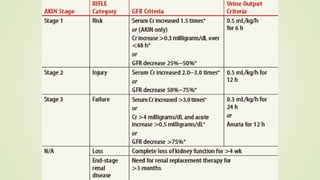
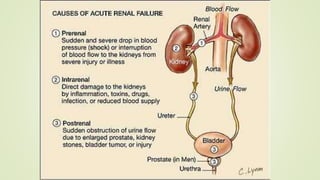
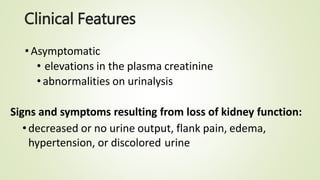
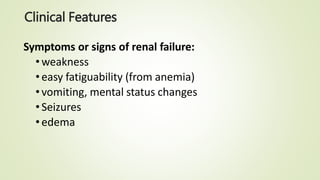
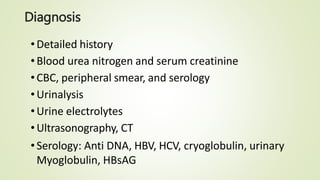
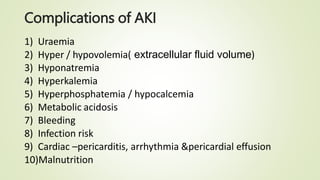
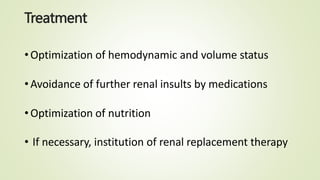
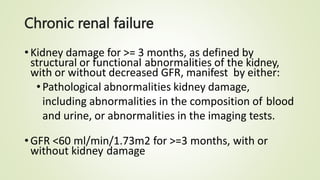
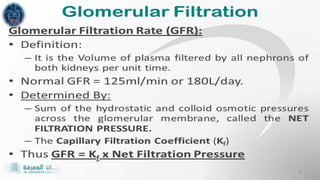
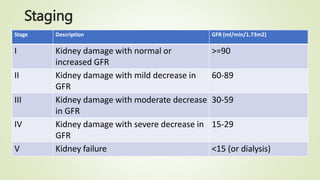
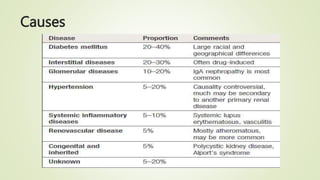
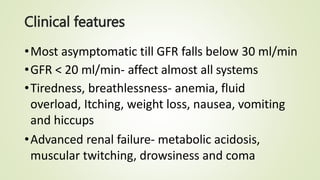
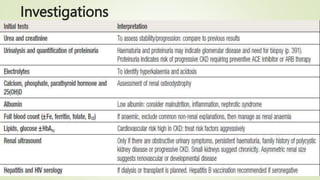
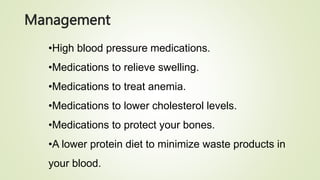
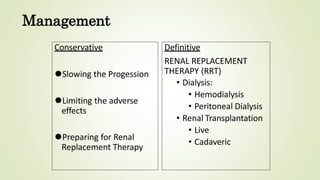
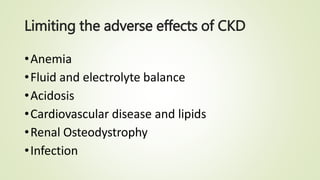
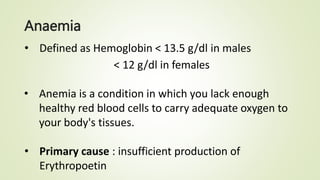
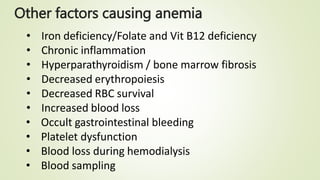
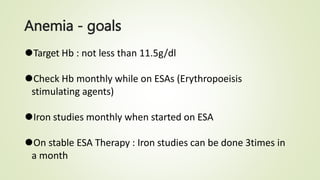
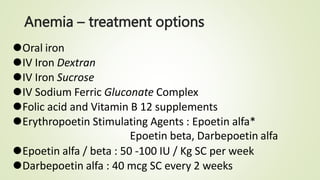
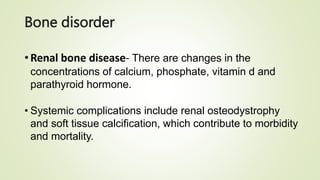
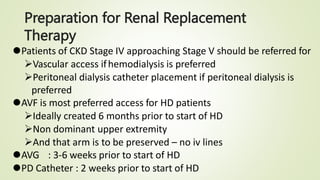
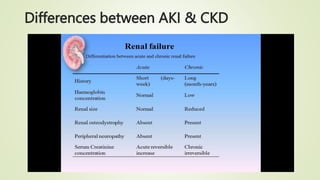
The document discusses renal failure, including acute renal failure (ARF) and chronic renal failure (CRF). It defines renal failure as when the kidneys cannot remove metabolic waste or perform regulatory functions. ARF is a reversible clinical syndrome with sudden loss of kidney function over hours to days. CRF is kidney damage for 3+ months with decreased GFR. CRF management focuses on slowing progression, limiting complications like anemia and bone disease, and preparing for renal replacement therapies like dialysis and transplantation.