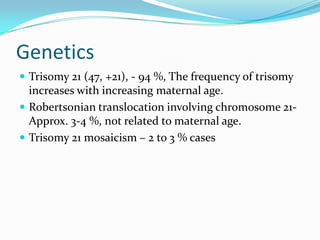
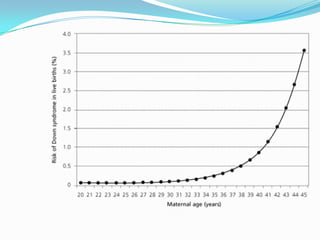
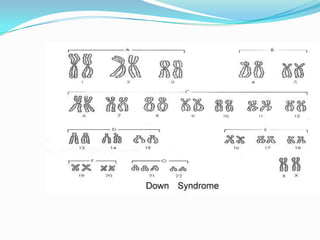
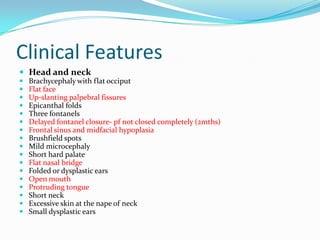
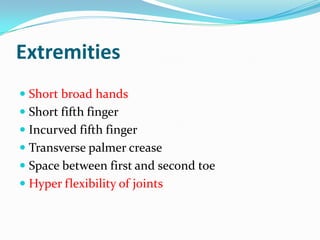
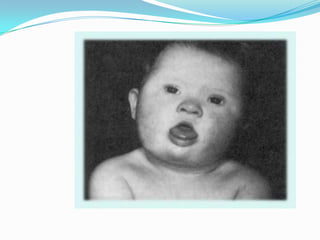
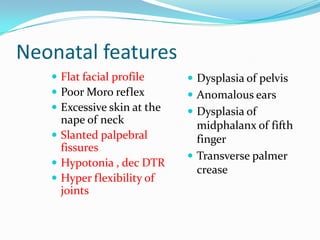
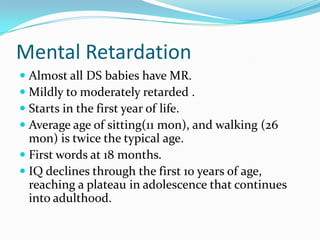
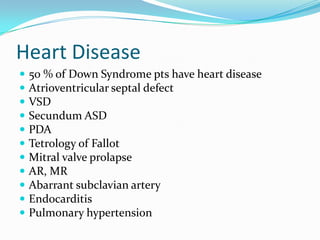
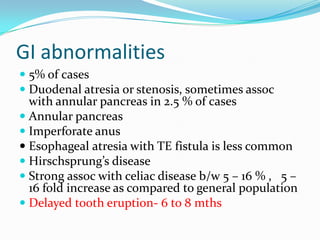
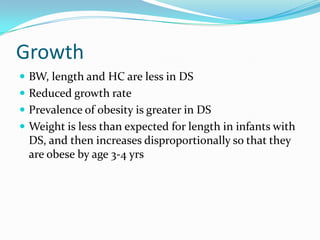
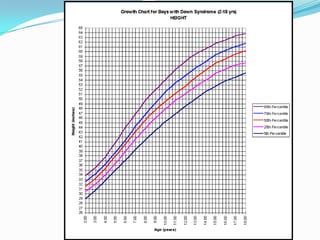
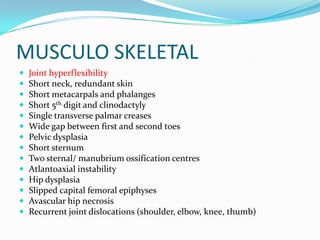
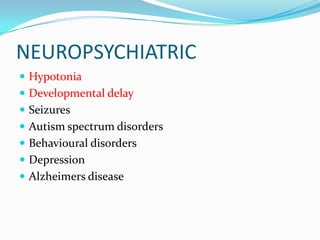
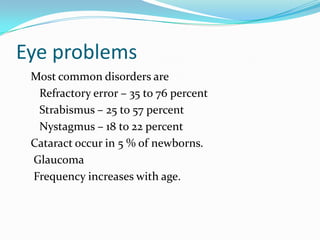
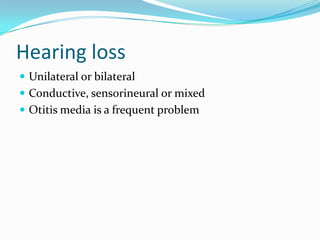
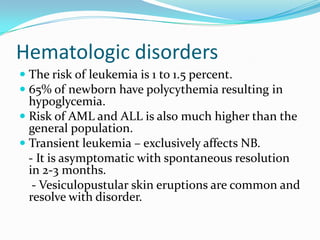
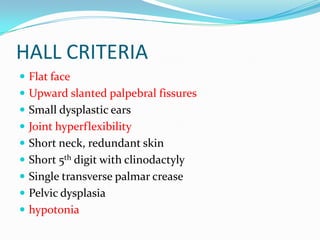
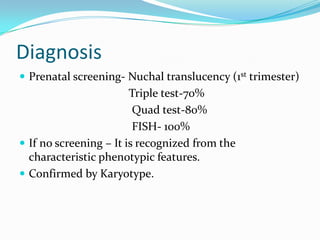
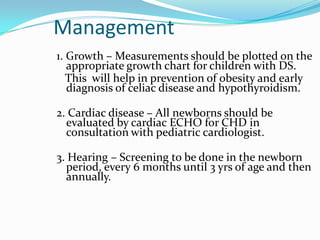
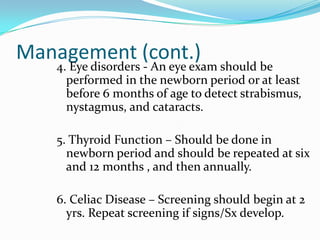
This document provides details on the case of an 8 month old female child named Azma who presented with recurrent cold, cough, loose motions, and rapid breathing. It summarizes her birth history, developmental milestones, family history, clinical features, genetic causes, common health issues, diagnostic criteria, management, and prognosis of Down syndrome.