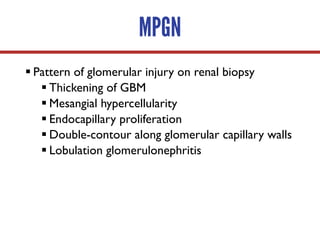
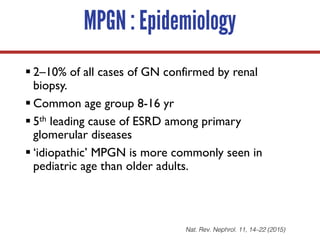
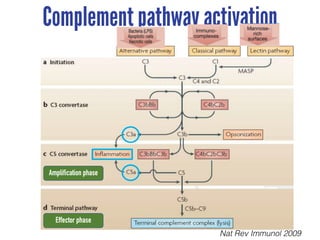
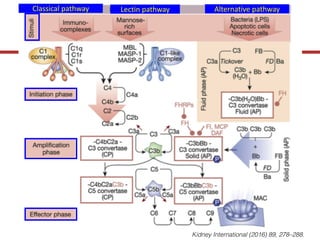
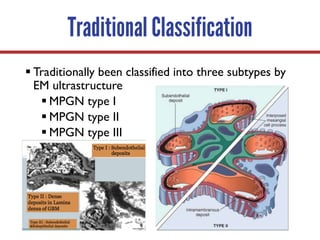
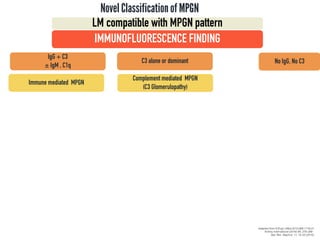
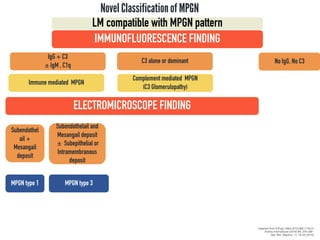
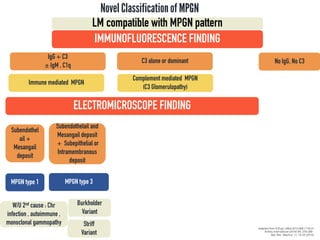
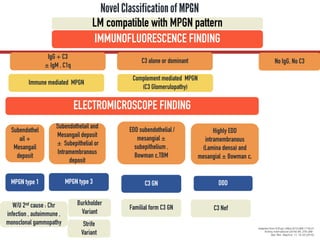
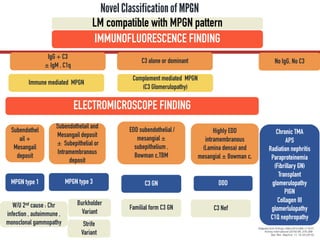
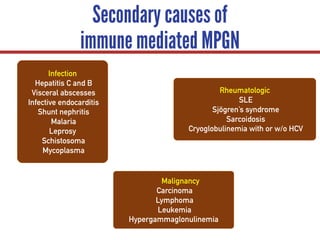
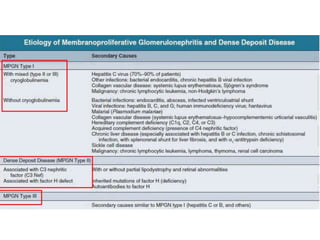
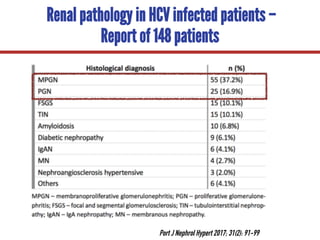
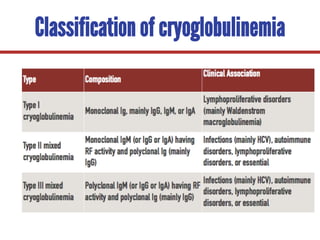
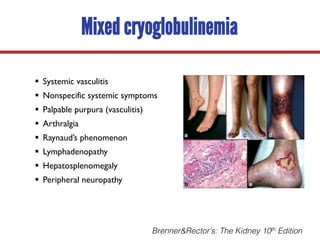
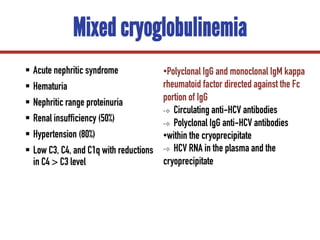
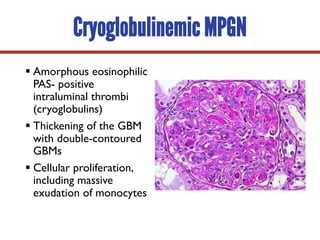
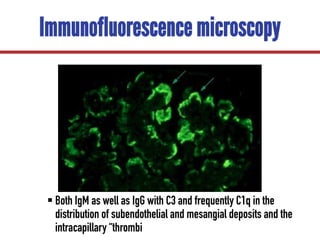
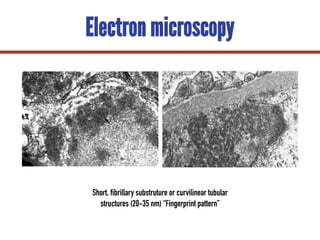
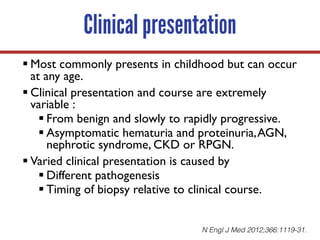
