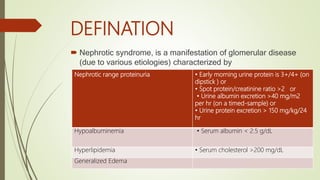
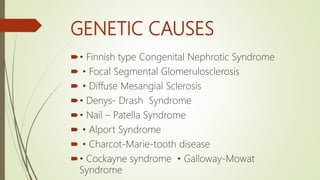
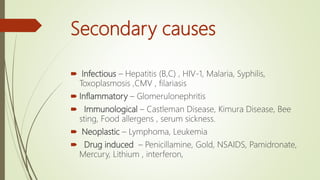
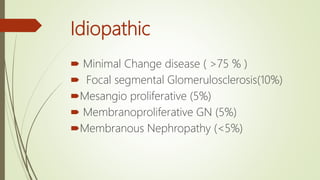
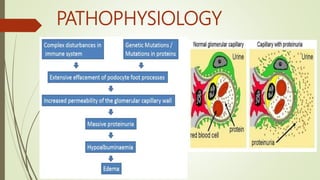
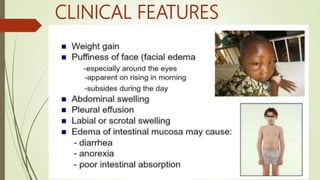
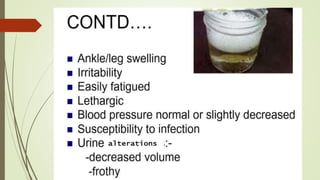
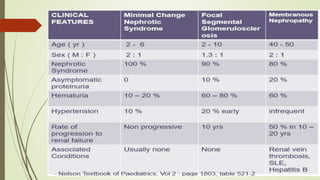
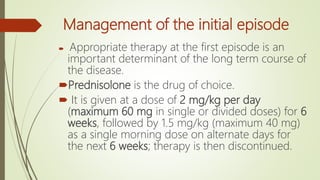
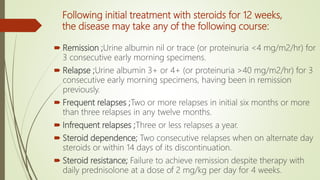
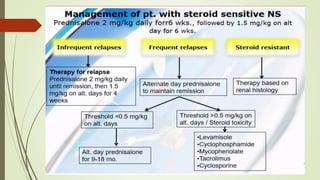
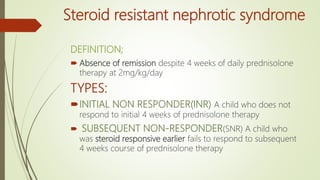
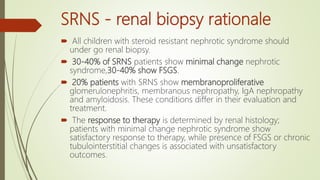
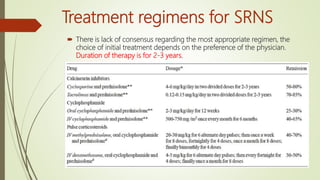
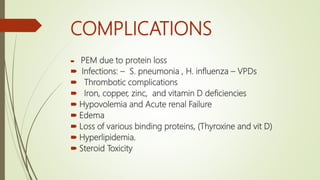
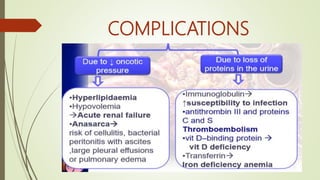
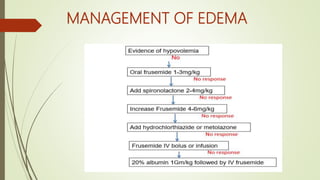
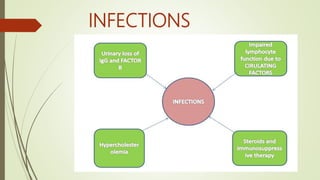
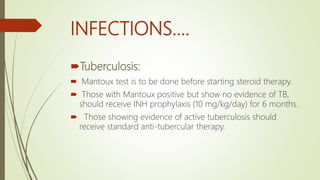
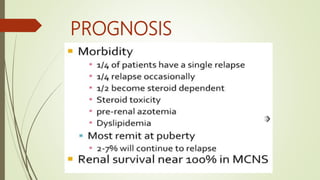
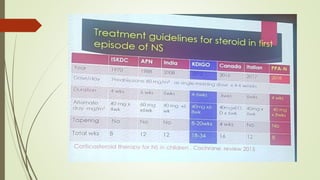
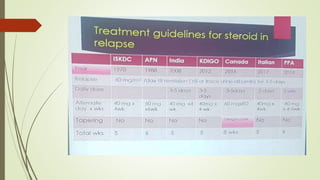
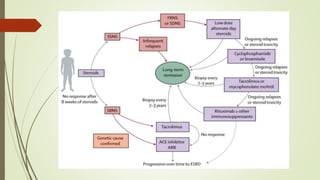
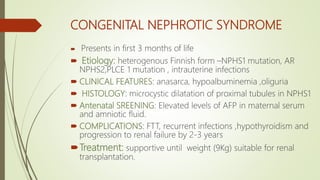
Nephrotic syndrome is characterized by nephrotic range proteinuria, hypoalbuminemia, hyperlipidemia, and edema. It is mostly caused by primary glomerular abnormalities. The majority of cases are idiopathic minimal change disease. Steroids are the first line treatment and frequent relapses are managed with immunosuppressants. Complications include infections, thromboembolism, and steroid toxicity. Prognosis is generally good but depends on underlying pathology and response to treatment. Congenital nephrotic syndrome presents in infants and has a heterogeneous genetic cause.