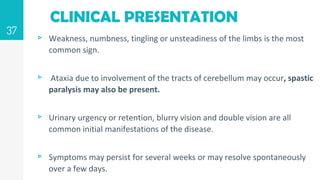
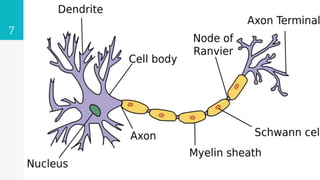
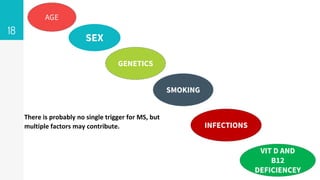
Multiple sclerosis is a chronic disease of the central nervous system characterized by demyelination of nerve fibers. It is an autoimmune disorder where the body's immune system attacks the protective myelin sheath surrounding nerve fibers. Symptoms vary depending on the location of demyelination and include weakness, numbness, vision problems, and difficulties with coordination and balance. There are several types of MS including relapsing-remitting, secondary progressive, primary progressive, and clinically isolated syndrome. The exact cause is unknown but genetic and environmental factors such as infections are thought to play a role in its development.





![IMMUNOPATHOLOGY
▹ The cellular immunology of MS involves altered interactions between
T cells, B cells, myeloid cells, and additional immune cell populations.
▹ Infiltration by inflammatory cells T helper 17-type (Th17)
▹ The risk of developing MS is associated with certain class I and class II
alleles of the major histocompatibility complex loci that are involved
in T cell activation and regulation
▹ Antibodies against one myelin protein (myelin oligodendrocyte
glycoprotein [MOG])
23](https://image.slidesharecdn.com/multiplesclerosisppt-211008150400/85/Multiple-sclerosis-ppt-23-320.jpg)