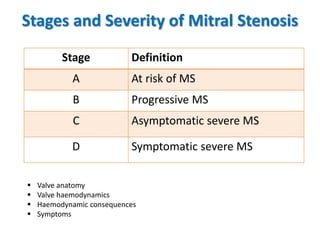
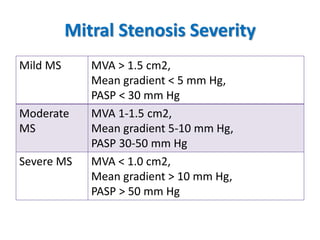
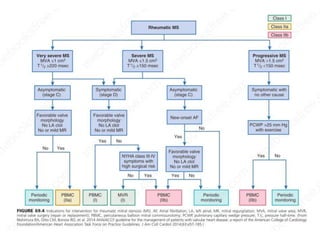
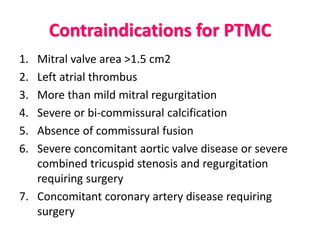
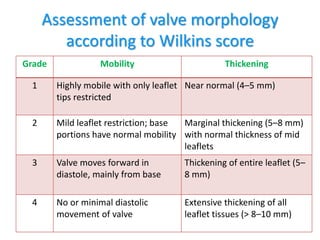
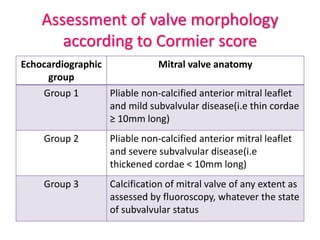
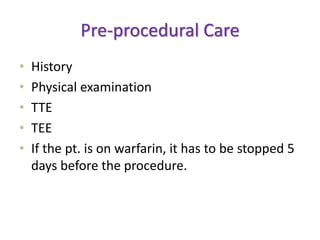
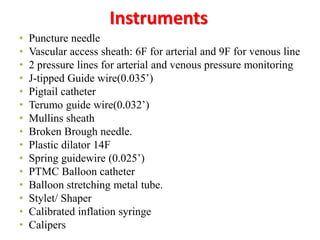
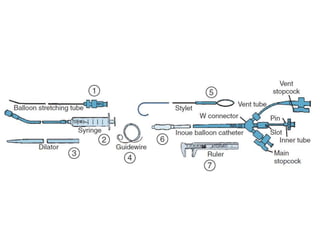
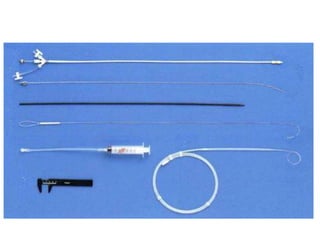
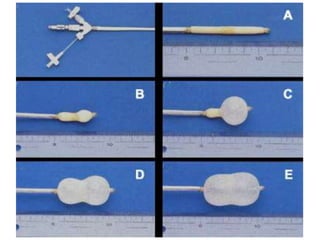
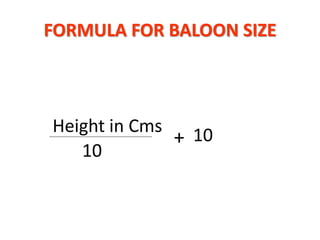
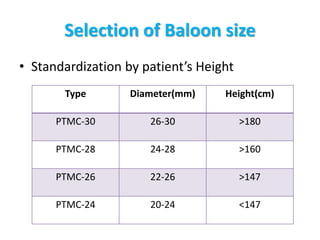
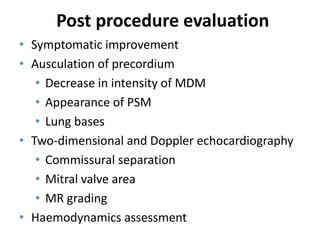
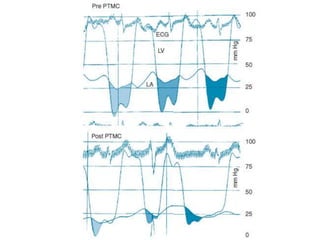
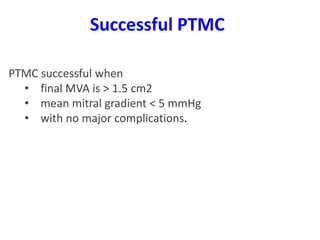
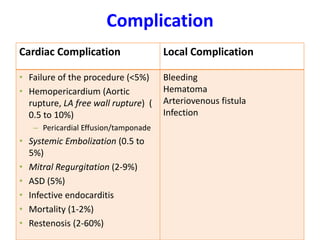
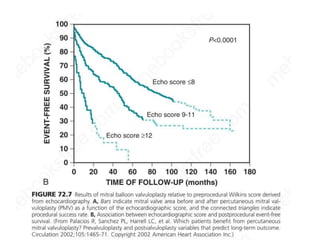
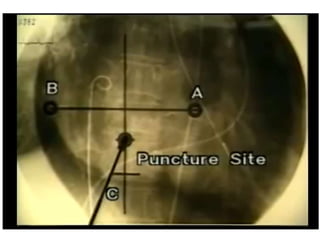
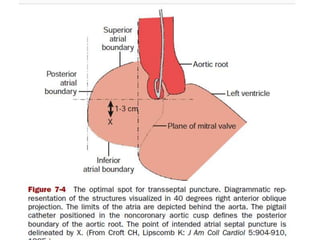
This document provides information about percutaneous transvenous mitral commissurotomy (PTMC), a procedure used to treat mitral stenosis. It discusses the stages and severity of mitral stenosis, indications and contraindications for PTMC, assessment of valve morphology, the PTMC procedure technique, instruments used, balloon size selection, post-procedure evaluation, complications, follow-up care, and long-term prognosis. PTMC is performed to improve the opening of a stenosed mitral valve by splitting the fused commissures using a balloon catheter, and is an important therapeutic option for treating symptomatic mitral stenosis.