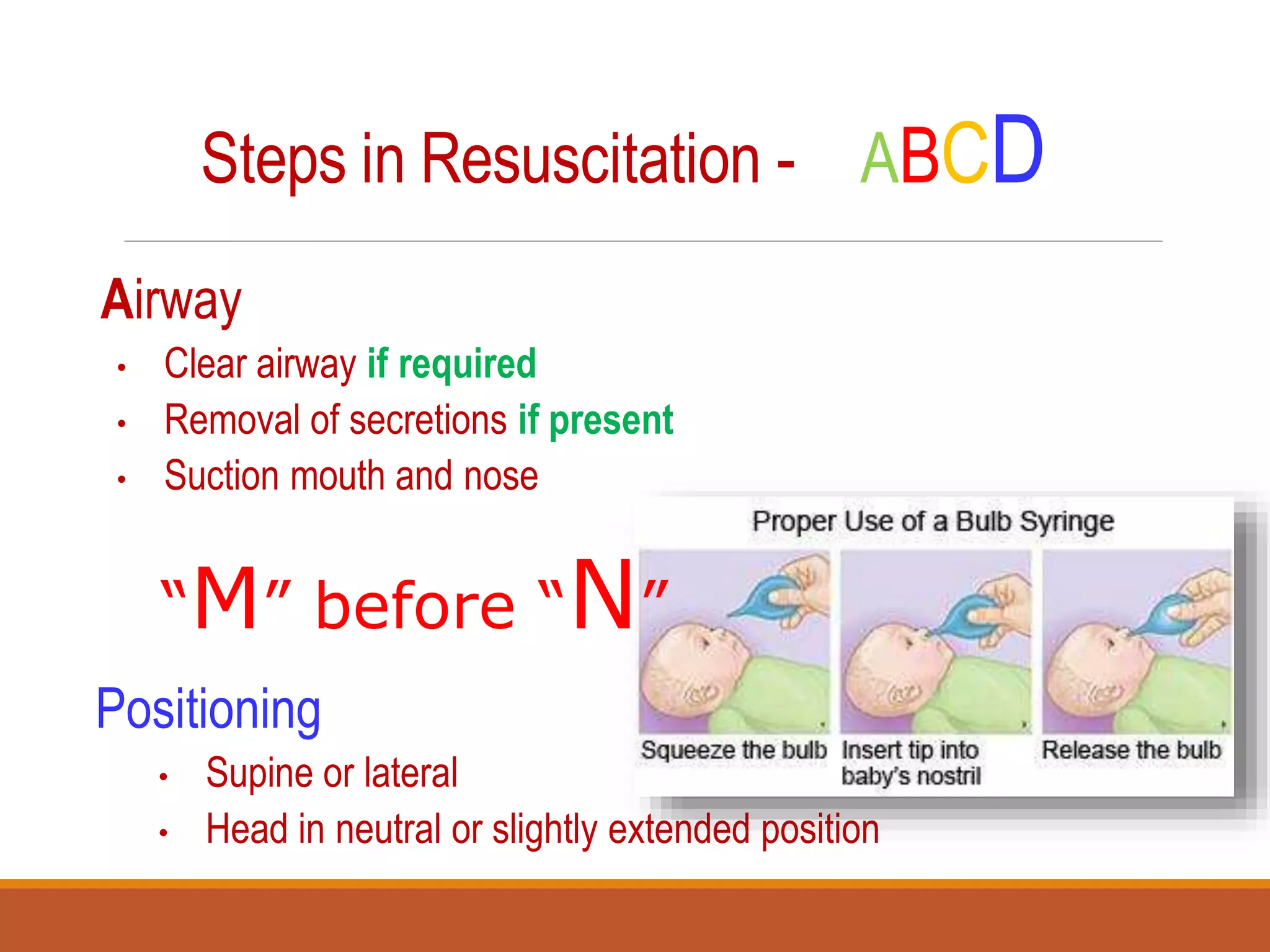
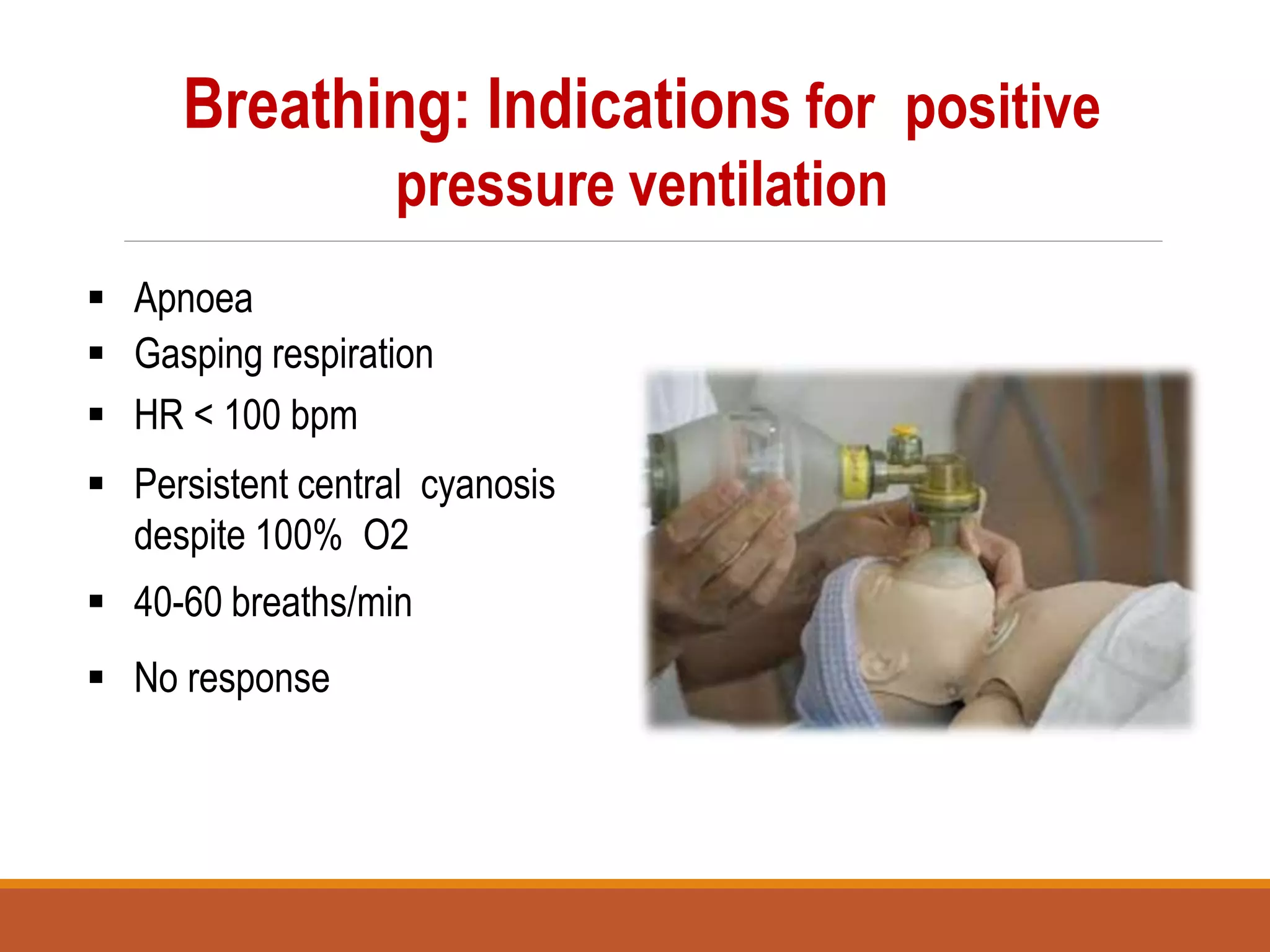
The document discusses the process and techniques of neonatal resuscitation, detailing the physiological changes at birth, causes of neonatal mortality, and APGAR scoring for assessing newborns. It outlines essential equipment and step-by-step procedures for providing appropriate resuscitation measures in compromised infants, emphasizing the importance of early intervention for effective outcomes. It also highlights ethical considerations for discontinuing resuscitation efforts in cases with poor prognostic indicators.