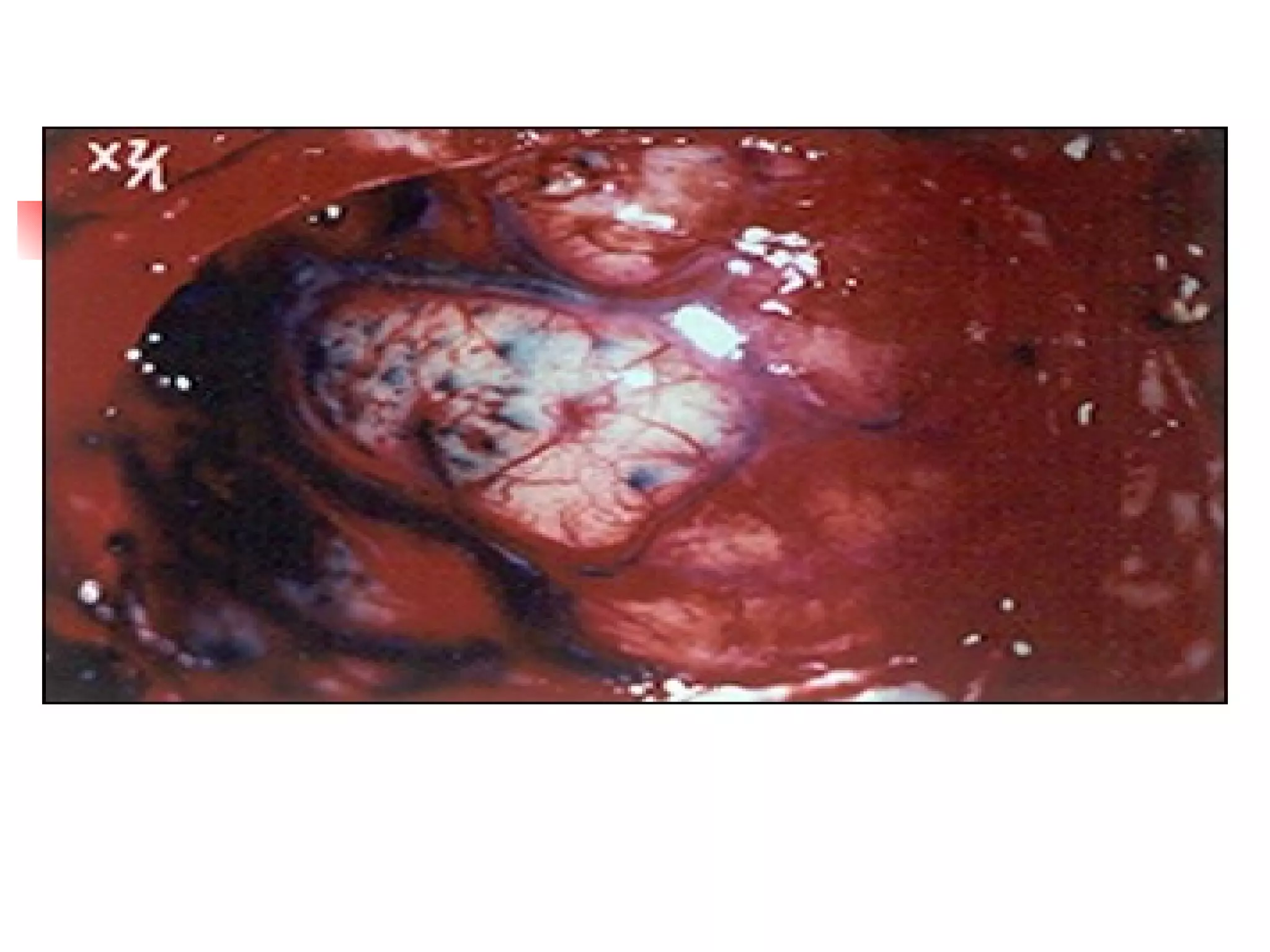
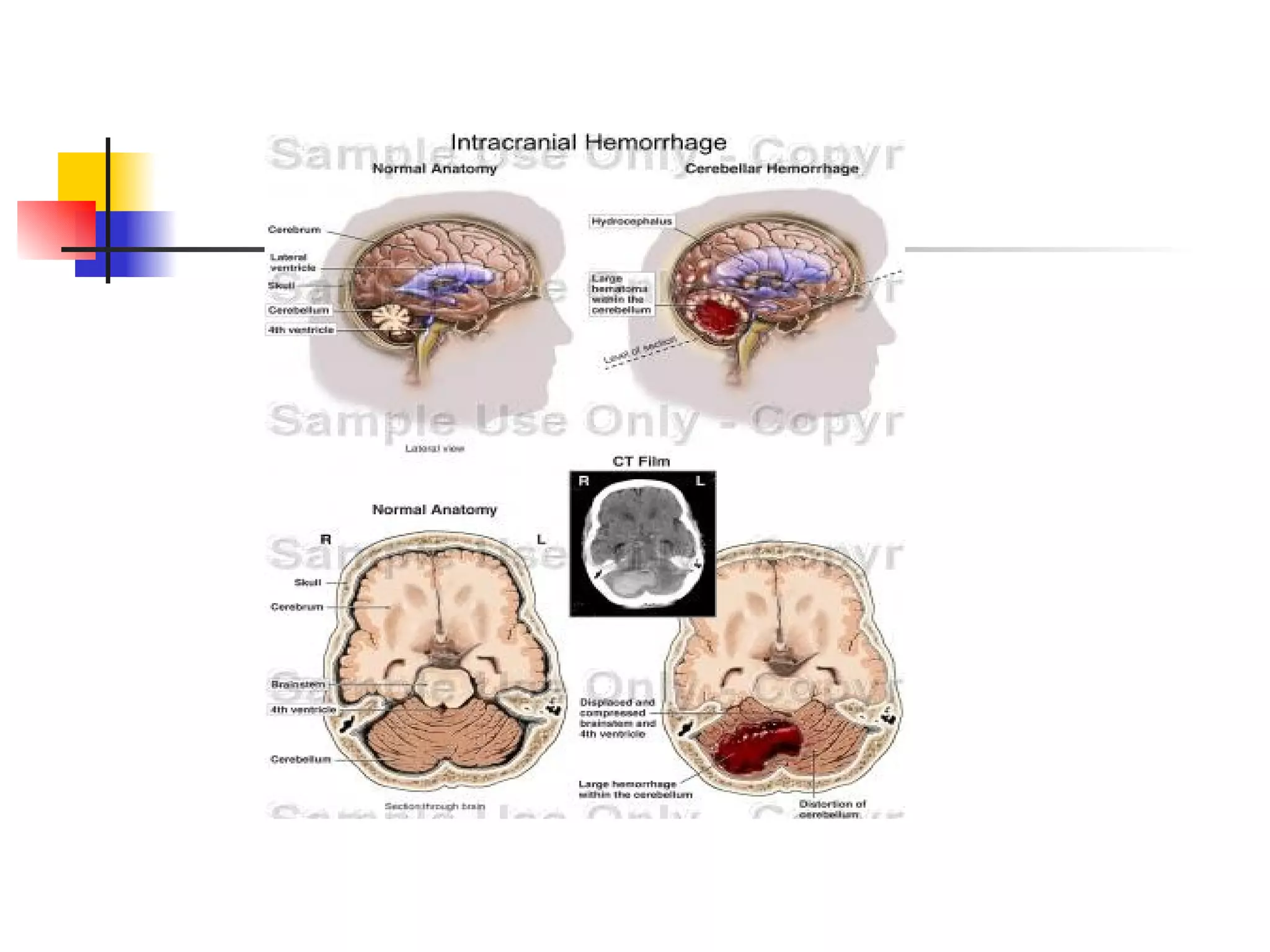
