This document discusses posterolateral corner injuries of the knee. It provides details on the anatomy, mechanisms of injury, clinical evaluation, imaging, and treatment of these injuries. Key points include:
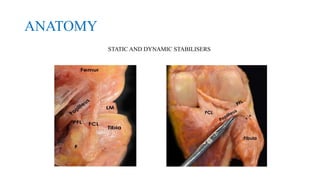
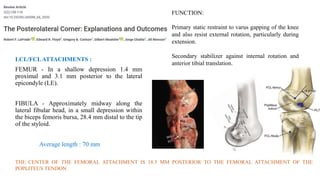
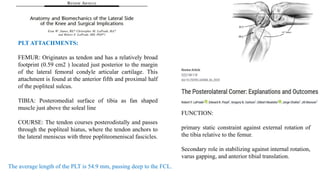
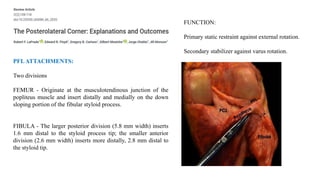
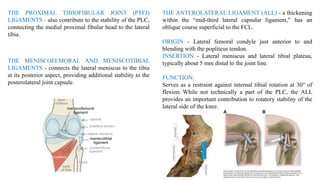
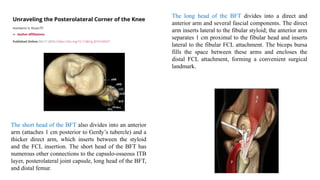
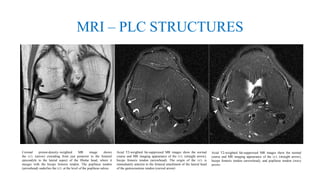
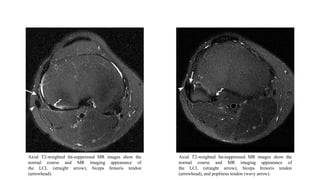
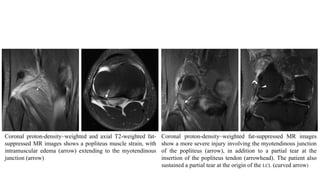
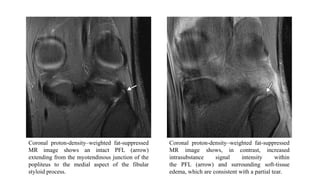
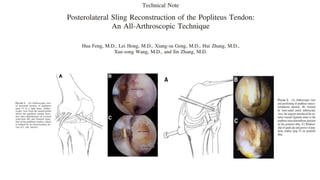
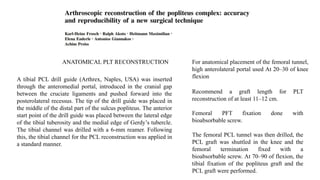
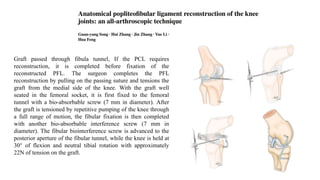
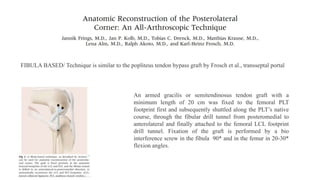
- The posterolateral corner is made up of several static and dynamic stabilizers including the LCL, popliteus tendon, popliteofibular ligament, and biceps femoris tendon.
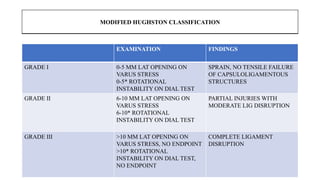
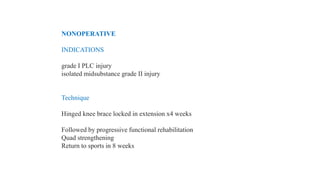
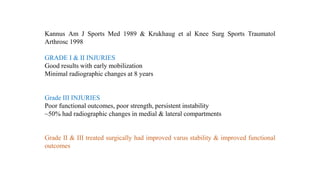
- Injuries can range from grade I sprains to grade III complete ligament disruptions and are often associated with injuries to other knee ligaments.
- Evaluation involves assessing varus and rotational stability along with imaging like MRI to identify injured structures.
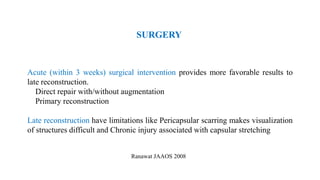
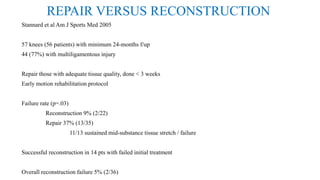
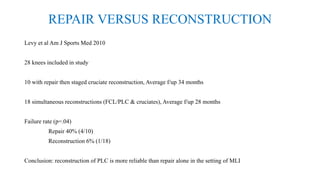
- Treatment ranges from bracing and rehabilitation for