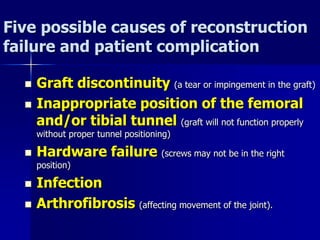
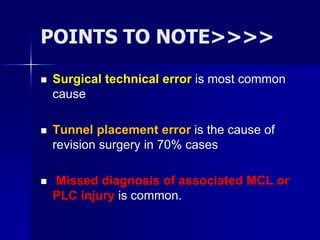
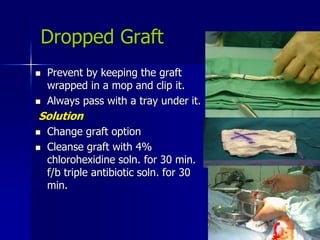
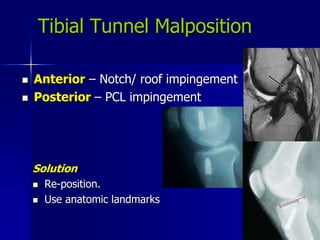
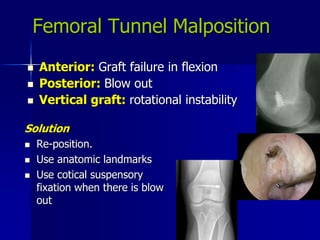
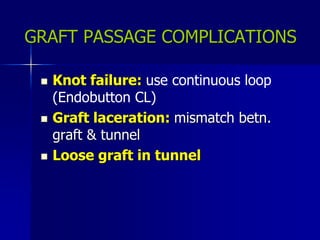
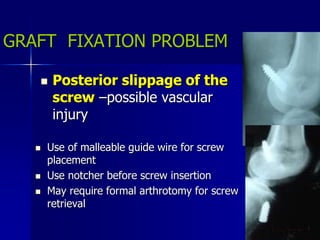
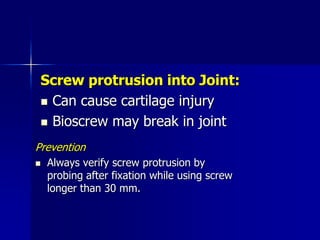
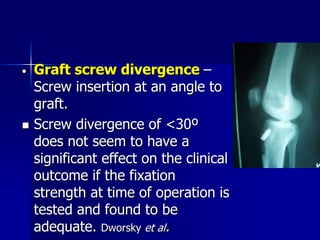
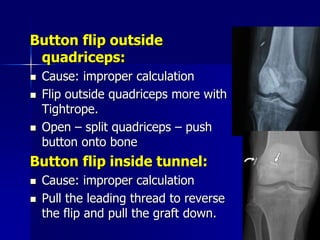
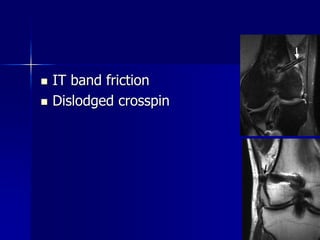
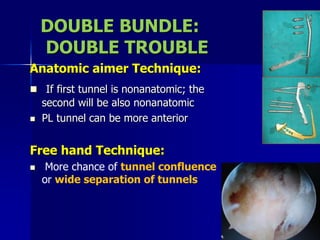
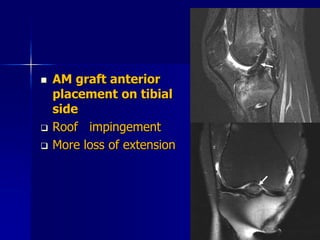
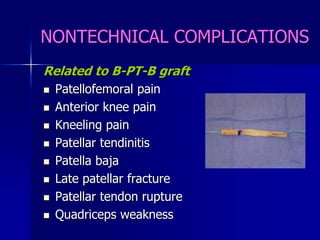
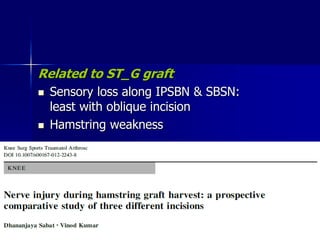
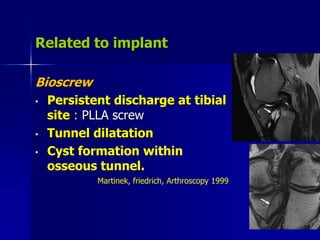
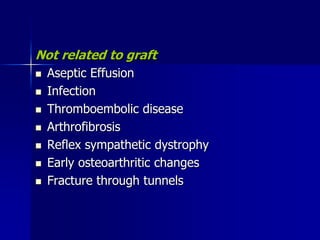
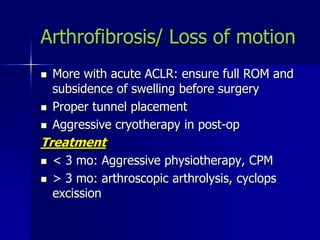
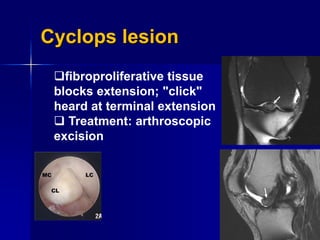
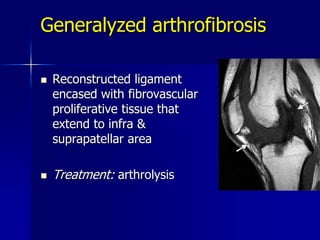
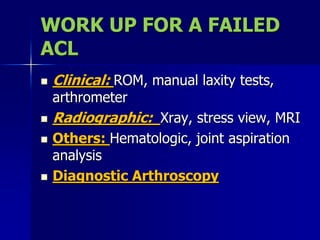
The document discusses potential complications from ACL reconstruction surgery, noting that surgical technical errors during graft harvest, tunnel preparation, or fixation are most common causes of failure. Five possible causes of reconstruction failure are identified as graft discontinuity, inappropriate tunnel positioning, hardware failure, infection, or arthrofibrosis. Proper surgical technique and avoidance of tunnel malpositioning are emphasized to prevent complications.