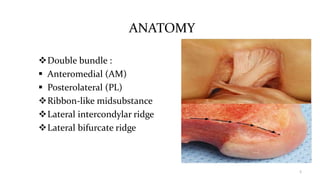
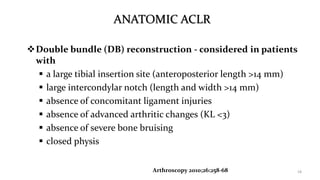
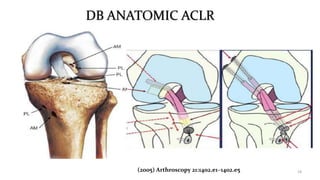
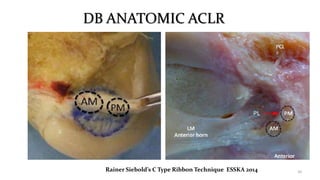
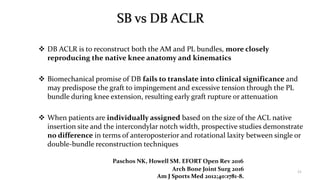
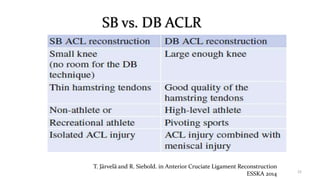
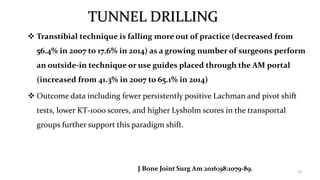
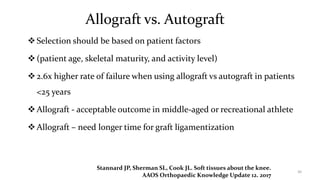
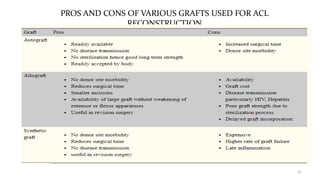
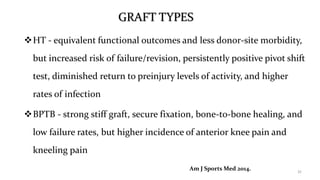
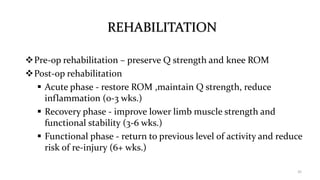
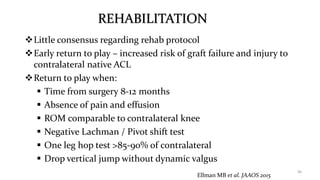
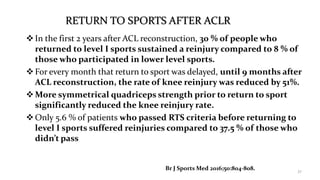
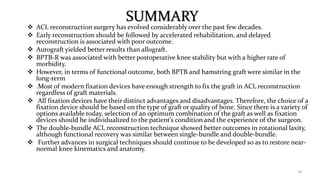
Current trends in ACL surgery include a shift towards anatomical reconstruction techniques that more closely restore the native ACL footprint. While double bundle reconstruction aims to better restore knee rotation, high quality studies show no difference in outcomes compared to single bundle reconstruction. Autograft tissue like hamstring tendon is preferred over allograft for younger patients due to higher failure rates with allograft. Postoperative rehabilitation protocols emphasize early range of motion restoration and return to sport is recommended between 8 to 12 months following surgery accompanied by meeting specific strength and performance benchmarks.