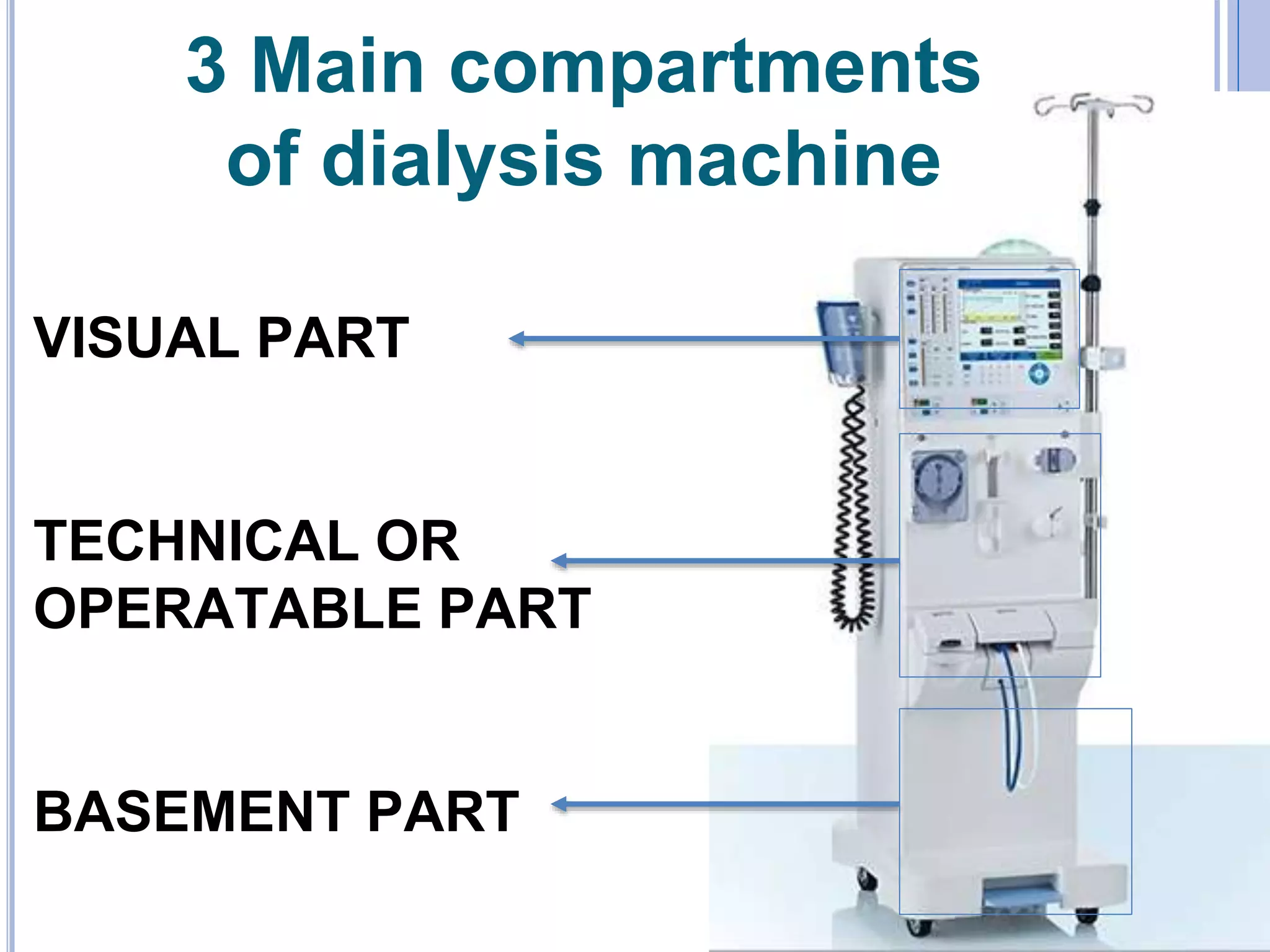
The document describes the key components and functions of a dialysis machine. It discusses the three main compartments, features like the blood pump and dialysate delivery system, safety monitors including pressure monitors, and options like bicarbonate and variable sodium. It provides details on how each component works, such as how the blood pump circulates blood and how safety monitors detect issues like high pressure or air bubbles. The document also covers system disinfection and how to respond to common alarm situations during dialysis treatment.