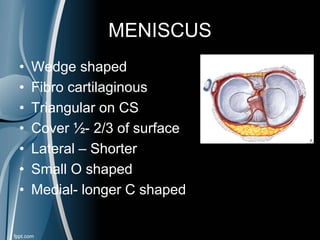
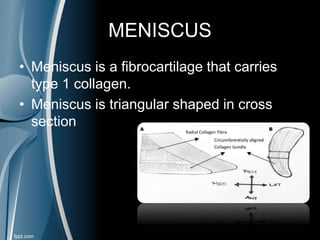
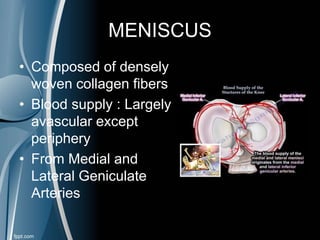
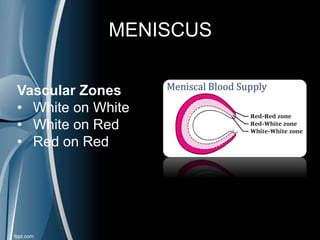
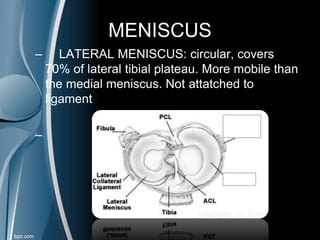
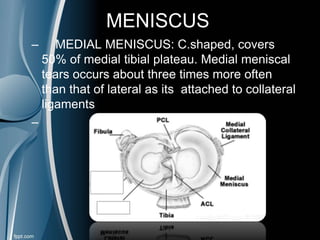
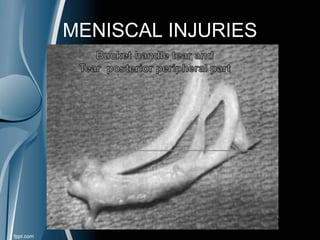
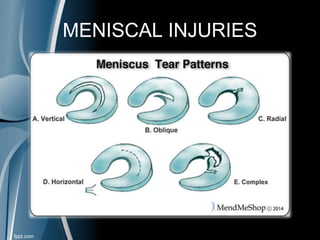
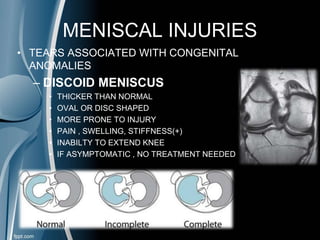
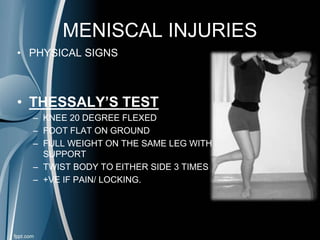
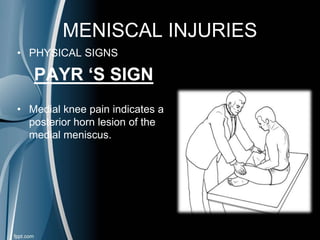
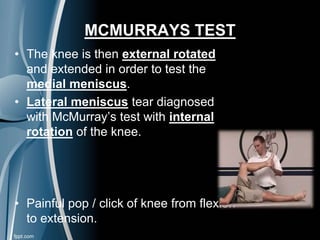
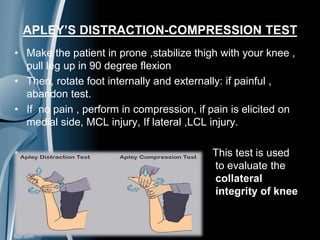
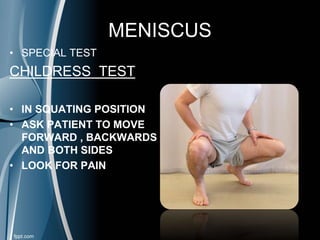
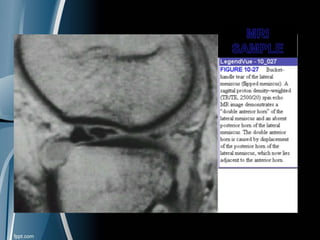
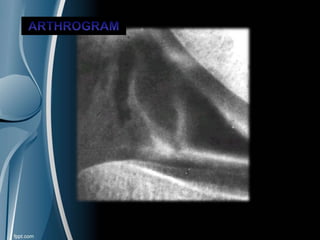
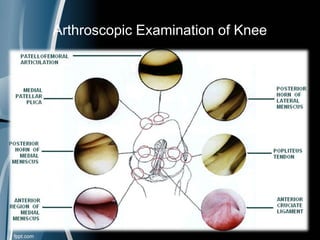
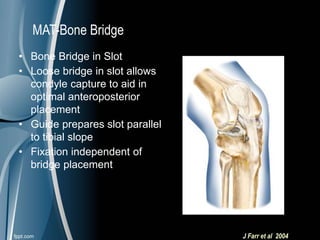
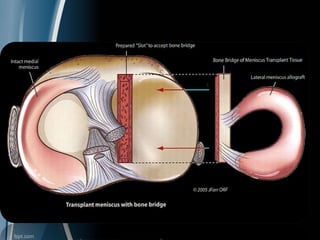
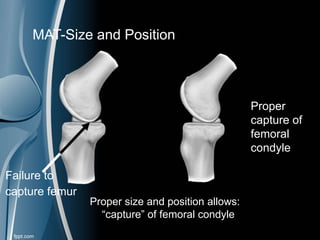
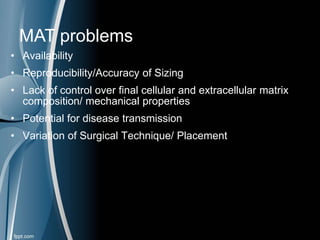
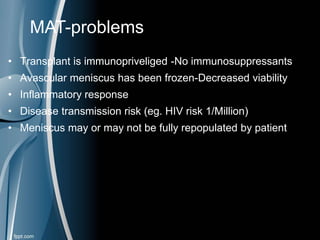
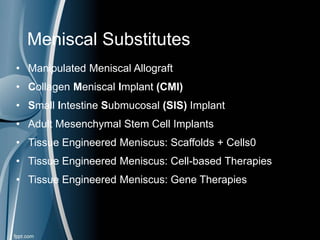
This document discusses meniscal injuries of the knee. It provides information on meniscal anatomy, vascular supply, types of tears including longitudinal, horizontal, and bucket handle tears. It outlines signs and symptoms of meniscal tears including joint line tenderness. Physical exam tests like McMurray's test and MRI are discussed for diagnosis. Treatment options including non-surgical management for small peripheral tears versus surgical options like partial meniscectomy, meniscal repair, and allograft transplantation are summarized. Post-operative rehab and potential complications are also briefly mentioned.