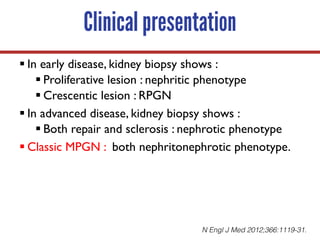
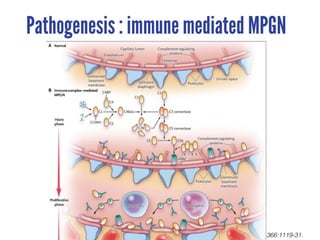
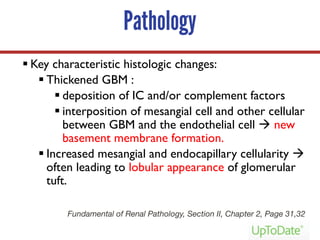
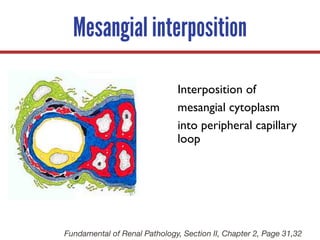
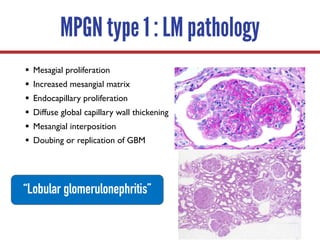
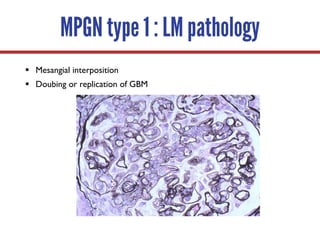
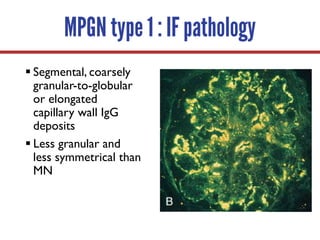
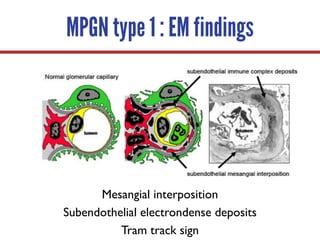
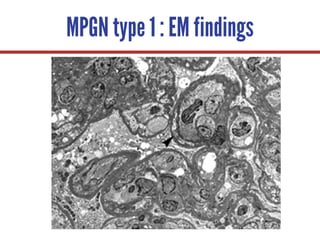
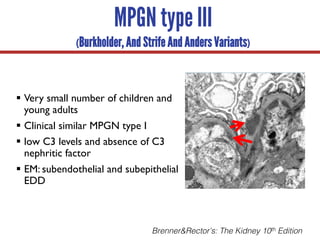
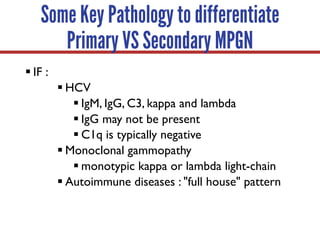
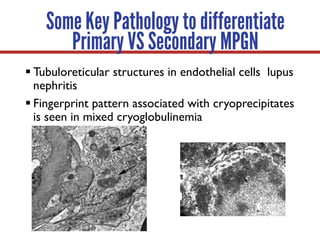
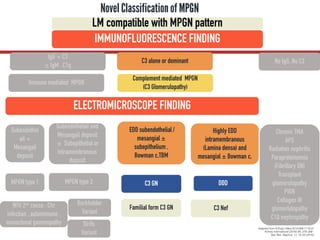
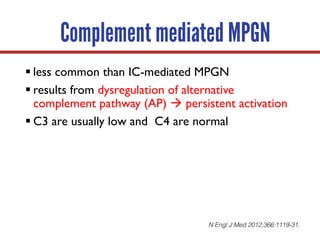
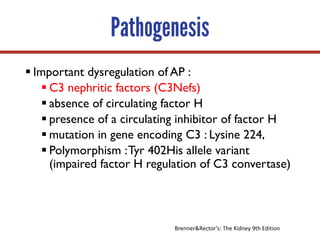
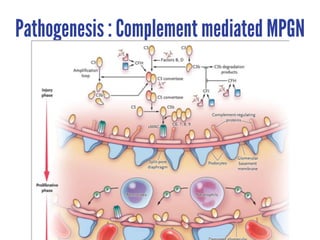
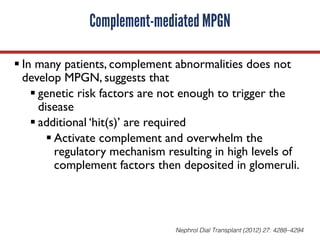
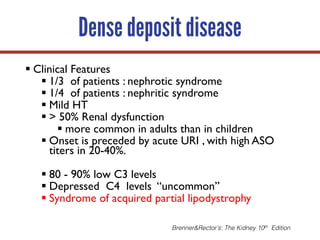
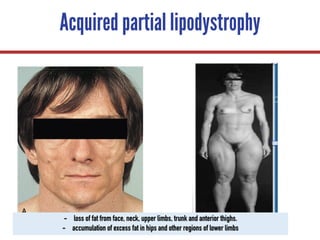
