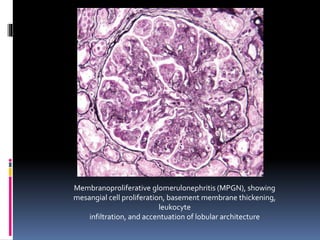
Membranoproliferative glomerulonephritis (MPGN) is characterized by alterations in the glomerular basement membrane and mesangium as well as proliferation of glomerular cells. There are two main types of MPGN, type I and dense deposit disease (formerly type II), which are pathological entities with distinct features. Type I MPGN, which is more common, can be caused by circulating immune complexes or planted antigens, while dense deposit disease appears to be due to excessive complement activation from C3 nephritic factor. Both present variably with hematuria, proteinuria, or nephrotic syndrome and carry poor prognoses, with dense deposit disease being worse.