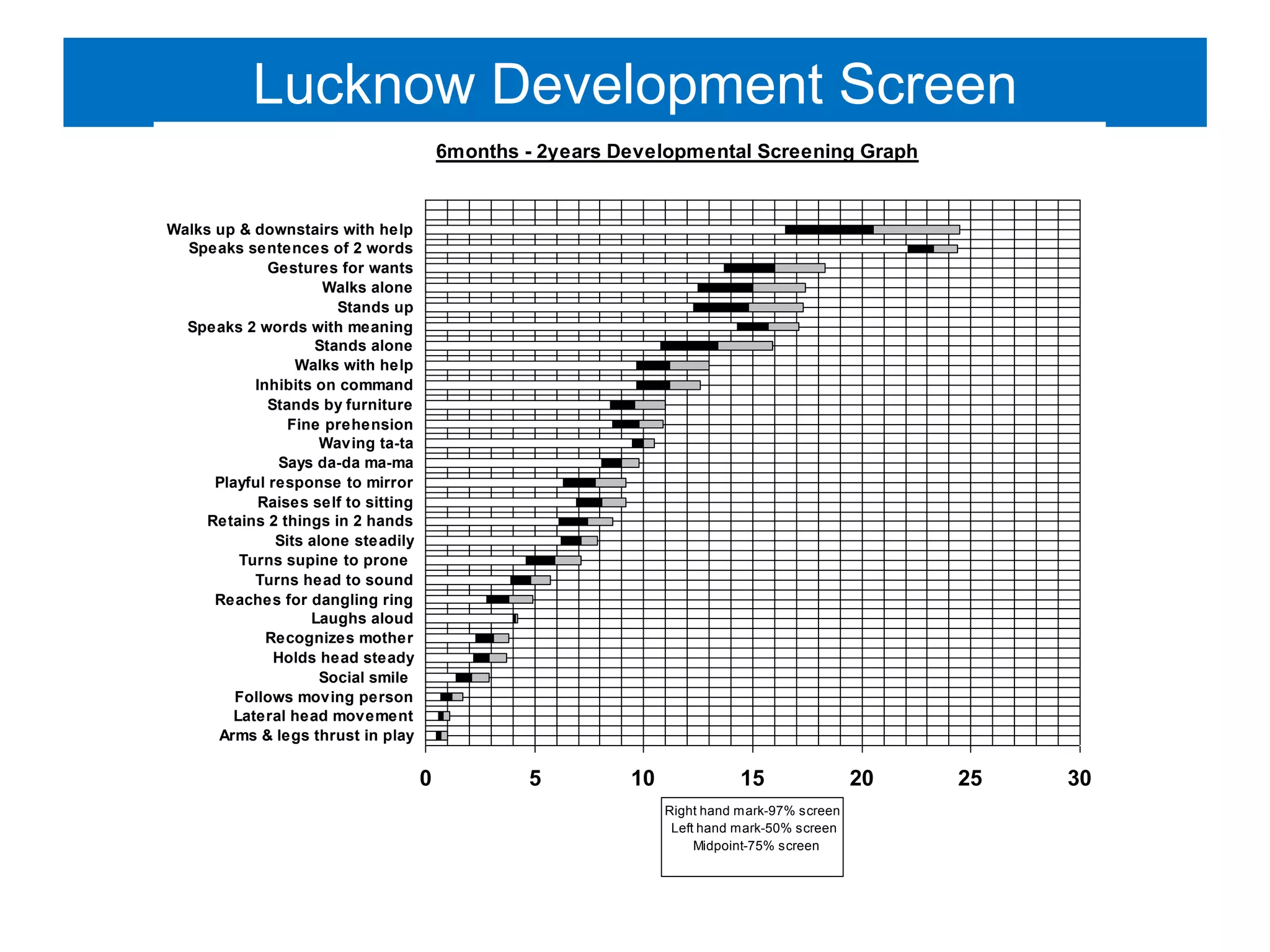
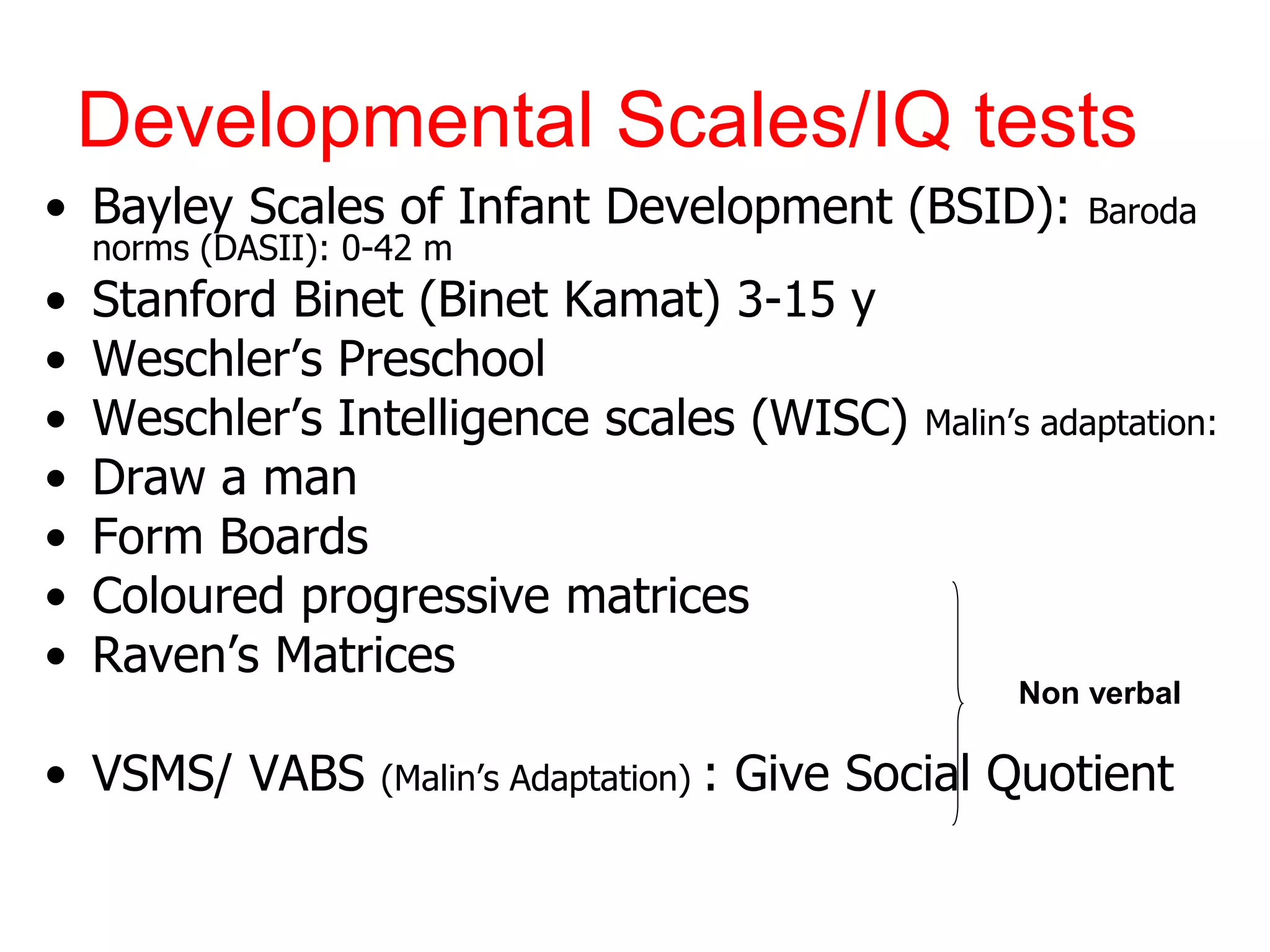
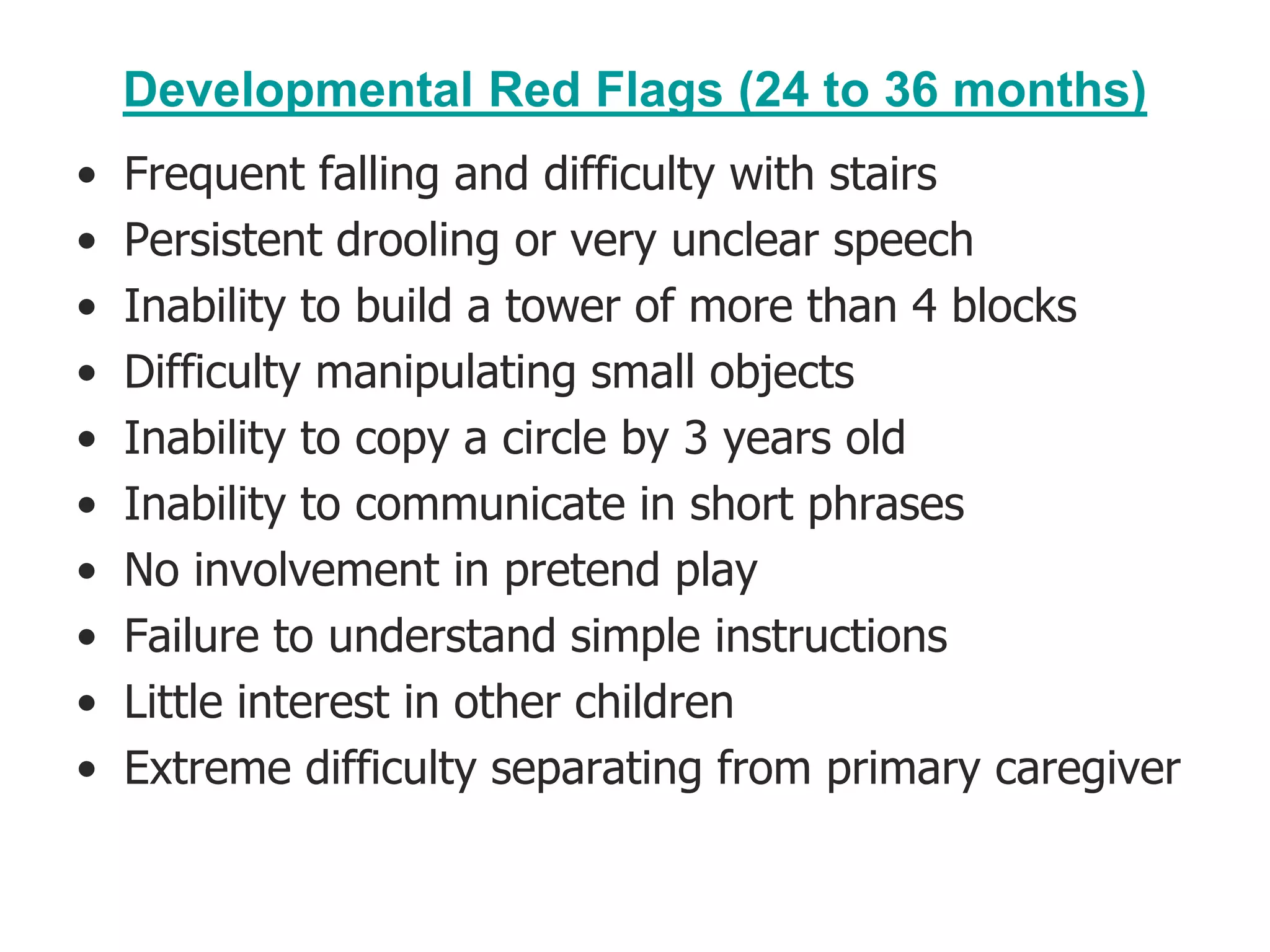
This document discusses the approach to developmental delay. It begins by outlining normal child development and milestones in gross motor, fine motor, language, and social skills. It then describes transient versus persistent developmental delay. Screening tools used in India to identify developmental delay are mentioned. Formal developmental assessments including the Bayley Scales and IQ tests are also discussed. The document provides guidance on evaluating a child with delay, including obtaining a thorough history and physical exam. Key areas to assess and developmental red flags at different ages are outlined.