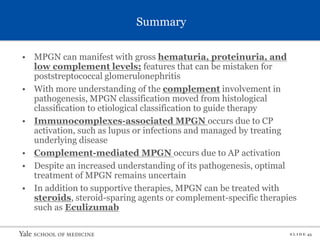
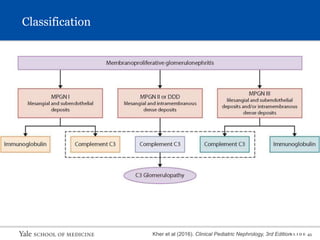
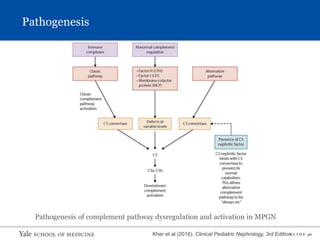
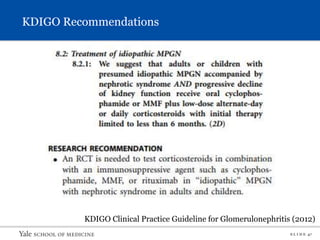
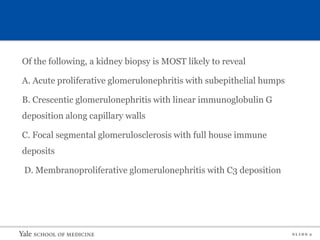
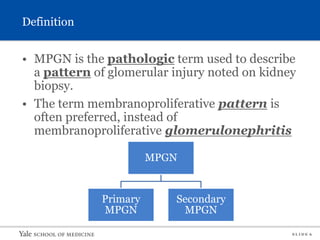
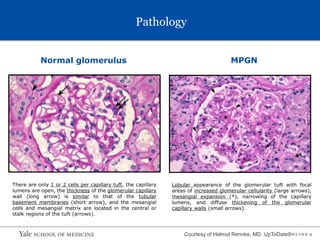
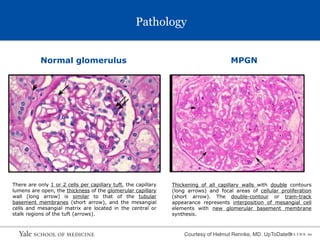
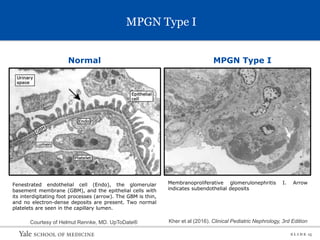
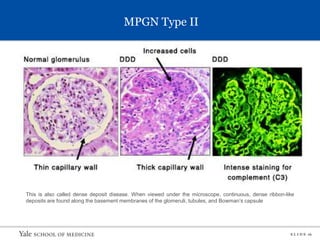
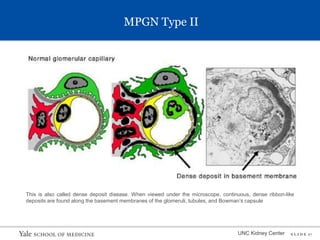
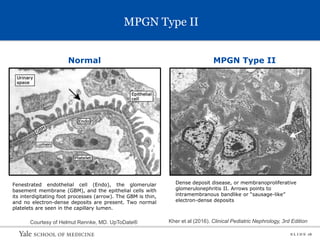
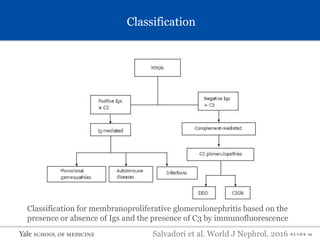
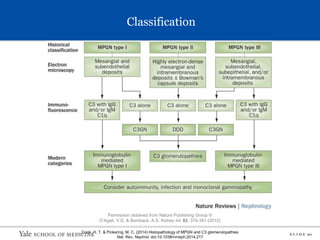
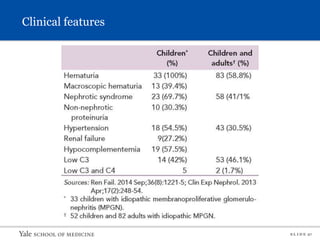
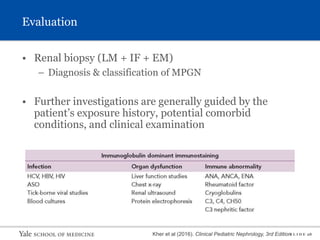
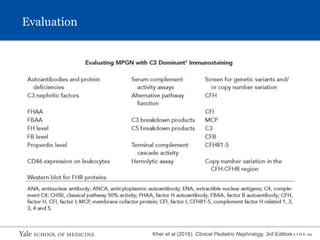
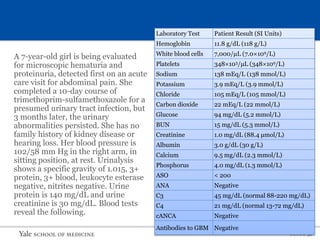
This document describes a case of a 7-year-old girl presenting with microscopic hematuria and proteinuria. Laboratory tests revealed decreased complement C3 levels. Of the pathologies listed, a kidney biopsy would most likely reveal membranoproliferative glomerulonephritis (MPGN) with C3 deposition. The document then provides an overview of MPGN, including its epidemiology, pathology, classification, pathogenesis involving immunocomplex deposition and complement abnormalities, clinical features, evaluation involving renal biopsy and further investigations, and treatment strategies including corticosteroids, immunosuppression, plasma exchange and supportive therapies.
