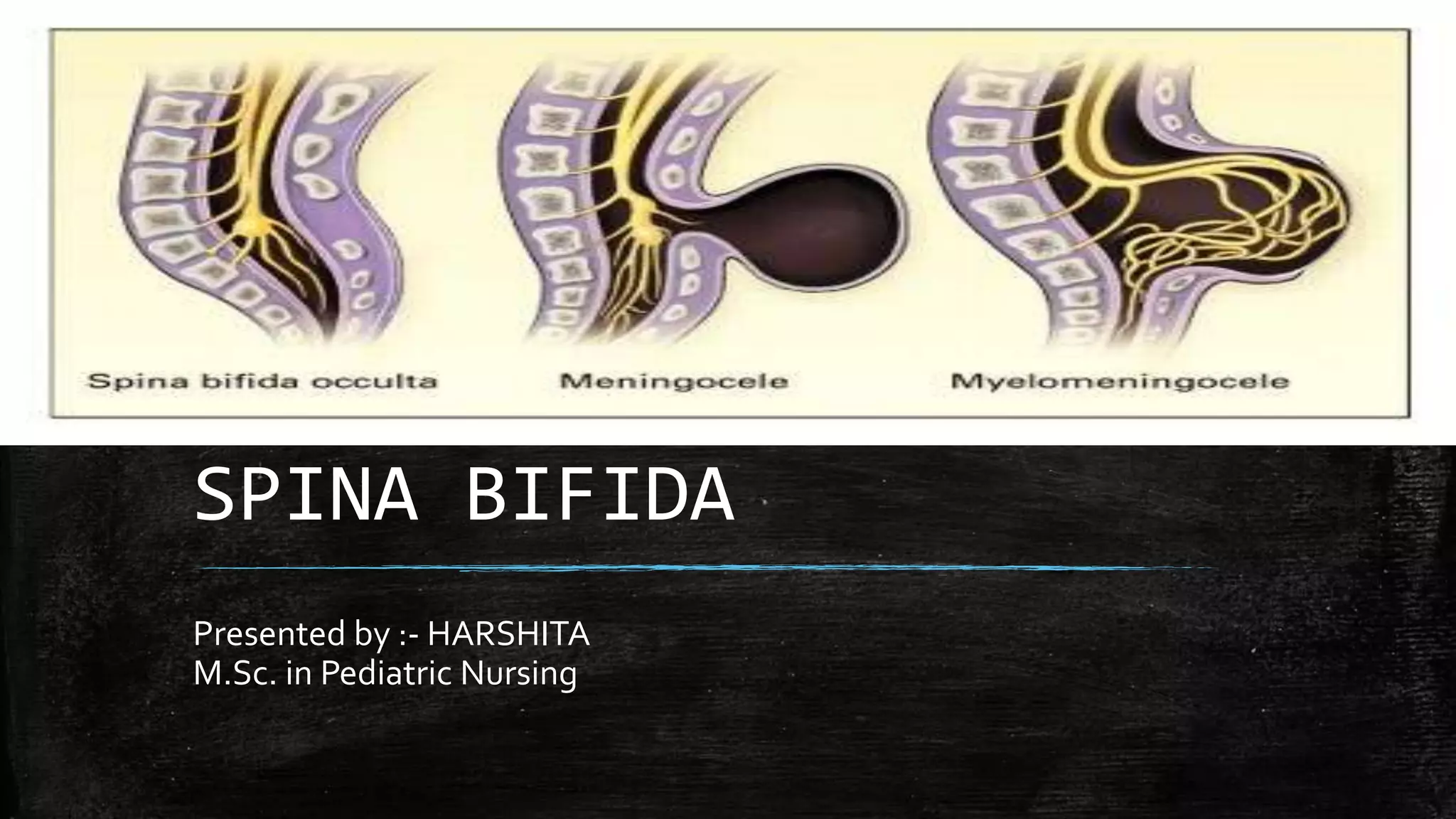
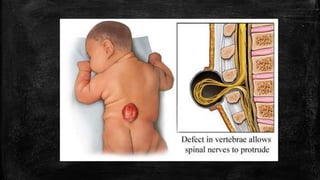
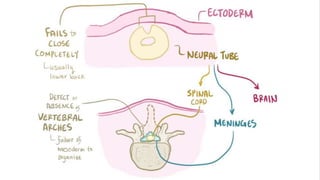
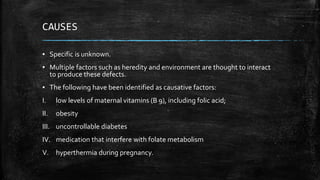
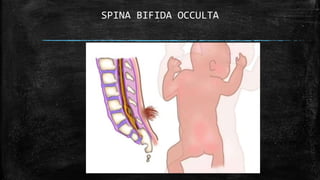
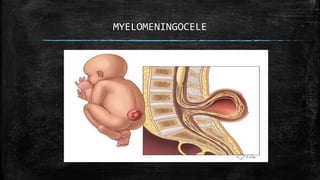
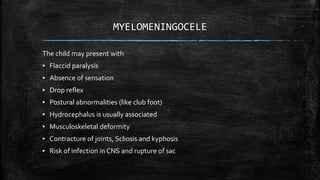
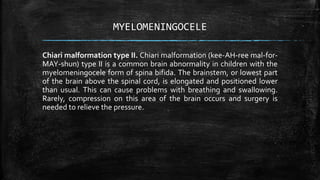
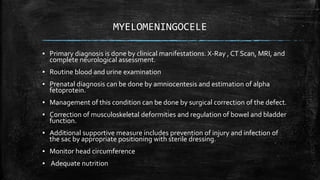
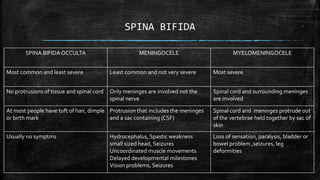
Spina bifida is a neural tube defect characterized by incomplete closure of the backbone and membranes around the spinal cord, resulting in various forms such as occulta, meningocele, and myelomeningocele. Its causes are multifactorial, including genetics and environmental factors like maternal vitamin deficiencies. Management involves surgical correction and long-term care for associated complications like hydrocephalus and musculoskeletal issues.