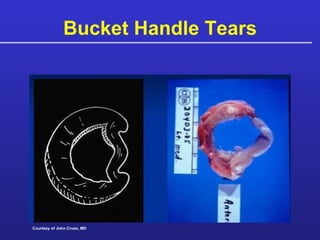
The document discusses meniscus repair, detailing the frequency and implications of meniscal tears, particularly in athletes. It covers diagnostic methods, surgical techniques, and rehabilitation strategies, emphasizing the importance of preserving the meniscus for joint stability and function. Various case studies and research findings are presented to illustrate treatment outcomes and the biomechanics of meniscal injuries.