![S L I D E 3
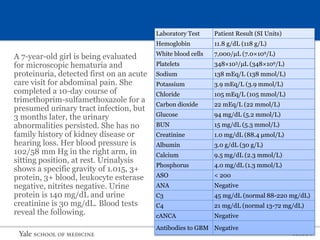
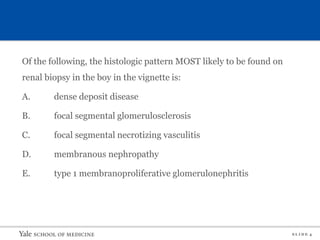
A 10-year-old Vietnamese boy developed gross hematuria 2 hours after
playing basketball. He has no history of upper respiratory or
gastrointestinal infection, joint pain, rash, or trauma. His blood pressure is
140/90 mm Hg; the rest of his physical examination is normal. Urinalysis
shows specific gravity of 1.025; protein, 300 mg/dL; red blood cells
(RBCs), 70/hpf; white blood cells, 7/hpf; and several RBCs and mixed
cellular casts per low-power field. His laboratory findings are as follows:
Serum creatinine, mg/dL (µmol/L) 1.0 (88.4)
Total protein, g/dL (g/L) 5.2 (52)
Albumin, g/dL (g/L) 2.9 (29)
Cholesterol, mg/dL (mmol/L) 190 (4.9)
C3, µg/mL (g/L) 510 (0.51; normal, 900-1,800 [0.91-1.8])
C4, µg/mL (g/L) 15 (0.15; normal, 16-47 [0.16-0.47])
Anti-DNA antibody Negative
Results of serologic tests for hepatitis B s antigen and hepatitis B e antigen
are positive.](https://image.slidesharecdn.com/mpgn-220825171713-e8fcb1fb/85/MPGN-pptx-4-320.jpg)
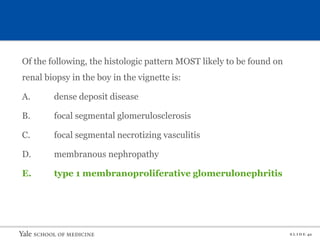
![S L I D E 41
A 10-year-old Vietnamese boy developed gross hematuria 2 hours after
playing basketball. He has no history of upper respiratory or
gastrointestinal infection, joint pain, rash, or trauma. His blood pressure is
140/90 mm Hg; the rest of his physical examination is normal. Urinalysis
shows specific gravity of 1.025; protein, 300 mg/dL; red blood cells
(RBCs), 70/hpf; white blood cells, 7/hpf; and several RBCs and mixed
cellular casts per low-power field. His laboratory findings are as follows:
Serum creatinine, mg/dL (µmol/L) 1.0 (88.4)
Total protein, g/dL (g/L) 5.2 (52)
Albumin, g/dL (g/L) 2.9 (29)
Cholesterol, mg/dL (mmol/L) 190 (4.9)
C3, µg/mL (g/L) 510 (0.51; normal, 900-1,800 [0.91-1.8])
C4, µg/mL (g/L) 15 (0.15; normal, 16-47 [0.16-0.47])
Anti-DNA antibody Negative
Results of serologic tests for hepatitis B s antigen and hepatitis B e antigen
are positive.](https://image.slidesharecdn.com/mpgn-220825171713-e8fcb1fb/85/MPGN-pptx-42-320.jpg)