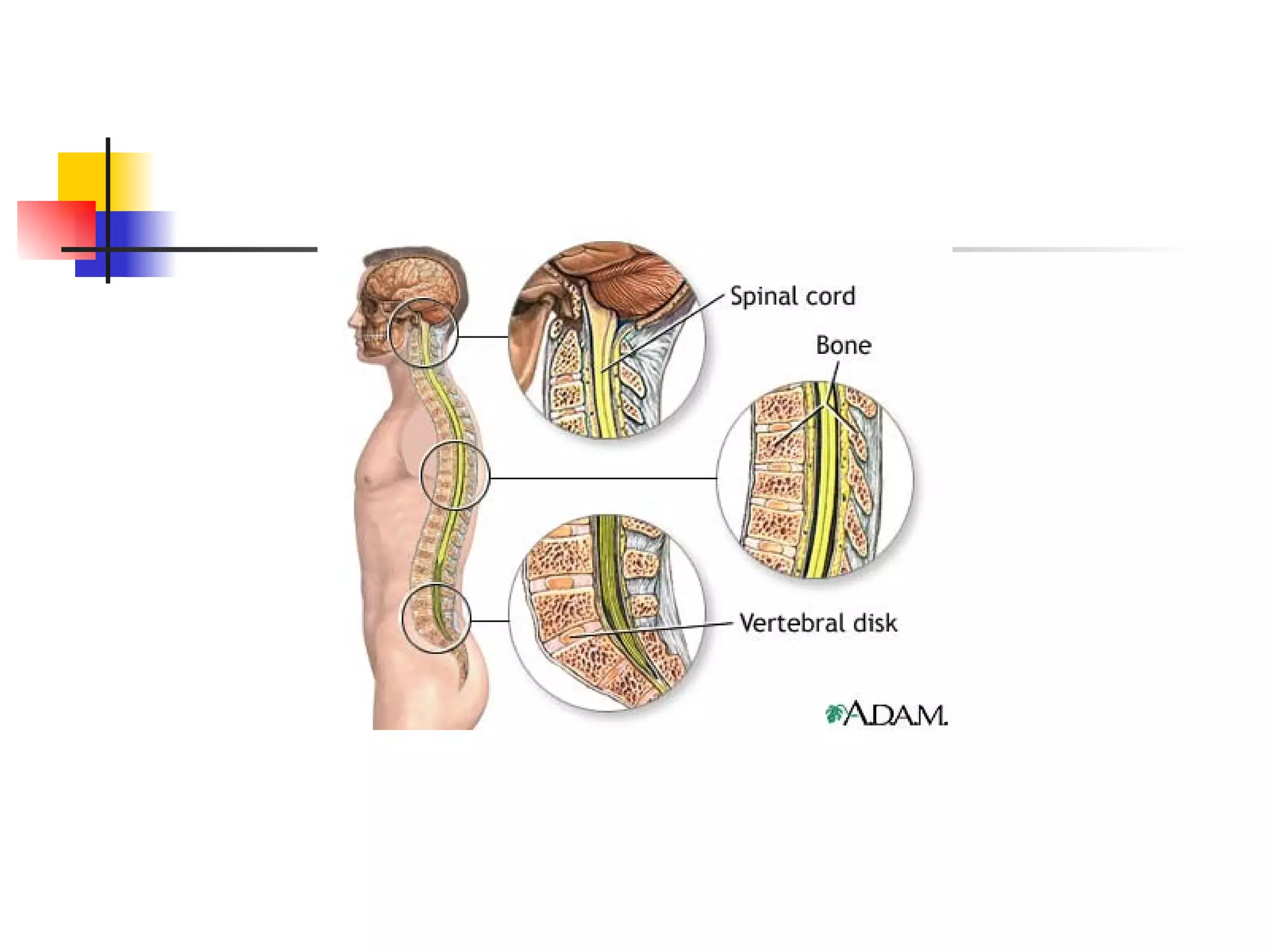
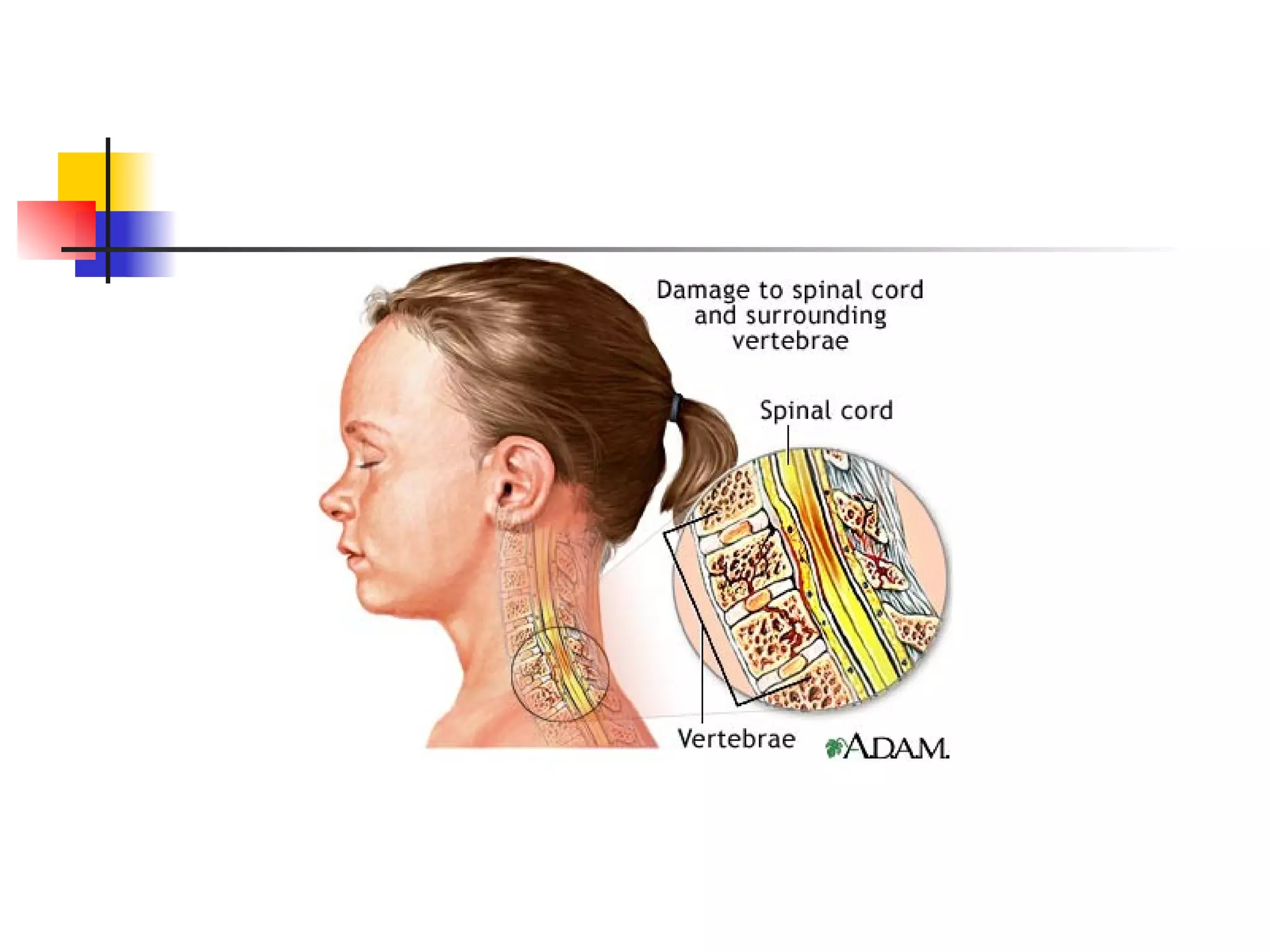
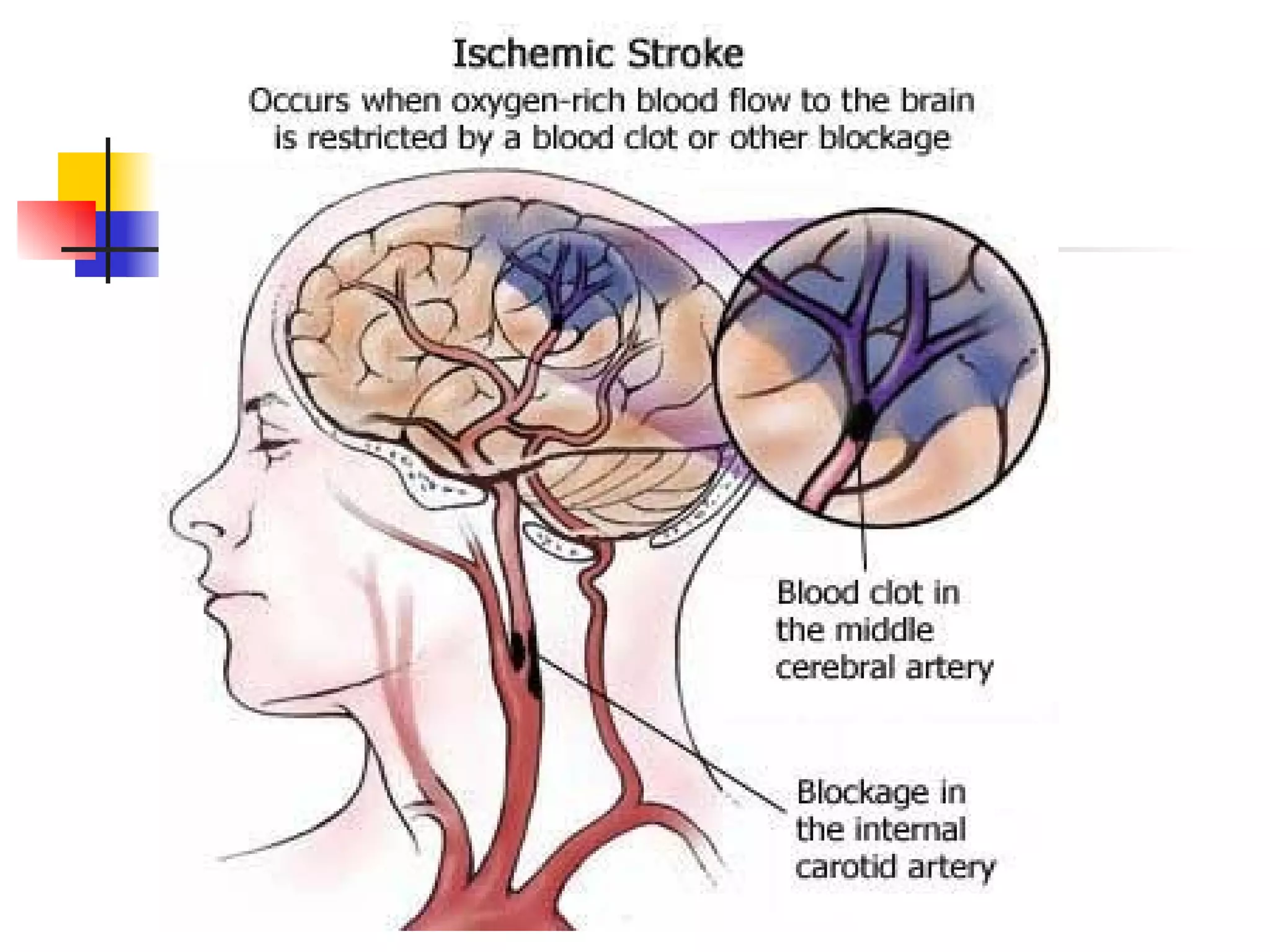
