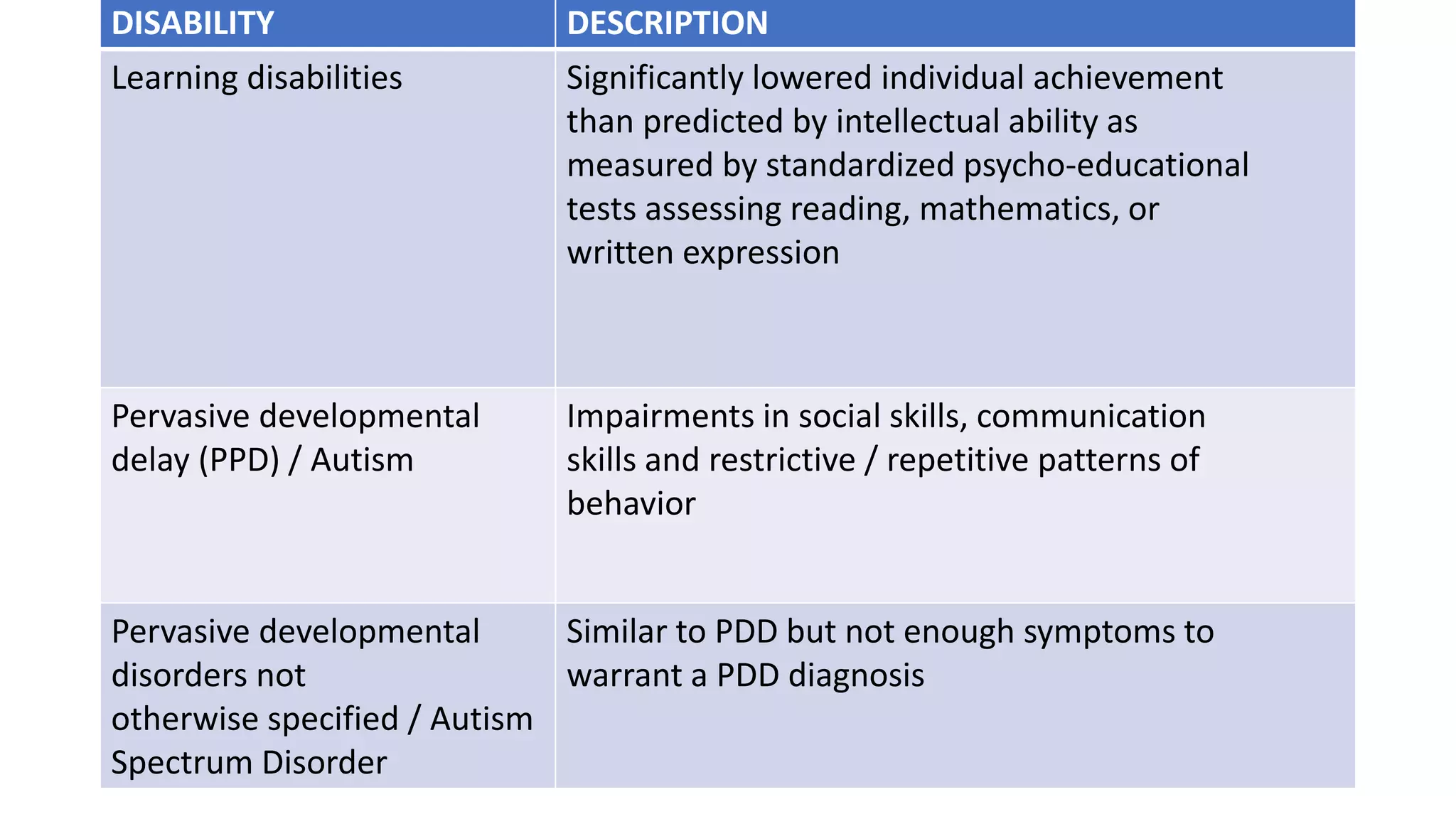
Developmental delay occurs in 5-10% of children and is defined as a child not reaching developmental milestones at the expected age. Developmental assessment involves screening, surveillance, and diagnostic evaluation to identify delays. Physical exam may provide clues to underlying causes, which include genetic syndromes, infections, toxins, and trauma. Investigations help diagnose specific conditions, and management consists of specialized therapies and treatments tailored to each child's needs.