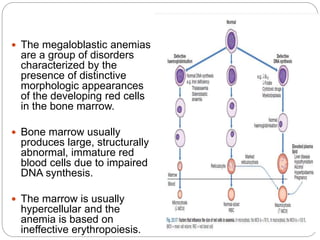
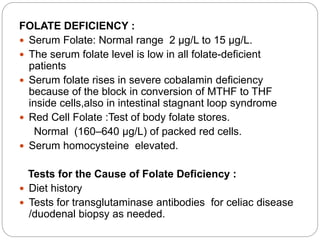
This document provides an overview of macrocytic anemia, focusing on deficiencies in cobalamin and folate. It describes the etiology, absorption, clinical features, hematologic findings, diagnosis, and other causes of macrocytic anemia. Cobalamin and folate deficiencies can result in megaloblastic changes in the bone marrow and ineffective hematopoiesis. Diagnosis involves measuring serum levels of cobalamin, folate, methylmalonic acid and homocysteine, along with tests to determine the underlying cause of deficiency. Other potential causes of macrocytic anemia include vitamin B6 deficiency, acute infections, drugs, toxins, acute myeloid leukemia, and genetic disorders.