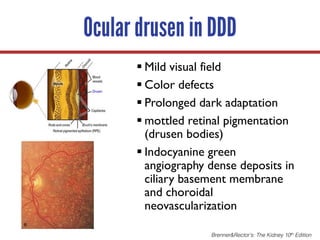
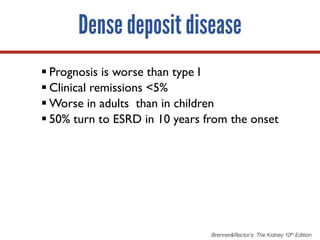
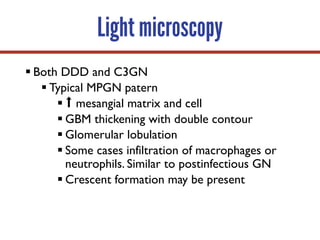
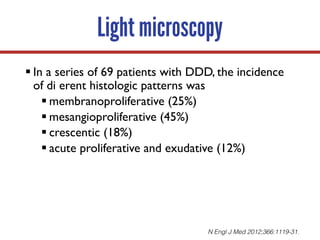
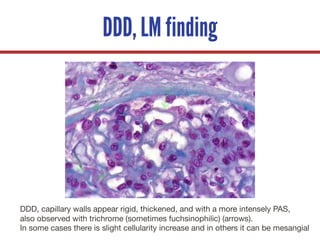
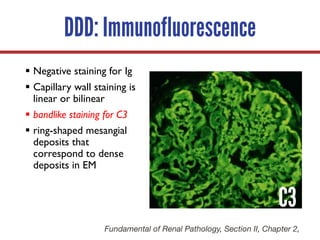
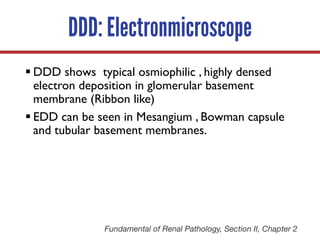
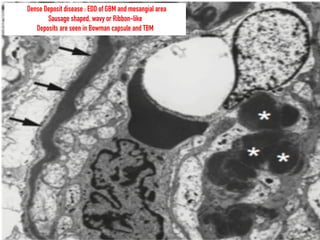
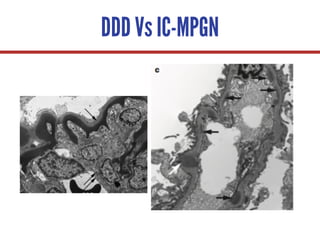
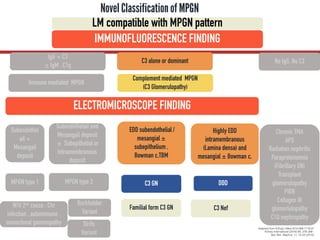
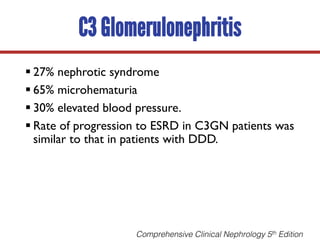
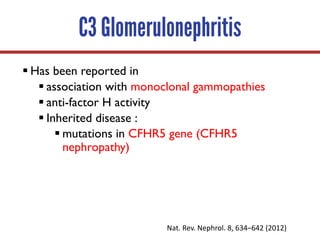
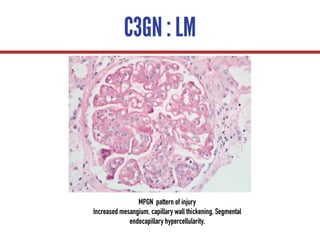
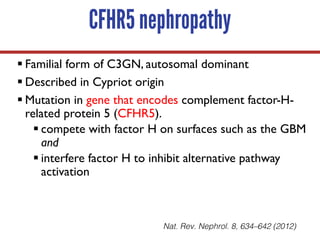
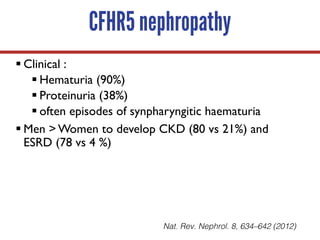
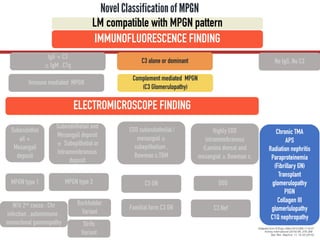
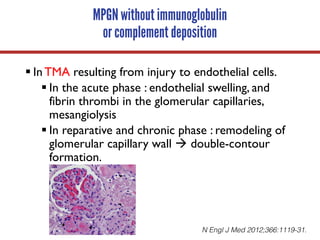
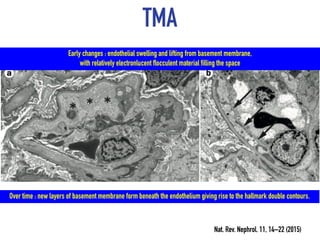
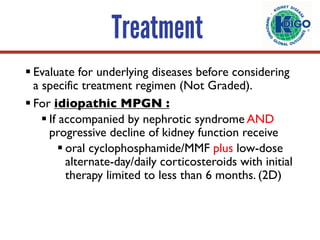
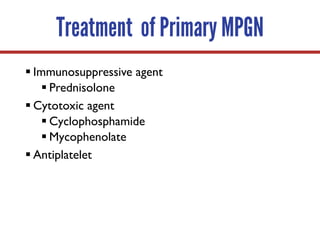
