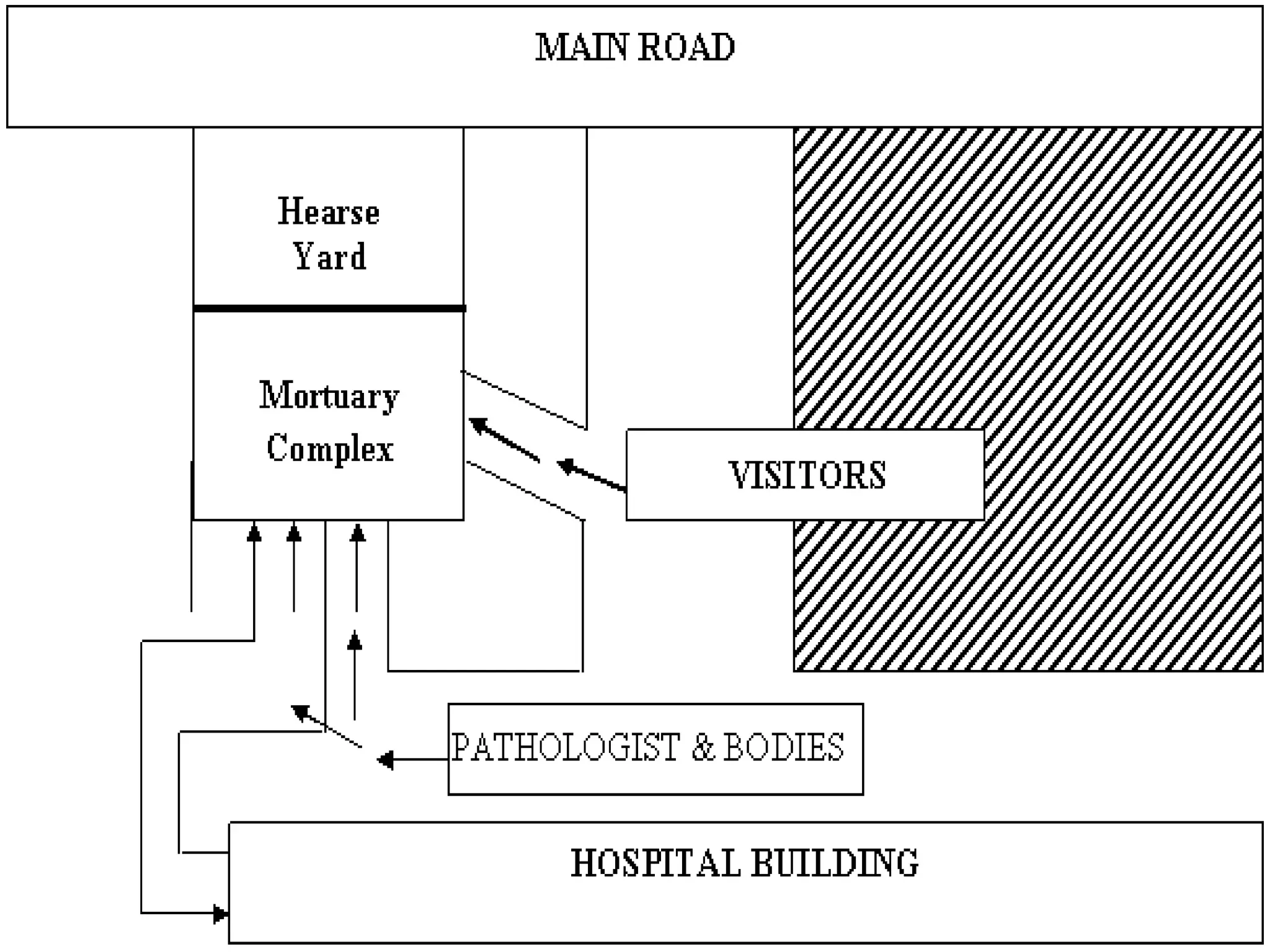
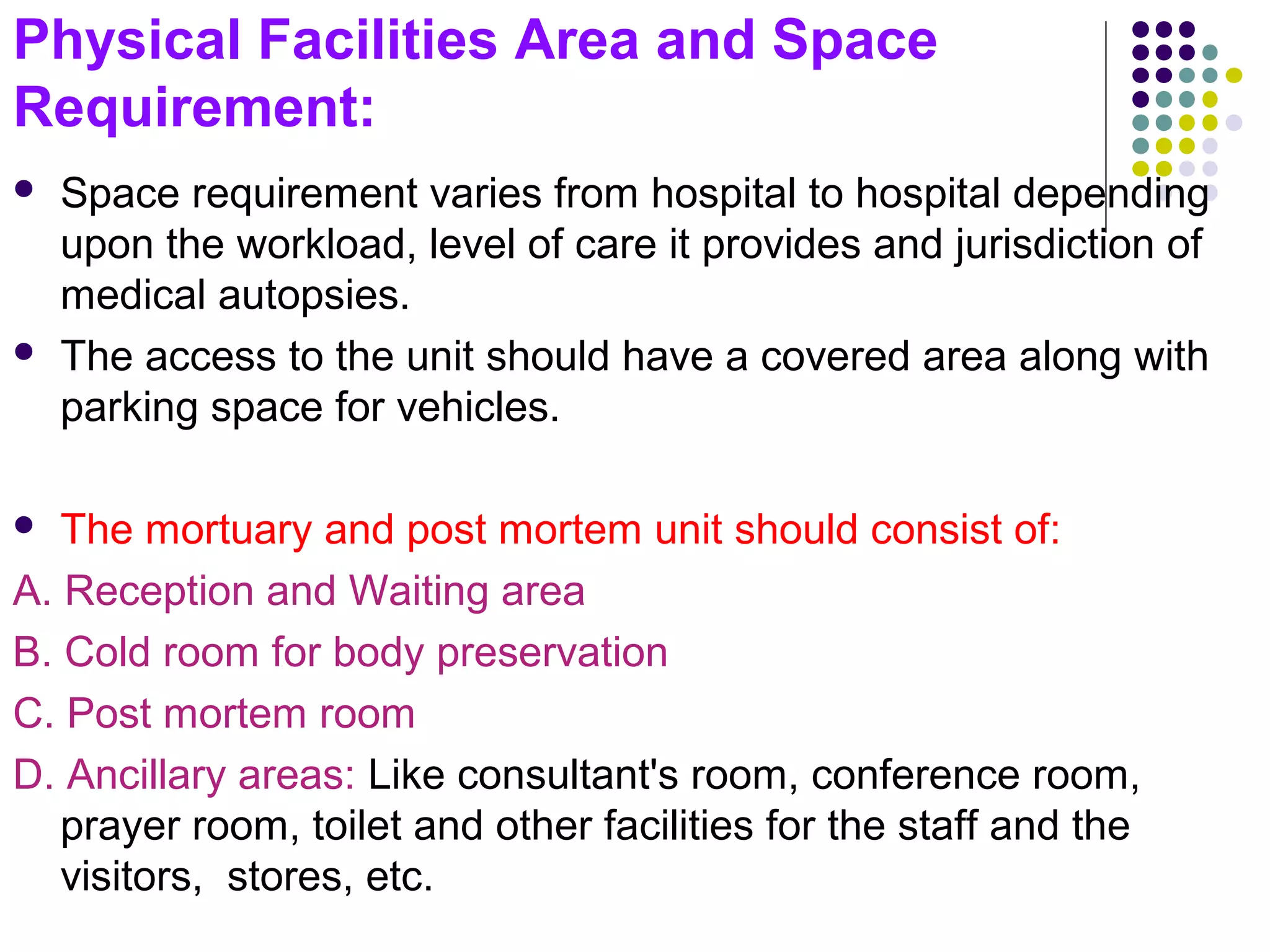
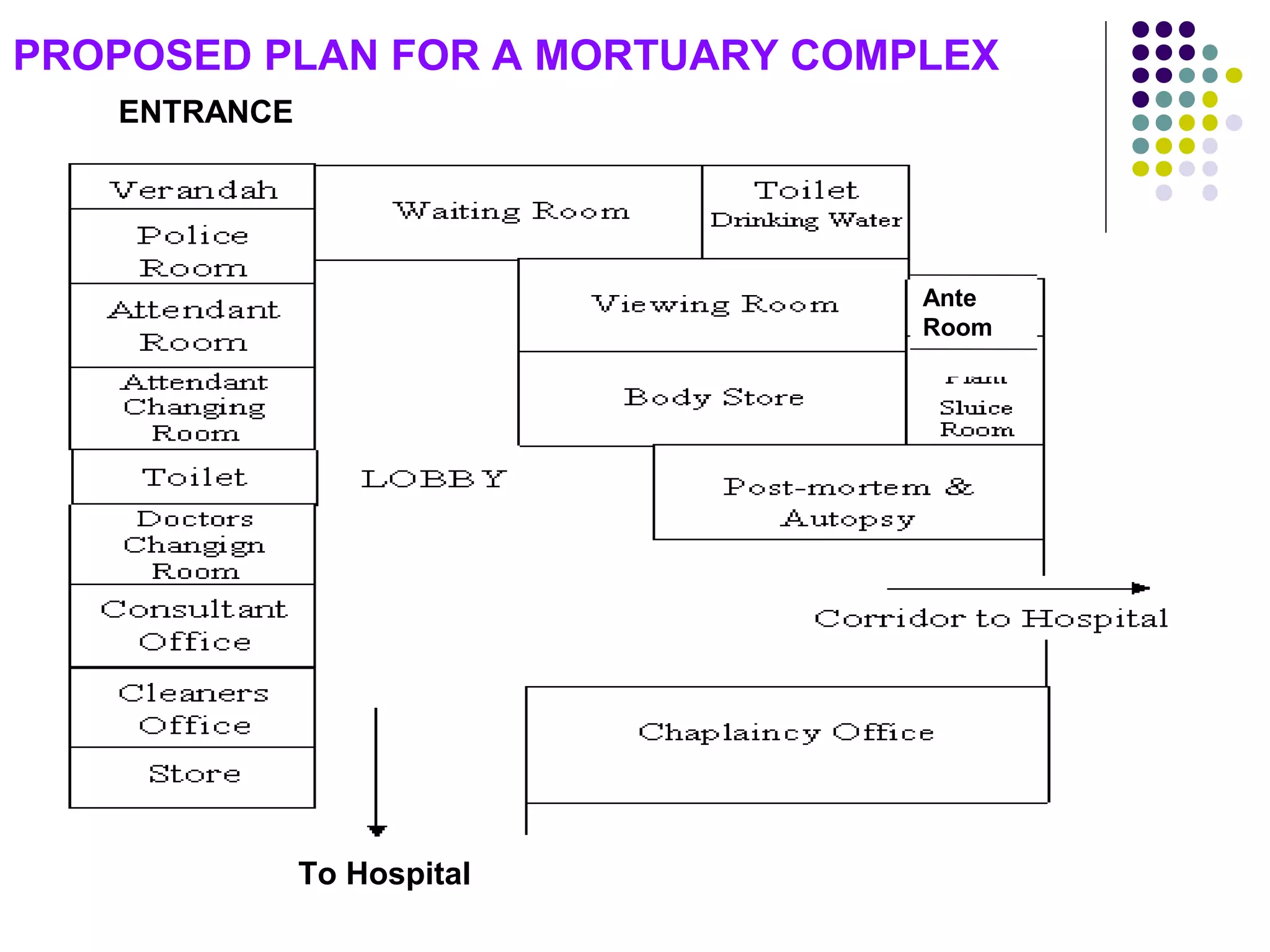
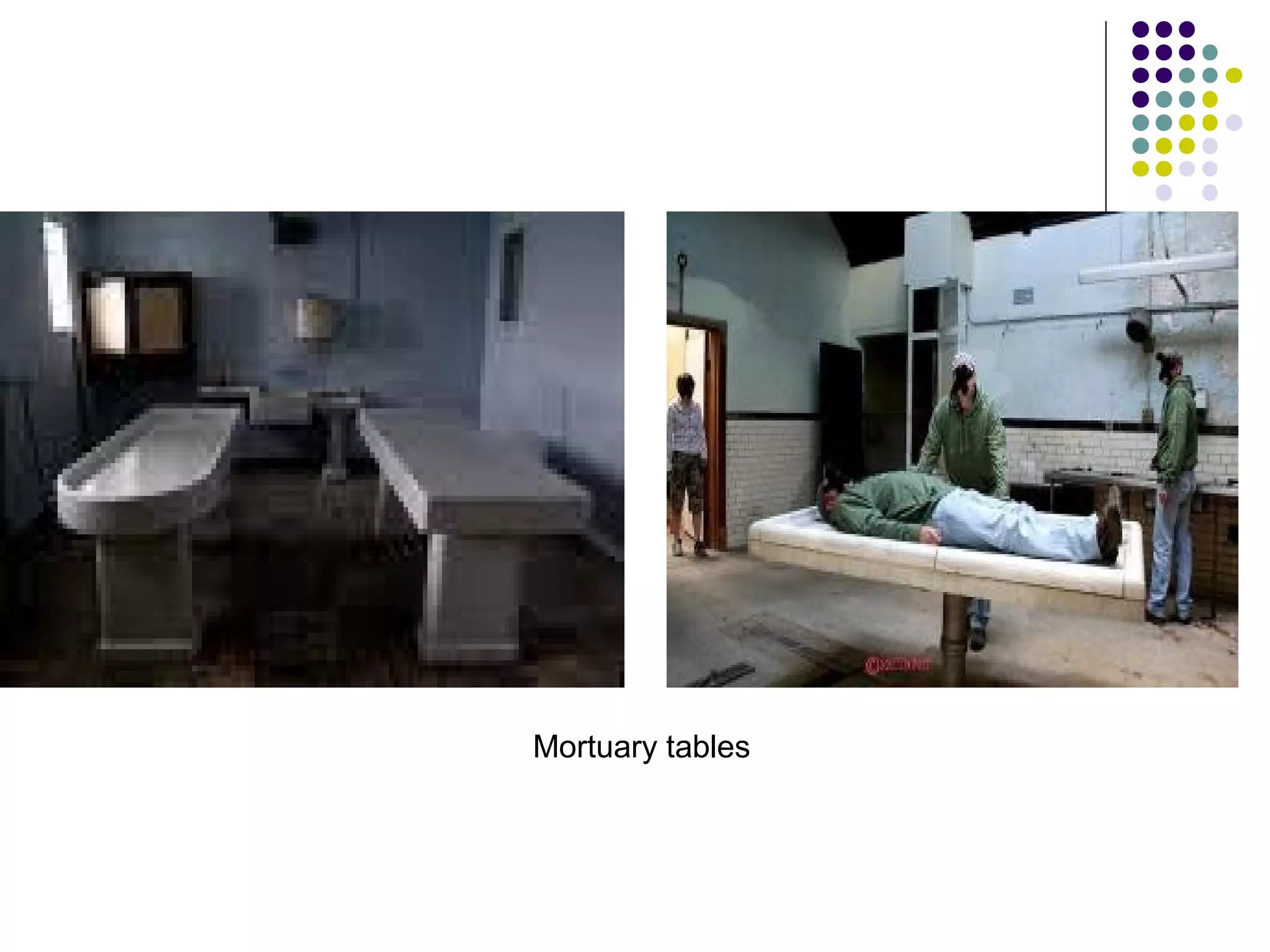
The document discusses the requirements and setup for a modern mortuary facility, including staffing, physical space, equipment, and upgrades needed for handling highly infectious diseases. Key points include guidelines from the Medical Council of India on minimum staffing levels based on annual autopsy numbers. Physical space should include a reception area, cold storage room, post-mortem room, and ancillary spaces like a doctor's office. Equipment needs include scales, cutting instruments, forceps, saws, and supplies for cleaning/preserving specimens. Proper ventilation, lighting, and safety features are also outlined.