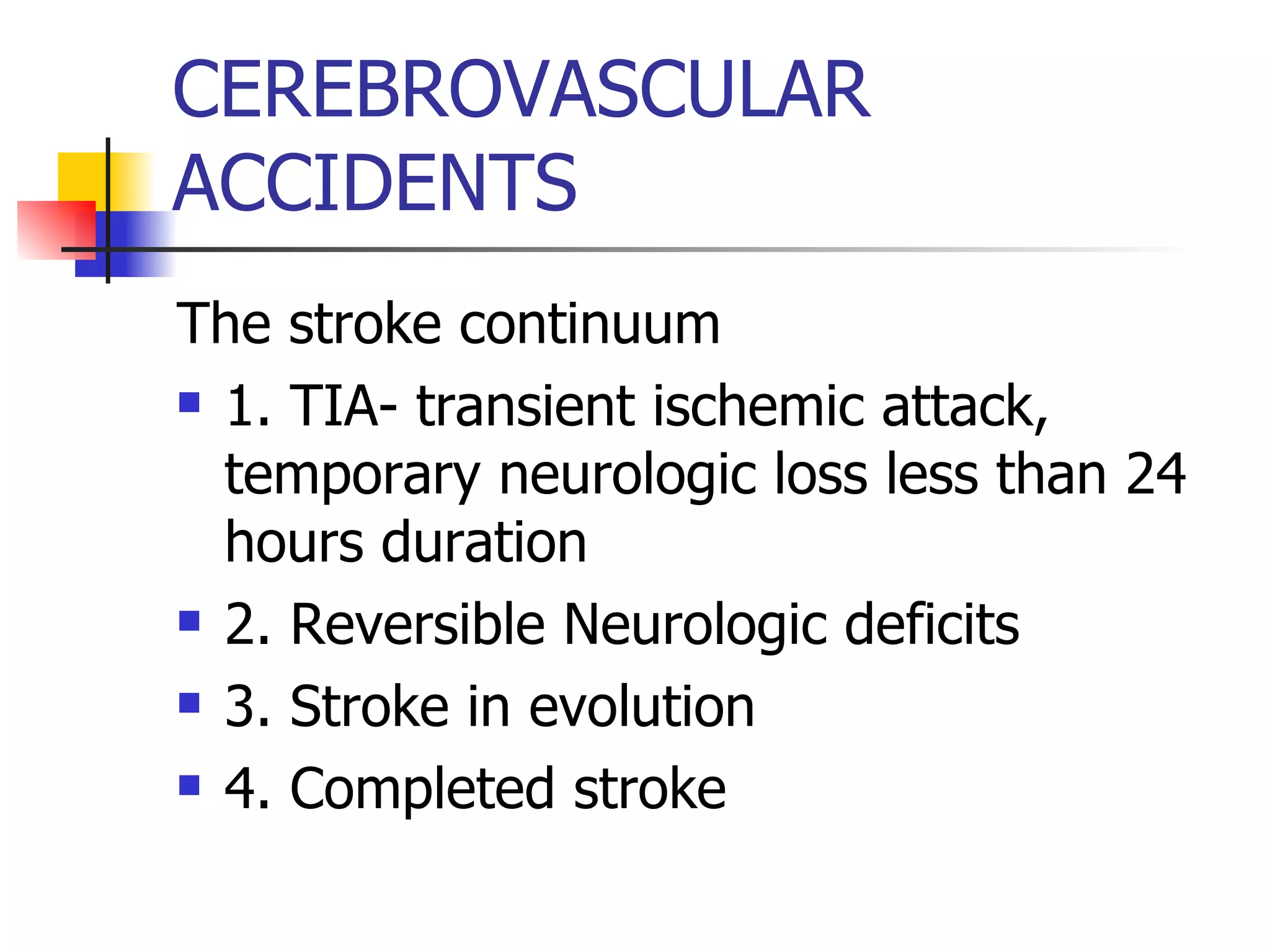
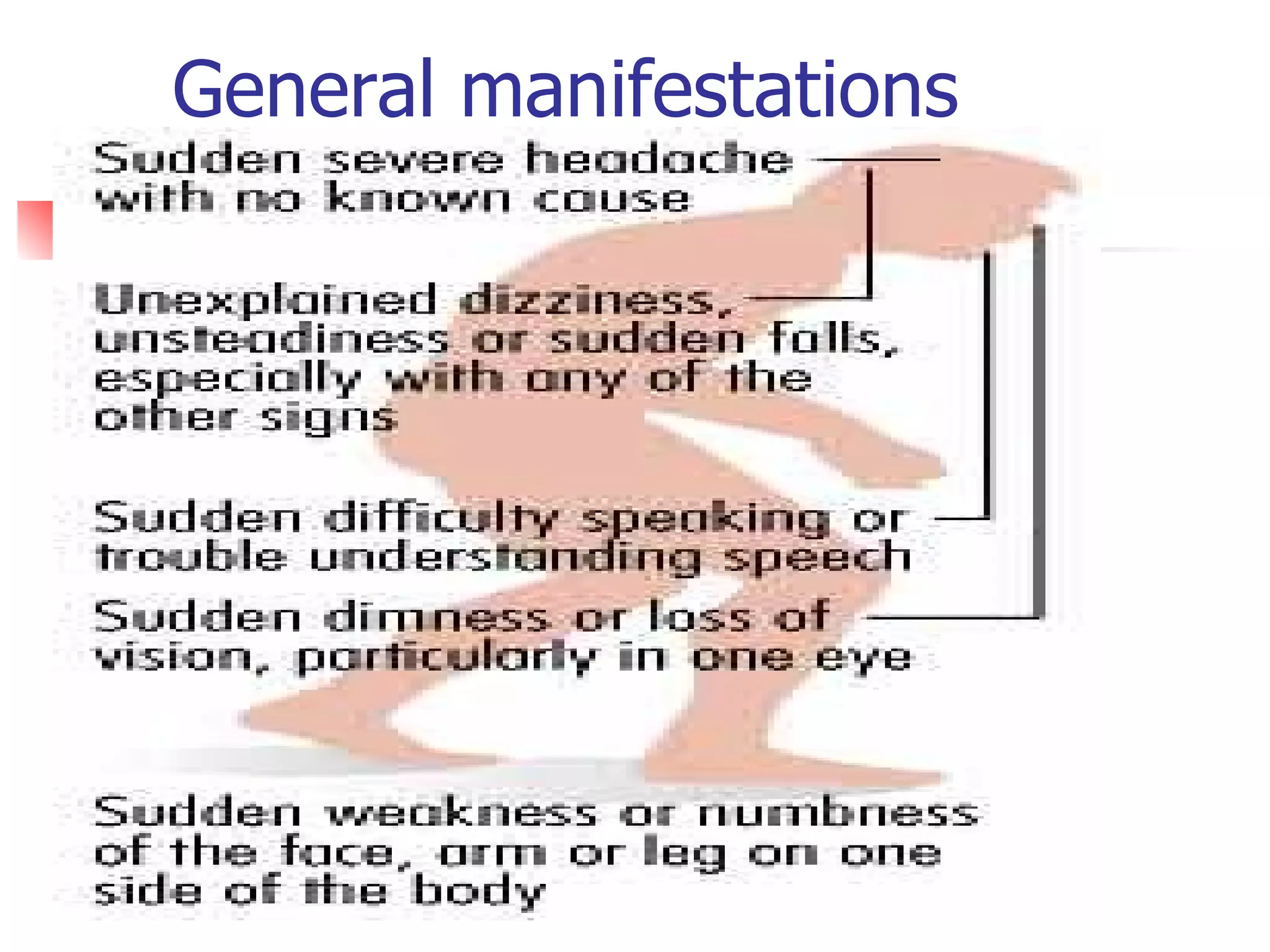
This document provides an outline and overview of key concepts for a review on neurologic nursing concepts for nurse licensure examination. It includes brief summaries of topics like anatomy and physiology of the nervous system, assessment techniques for the neurologic system, common neurologic disorders and conditions, related nursing interventions, and diagnostic tests.