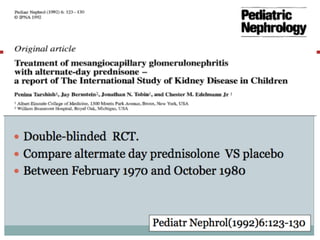
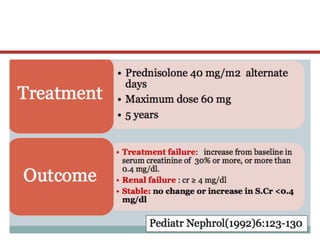
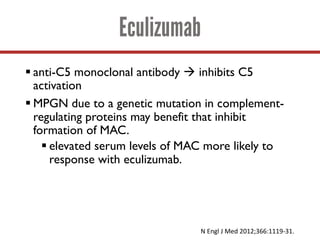
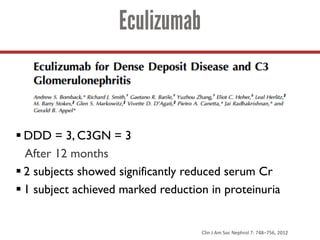
This document provides information on membranoproliferative glomerulonephritis (MPGN), including its classification, pathogenesis, clinical presentation, pathology, and treatment. MPGN is classified based on immunofluorescence and electron microscopy findings. It can be immune-mediated via immune complex deposition or complement-mediated via dysregulation of the alternative complement pathway. On pathology, it is characterized by thickened glomerular basement membranes, mesangial hypercellularity, and endocapillary proliferation. Clinical presentation varies from asymptomatic to nephrotic syndrome or renal failure.