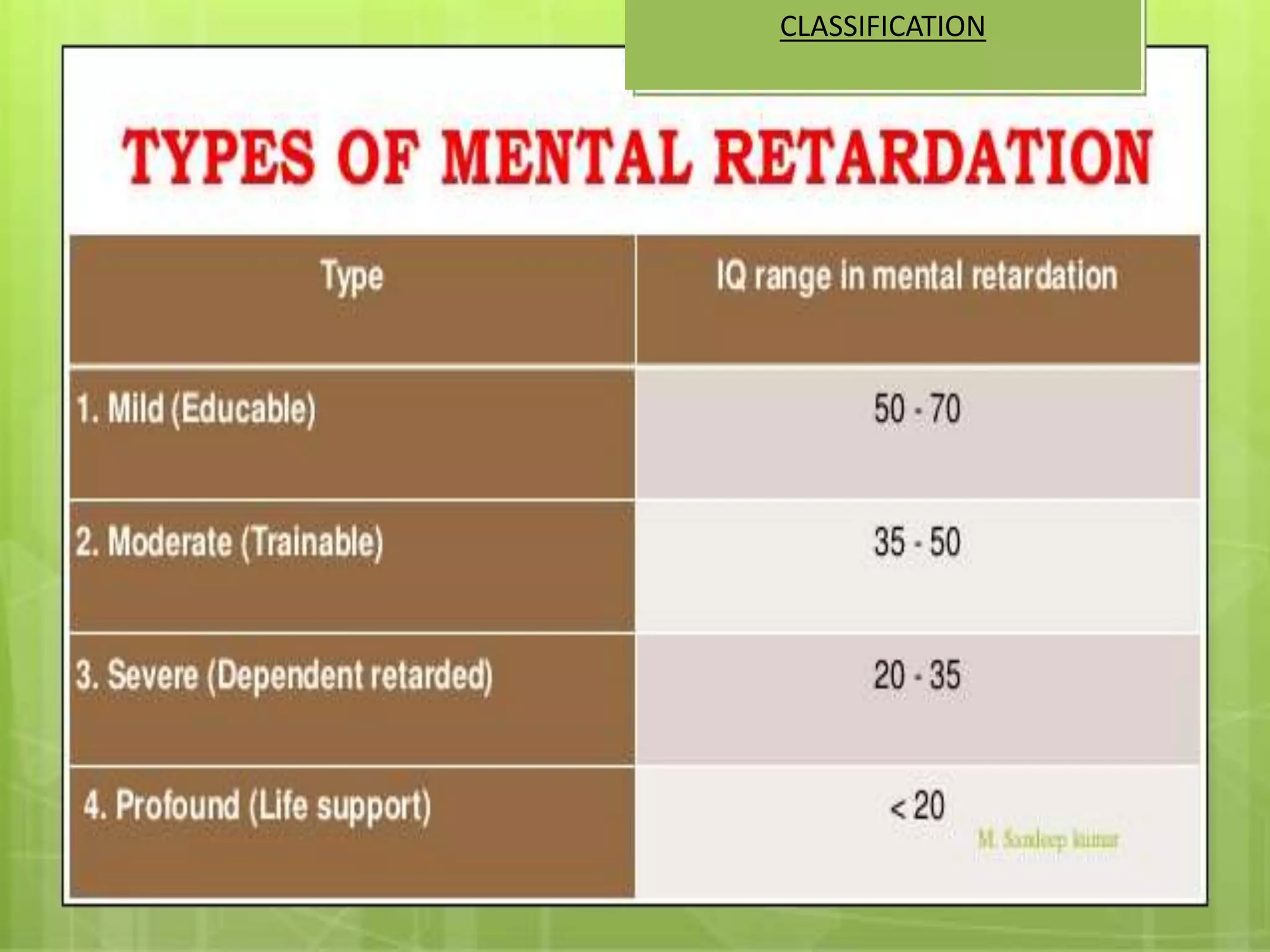
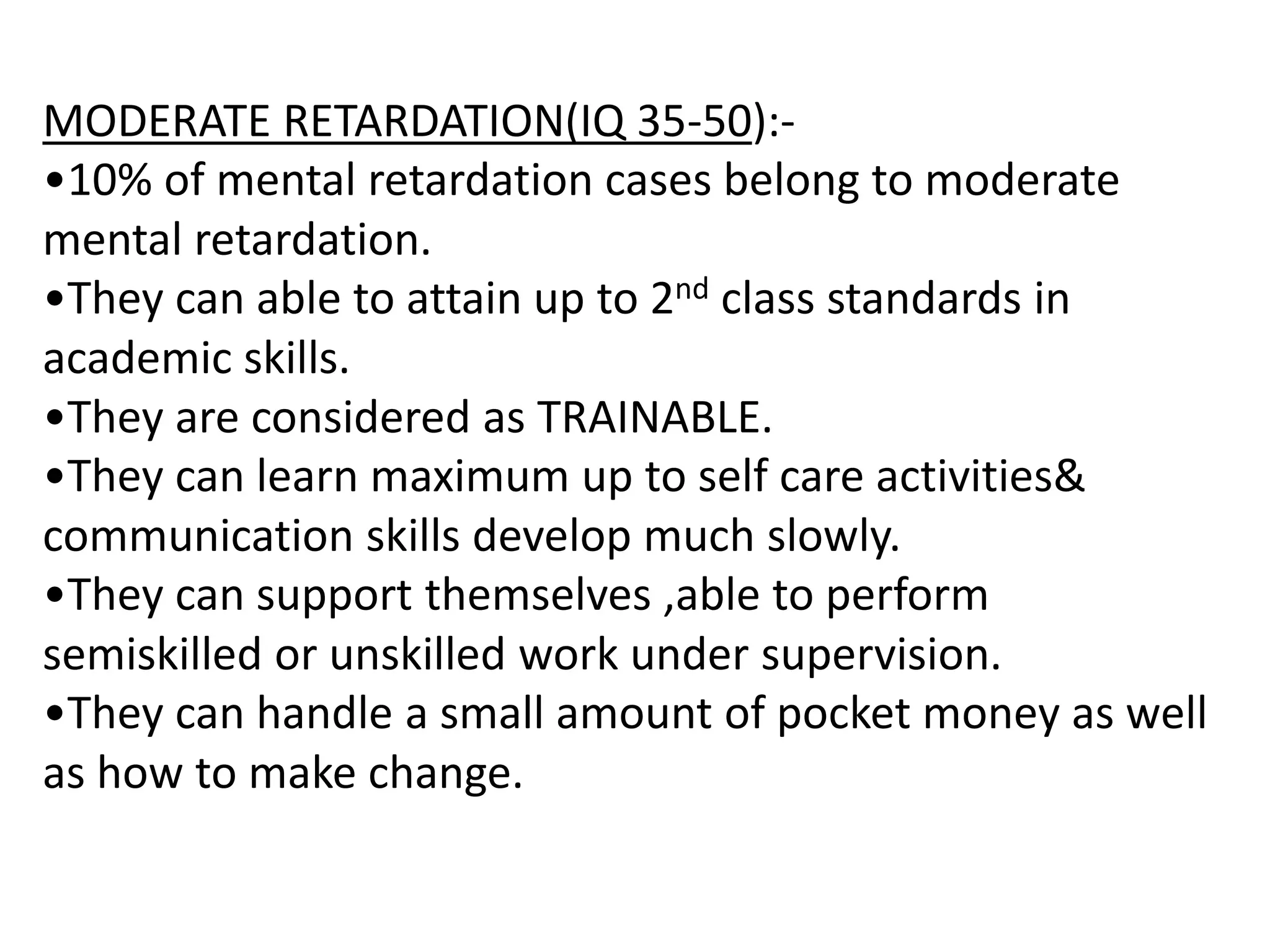
1) The document discusses mentally challenged or mentally retarded children, defining it as significantly sub-average intellectual functioning and impaired adaptive behavior that manifests during development.
2) Causes of mental retardation include genetic factors like chromosomal abnormalities, metabolic disorders, infections during pregnancy, prenatal factors, and environmental factors.
3) Treatment involves behavior management, special education programs, family therapy and rehabilitation services according to the level of impairment. Prevention focuses on preconception counseling, prenatal care, and early detection/treatment of disorders.